fibroblastbluestack
bluestack 时间:2021-02-20 阅读:()
RESEARCHOpenAccessLipopolysaccharide-inducedblood-brainbarrierdisruption:rolesofcyclooxygenase,oxidativestress,neuroinflammation,andelementsoftheneurovascularunitWilliamA.
Banks1,2*,AliciaM.
Gray3,MichelleA.
Erickson1,2,ThereseS.
Salameh1,MamathaDamodarasamy2,NaderSheibani4,JamesS.
Meabon5,EmilyE.
Wing1,YoichiMorofuji1,2,6,DavidG.
Cook1andMayJ.
Reed2AbstractBackground:Disruptionoftheblood-brainbarrier(BBB)occursinmanydiseasesandisoftenmediatedbyinflammatoryandneuroimmunemechanisms.
InflammationiswellestablishedasacauseofBBBdisruption,butmanymechanisticquestionsremain.
Methods:Weusedlipopolysaccharide(LPS)toinduceinflammationandBBBdisruptioninmice.
BBBdisruptionwasmeasuredusing14C-sucroseandradioactivelylabeledalbumin.
Braincytokineresponsesweremeasuredusingmultiplextechnologyanddependenceoncyclooxygenase(COX)andoxidativestressdeterminedbytreatmentswithindomethacinandN-acetylcysteine.
Astrocyteandmicroglia/macrophageresponsesweremeasuredusingbrainimmunohistochemistry.
InvitrostudiesusedTranswellculturesofprimarybrainendothelialcellsco-ortri-culturedwithastrocytesandpericytestomeasureeffectsofLPSontransendothelialelectricalresistance(TEER),cellulardistributionoftightjunctionproteins,andpermeabilityto14C-sucroseandradioactivealbumin.
Results:IncomparisontoLPS-inducedweightloss,theBBBwasrelativelyresistanttoLPS-induceddisruption.
DisruptionoccurredonlywiththehighestdoseofLPSandwasmostevidentinthefrontalcortex,thalamus,pons-medulla,andcerebellumwithnodisruptioninthehypothalamus.
TheinvitroandinvivopatternsofLPS-induceddisruptionasmeasuredwith14C-sucrose,radioactivealbumin,andTEERsuggestedinvolvementofbothparacellularandtranscytoticpathways.
Disruptionasmeasuredwithalbuminand14C-sucrose,butnotTEER,wasblockedbyindomethacin.
N-acetylcysteinedidnotaffectdisruption.
Invivo,themeasuresofneuroinflammationinducedbyLPSweremainlynotreversedbyindomethacin.
Invitro,theeffectsonLPSandindomethacinwerenotalteredwhenbrainendothelialcells(BECs)wereculturedwithastrocytesorpericytes.
Conclusions:TheBBBisrelativelyresistanttoLPS-induceddisruptionwithsomebrainregionsmorevulnerablethanothers.
LPS-induceddisruptionappearsistobedependentonCOXbutnotonoxidativestress.
Basedoninvivoandinvitromeasuresofneuroinflammation,itappearsthatastrocytes,microglia/macrophages,andpericytesplaylittleroleintheLPS-mediateddisruptionoftheBBB.
Keywords:Blood-brainbarrier,Neurovascularunit,Neuroinflammation,Brainendothelialcells,Indomethacin,Lipopolysaccharide*Correspondence:wabanks1@uw.
edu1GeriatricResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA2DivisionofGerontologyandGeriatricMedicine,DepartmentofInternalMedicine,UniversityofWashingtonSchoolofMedicine,Seattle,WA,USAFulllistofauthorinformationisavailableattheendofthearticle2015Banksetal.
OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Banksetal.
JournalofNeuroinflammation(2015)12:223DOI10.
1186/s12974-015-0434-1BackgroundThevascularblood-brainbarrier(BBB)protectsthecentralnervoussystemfromblood-bornesubstancesthatareotherwiseneurotoxic.
InflammationhaslongbeenknowntodisrupttheBBB.
Skoogin1937foundthatanallergicreactioncoulddisrupttheBBB[1].
Meningitis,encephalitis,sepsis,andlocalandsystemicinfectionshavebeenassociatedwithalteredpermeabilityoftheBBBtomanysubstancesandimmunecells[2].
Eckmanetal.
asearlyas1958andAllenafewyearslatershowedthatgram-negativeendotoxinwasassociatedwithBBBdisruption[3,4].
Gram-negativeendotoxininitsmorepurifiedformoflipopolysaccharide(LPS)isknowntodisrupttheBBBandalsoaltersmanyotheraspectsofBBBfunc-tion,includingadsorptivetranscytosis,immunecelltrafficking,andvarioustransportfunctions[5–9].
Morerecently,anumberofdiseasesthatincludemultiplesclerosis,Alzheimer'sdisease,diabetesmel-litus,obesity,andstrokehavebeenassociatedwithbothinflammationandBBBdisruption[10–14].
Thebarrierfunctionsofthecapillarybedofthebrainareknowntoarisefromthreemodifications:thepresenceoftightjunctionsbetweenendothelialcells,anearabsenceofmacropinocytosis,andlossoffenestrae[15,16].
Together,thesethreemodifica-tionspreventtheproductionofanultrafiltratebythebrain'scapillarybed.
InflammationcaninduceBBBdisruptionbyalteringtightjunctionfunction,thuspromotingparacellularleakage,andre-inducingvesicularprocesses,thuspromotingtranscytoticleak-age.
Insomecauses,transcytoticmechanismsmaybethedominantformofBBBdisruption[17,18]andmayprecedeparacellularopening[19,20].
MechanismsbywhichLPSaffectsBBBfunctionarenotwellunderstood.
Thecyclooxygenase(COX)inhibitorindomethacinreversessomeLPS-induceddysfunctionsoftheBBB,includinginvitrodisrup-tion[21,22]andinvivoimpairedamyloidbetapeptideefflux[23].
However,indomethacinhasnoeffectonLPS-inducedinhibitionofP-glycoproteinactivity[24].
TheantioxidantN-acetylcysteine(NAC)protectsthebrainendothelialcell(BEC)fromoxida-tivestressinducedbymethamphetamineandanti-retroviraldrugs[25,26]andreversesthedecreasedbrain-to-bloodtransportofamyloidbetapeptideinducedbyLPS[27].
TheeffectofNAConLPS-inducedBBBdisruptionhasnotbeenexaminedinvivo.
Here,wefurtherexaminedthemechanismsbywhichLPSinducesBBBdisruptionbothinvivoandinvitrobyinvestigatingbraincytokines,prostaglan-dininhibition,oxidativestress,andastrocyteandmicroglialactivation.
MethodsAnimalsAllmiceweretreatedinaccordancewithNIHGuidelinesfortheCareandUseofLaboratoryAnimalsinanAAALAC-accreditedfacilityandapprovedbytheInstitu-tionalAnimalCareandUseCommitteeoftheVAPugetSoundHealthCareSystem.
MaleCD-1miceat6–8weeksofagewerepurchasedfromCharlesRiverandkeptona12/12-hlight/darkcyclewithadlibitumfoodandwater.
RadioactiveprobesSucroselabeledwith14CwaspurchasedfromPerkin-Elmer(Waltham,MA).
Bovineserumalbumin(BSA)waslabeledwith125Ibythechloramine-Tmethod,andtheresultingradioactivealbumin(iodine-labeledalbumin(I-Alb))waspurifiedonaG-10Sephadexcolumn.
BSAwaslabeledwith99mTc(technetium-labeledalbumin(Tc-Alb))andpurifiedonaG-10Sephadexcolumn.
Lipopolysaccharide(LPS)doseresponseandtimestudiesMaleCD-1miceaged6–10weekswereweighedandgivenanintraperitoneal(IP)injectionof0.
03,0.
3,or3mg/kgLPSfromSalmonellatyphimurium(SigmaAldrich,St.
Louis,MO,USA)dissolvedinsterilenormalsaline.
Micewerereweighedabout23haftertheLPSinjection,anesthetizedwithurethane,andthejugularveinsexposed.
Themiceweregivenanivinjectionof14C-sucrose(106dpmin0.
2mloflactatedRinger'ssolutionwith1%BSA)24h±20minaftertheLPSinjection.
Arterialbloodwascollectedfromacutinthedescendingabdominalaorta.
Thevascularspaceofthebrainwaswashedfreeofbloodbyopeningthethorax,clampingthedescendingthoracicaorta,severingbothjugularveins,andperfusing20mloflactatedRinger'ssolutionthroughtheleftventricleoftheheartinlessthan1min.
Afterwashout,themousewasimmediatelydecapitatedandthewholebrainwasremovedandweighed.
Serumwasobtainedbycentrifugingthecarotidarterybloodfor10minat4000*g.
Thebrainsweresolu-bilized,andthelevelofradioactivityinthebrainsandseraweredeterminedinabetacounter.
Asubsetofmicethatreceived3mg/kgofLPSwasstudiedfor14C-sucrosepermeation4haftertheLPSinjection.
Anothersubsetofmicethatwerestudiedfor14C-sucrosepermeation24hafterreceiving3mg/kgofLPShadtheirbrainsdissectedintotheolfactorybulb,frontalcortex,parietalcortex,occipitalcortex,striatum,hippocampus,hypothalamus,thalamus,cerebellum,pons-medulla,andmidbrain.
OthermicereceivedaninjectionofI-Albinsteadof14C-sucrose,butwereotherwisetreatedthesame,receiving3mg/kgofLPSandbeingstudiedat24h.
Levelsofradioactivityintheserumandbrainweredeterminedinagammacounter.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page2of15Resultswerecalculatedbydividingthecountspermi-nuteperbrainorbrainregionbythecountsperminutepermicroliterinthecorrespondingserumandbytheweightofthebrainorbrainregion.
Theresultswerethusexpressedasmicroliterspergramofbraintissue.
Bloodlevelswerecalculatedasthepercentoftheinjecteddosepresentpermilliliterofserum(%injec-tion/ml)bydividingthecountsperminutepermilliliterbythecpminjectedivandmultiplyingby100.
AdministrationofNACorindomethacinIntheNACstudy,maleCD-1micewereassignedtooneoffourgroups.
Allmicereceivedinjectionsof100μlofsalineat30min,0,6,and24h.
Ingroups1and3,the30-mininjectionwassaline,andingroups2and4,itwassalinecontainingNAC(100mg/kg;SigmaAldrich,St.
Louis,MO).
Ingroups1and2,theremaininginjections(0,6,24h)weresaline,whereasingroups3and4,thesalinevehiclecontainedLPS(3mg/kg).
Fourhoursafterthelastinjection,micereceivedaninjectionof106cpmof14C-sucroseandwerestudiedasdescribedabove.
Indomethacin(5mg/kg)wasstudiedinthesamedesignusingitinplaceofNAC.
Forthefirstinjection,7%NaHCO3wasusedasthevehicleinsteadofsaline.
CytokinemeasurementsWholebrainlysatesfrommicetreatedwiththethree-injectionregimenofLPSdescribedaboveweregentlyhomogenizedin150μlofNP40buffer(Invi-trogen,GrandIsland,NY).
Sampleswerecentrifugedfor5minat4°Cand12,000*g.
ProteincontentofthesupernatantwasthendeterminedaccordingtotheBCAassayprotocolsuppliedbythemanufac-turer.
Proteinconcentrationsareattached.
Apanelof23cytokines(interleukin(IL)-1α;IL-1β;IL-2;IL-3;IL-4;IL-5;IL-6;IL-9;IL-10;IL-12(p40);IL-12(p70);IL-13;IL-17;eotaxin(CCL11);granulocytecolony-stimulatingfactor(G-CSF);granulocyte-macrophagecolony-stimulatingfactor(GM-CSF);interferon(IFN)-γ;keratinocytechemoattractant(KC)(CXCL1);monocytechemoattract-antprotein(MCP)-1(CCL2);macrophageinflammatoryprotein(MIP)-1α(CCL3);MIP-1β(CCL4);regulatedonactivation,normalTcellexpressedandsecreted(RANTES;CCL5)andtumornecrosisfactor(TNF)-α)weremeasuredinwholebrainlysatesusingamurineBio-PlexProassaykit(Bio-RadLaboratories,Inc.
;Hercules,CA).
Allsampleswerediluted1:3insampledi-luentprovidedinthekitandprocessedaccordingtothemanufacturer'sprotocol.
PlateswerereadonaBio-Plex200(Bio-RadLaboratories,Inc.
;Hercules,CA).
ImmunohistochemistryControlmiceormicetreatedwiththeLPS±indometh-acinregimendescribedabovewereeuthanized,andtheirbrainsremovedandfixedin10%neutral-bufferedformalin,paraffin-embedded,andsectionedat5μm.
Sectionswerede-paraffinized,blockedin2%goatserum,andexposedto2–5μg/mlofmouseanti-F4/80(Serotec)orrabbitanti-Iba1(Wako).
SectionswerethenrinsedinTris-bufferedsalineandexposedto5μg/mlofbiotinylatedanti-mouseoranti-rabbitIgGandthentoVectastainavidin-biotincomplex(ABC)kit(Vector)inconjunctionwith3,3′-diaminobenzidine(DAB,Vector)toderiveaninsolublestainthatcouldbequantified.
Forquantification,aminimumoftwodigitalimagespermousecerebralcortexweretakenat*20magnifica-tion.
TheimageswereprocessedinImageJ,andthebrightnessandcontrastadjustedbeforeconvertingtoanRGBstackimage.
ThethresholdofthebluestackimageisadjusteduntilthestainedtissueshowsoptimalcontrastwithhighlightingoftheDABstaininred.
Thestainingareaanddensityweremeasured,andtheresultwasexpressedasanareafraction,whichisthepercentoftheenclosedareathatishighlightedinred.
Relativestainingintensitywasthencalculatedforthecerebralcorticesforeachgroupofmice.
WesternblottingforZO-1Individualbrainextractsofequivalenttotalproteincontentwereresolvedbysodiumdodecylsulfate-polyacrylamidegelelectrophoresis(SDS-PAGE)(50μgtotalprotein/lane)underreducingconditions,trans-ferredtonitrocellulose,andprobedwith1μg/mlofrabbitpolyclonalantibodiestoZO-1(Invitrogen).
Blotswerethenprobedwithanti-rabbithorseradishperoxidase-conjugatedsecondaryantibody(JacksonImmunoResearch,WestGrove,PA)(1μg/ml)andvisual-izedbyenhancedchemiluminescence(GEHealthcareLifeSciences,Piscataway,NJ).
DensitiesofthebandswerequantifiedusingImageJ.
Isolationofprimarybrainmicrovascularendothelialcells(BMECs)Primarybrainmicrovascularendothelialcells(BMECs)wereisolatedfrom8-week-oldCD-1miceaccordingtoexistingprotocols[28,29]withsomemodifications.
BMECswereculturedinBMECmedium,consistingofDulbecco'smodifiedEagle'smedium(DMEM)/F12supplementedwith20%plasma-derivedfetalbovineserum(AnimalTechnologies),1%GlutaMAX(LifeTechnologies),basicfibroblastgrowthfactor(bFGF,1ng/ml;RocheLifeSciences),heparin(100μg/ml),insulin(5μg/ml),transferrin(5μg/ml),selenium(5ng/ml)(insulin-transferrin-seleniummediumsupplement;LifeTechnologies),andgentamicin(50μg/ml;SigmaAldrich).
Puromycin(4μg/ml;SigmaAldrich)isaddedtotheBMECmediumforthefirst48hafterplatingtoremovepericytesandincreaseendothelialcellpurity[30].
CulturesBanksetal.
JournalofNeuroinflammation(2015)12:223Page3of15weremaintainedat37°Cinahumidifiedatmosphereof5%CO2/95%air.
Themediumischanged24hafterplatingtoremovenon-adheringcells,redbloodcells,anddebris.
At48hafterplating,themediumwaschangedagainwithanewmediumcontainingallthecomponentslistedabove,exceptpuromycin.
ThepurifiedprimaryBMECswereusedtoconstructinvitromodelswhen80%confluent,typicallythe5thdayafterisolation.
ImmortalizedmousebrainpericytesImmortalizedmousebrainpericytes(ImPCs)werepre-paredaspreviouslydescribed[31].
ImPCsweregrownonuncoatedflasksinlow-glucoseDMEMsupplementedwith2mML-glutamine,10%fetalcalfserum,1%non-essentialaminoacids(LifeTechnologies),andinterferongamma(5.
6ng/ml).
ImPCshavebeenpreviouslycharacterized[31]andstainpositivelyforα-smoothmuscleactin,CD-13,andplatelet-derivedgrowthfactorreceptorβandwerenegativeforfactorVIII.
ImPCswereusedatpassages13–15.
IsolationofprimaryastrocytesMousecerebralastrocyteswereobtainedfromneonatalCD-1mice.
Themeningeswerecarefullyremovedfromcorticesusingadissectingmicroscope.
Then,thecleanedcorticesweremechanicallydissociatedinastrocyteculturemedium.
Astrocytesweregrownonpoly-L-lysine-coated24-wellplatesinhighglucoseDMEM(LifeTechnologies)supplementedwith10%fetalbovineserum.
Constructionofinvitroblood-brainbarriermodelBMECswereculturedalone(monocultures),co-culturedwitheitherpericytesorastrocytes,ortri-culturedwithpericytesandastrocytesaccordingtopreviouslypub-lishedmethods[32].
Thetriple-culturemethodwasadjustedforco-cultureandendothelialcellmonoculturevariants.
Inbrief,immortalizedpericytes(5000cells/well),ifpresent,wereseededonthebottomofapolyes-terTranswellinsert(0.
33cm2,0.
4-μmporesize;CorningInc.
)andallowedtoadherefor4h.
EndothelialcellswerebrieflytrypsinizedandseededontheinsideoftheTranswellinsert,whichwascoatedwithfibronectinandcollagentypeIV(0.
1mg/ml,each),atadensityof4*104cellsperwell.
Theinsertswerethenplacedina24-wellplatecontainingprimaryastrocytes.
Themediumusedtoplatethecellsinthe24-wellTranswellscontainedallthecomponentsoftheBMECmedium,listedabove,withtheadditionof500nMhydrocortisonetoreinforcetightjunc-tions[33].
Themediumintheluminalchamber(ortheinsideoftheTranswellinsert)waschanged24hafterseeding.
BMECmonolayerswereculturedfor3daysbeforeuseinexperiments.
AnEVOMvoltohmmeterequippedwithaSTX-2electrode(WorldPrecisionInstruments;Sarasota,FL)wasusedtomeasuretransendothelialelectricalresistance(TEER,inohmspersquarecentimeter).
TheTEERofcell-freeTranswell-clearinsertswassubtractedfromobtainedvalues.
TEERwasmeasuredpriortotreatmentand24haftertreatment.
TheTEERvaluesre-portedinallfiguresaretheTEERpost-treatment.
TreatmentwithindomethacinandLPSCellswerepre-treatedwith50μlBMEC+HCwithorwithoutindomethacin(200μM).
After30min,50μlBMEC+HCwithorwithoutLPS(20μg/ml)wasaddedtowells.
Cellsweretreatedfor24h(indomethacinfinalconcentration:100μM,LPSfinalconcentration:10μg/ml).
TransendothelialpermeabilityForpermeabilityexperiments,Transwellinsertswerewashedwithserum-freeBMEC+HCmedium+0.
1%BSA.
Thesamemediumwasaddedtothewellsofanew24-wellplate,andthewashedinsertswereplacedinthisplate.
Toinitiatetransportexperiments,14C-sucrose(106cpm/ml)inmediumwasaddedtotheluminalchamber.
Forotherexperiments,99mTc-albumin(106cpm/ml)wasaddedtotheloadingsolutioninadditiontothe14C-sucrose.
Samples(500μl)werecollectedfromtheabluminalchamberat10,20,30,and45min,andwhensampleswereremoved,anequalvolumeoffresh1%BSA/serum-freeBMEC+HCmediumwasimmediatelyaddedtotheabluminalchamber.
Iftheloadingsolutiononlycontained14C-sucrose,liquidscintillationfluidwasaddedtoeachsampleandtheradioactivitywasmeasuredusingaliquidscintillationcounter.
Iftheloadingsolutioncontained99mTc-Alband14C-sucrose,eachsamplewasacidprecipitatedwith30%trichloroaceticacidandcentrifugedat5500*gfor10minat4°C.
Thepelletwascountedinagammacounterforpresenceof99mTc.
Thesupernatantwasremovedandplacedintoscintillationvials.
Liquidscintillationfluidwasaddedtothesupernatantsamplesafter3days,allowingforanyunbound99mTctodecay,andcountedinabetacounter.
Thepermeabilitycoefficientandclearanceofradio-activitywascalculatedaccordingtopreviouslypublishedmethods[34].
Clearancewasexpressedasmicrolitersofradioactivetracerdiffusingfromtheluminaltoablum-inalchamberandwascalculatedusingtheinitialamountofradioactivityintheloadingchamberandthemea-suredamountofradioactivityinthecollectedsamples.
ClearanceμlCCVC=CL;where[C]Listheinitialamountofradioactivitypermicroliterofthesolutionloadedintotheinsert(incountsperminutepermicroliter),[C]Cistheradioactivitypermicroliterinthecollectedsample(incountsperminutepermicroliter),andVCisthevolumeofcollectingBanksetal.
JournalofNeuroinflammation(2015)12:223Page4of15chamber(inmicroliters).
Theclearancevolumeincreasedlinearlywithtime.
Thevolumeclearedwasplottedversustime,andtheslopewasestimatedbylinearregressionanalysis.
TheslopeofclearancecurvesfortheBMECmonolayerplusTranswellmembranewasdenotedbyPSapp,wherePSisthepermeability*surfaceareaproduct(inmicrolitersperminute).
TheslopeoftheclearancecurvewithaTranswellmembranewithoutBMECswasdenotedbyPSmembrane.
TherealPSvaluefortheBMECmonolayer(PSe)wascalculatedfrom1=PSapp1=PSmembrane1=PSe:ThePSevaluesweredividedbythesurfaceareaoftheTranswellinsertstogeneratetheendothelialper-meabilitycoefficient(Pe,inmicrolitersperminutepersquarecentimeter).
ImmunohistochemistryforBMECBMECsgrownonTranswellinsertswerewashedinphosphate-bufferedsaline(PBS)andfixedwith4%PFAfor10minat4°C.
Cellswerepermeabilizedwith0.
1%TRITON-X100,blockedwith5%BSA,andthenincubatedwithanti-ZO-1ratmonoclonalantibody(Millipore,St.
Charles,MO,USA),claudin-5antibody(Abcam,Cambridge,MA),oroccludinantibody(Abcam)followedbyincubationwithAlexaFluor-568-conjugatedsecondaryantibody(Invitrogen,GrandIsland,NY,USA).
InsertsweremountedinantifademediumcontainingDAPI(nuclear)counterstain(SigmaAldrich)andphotographedwithaNikonECLIPSEE800fluorescencemicroscope.
SolubleTREM2ELISAToquantifytheconcentrationsofsolubletriggeringreceptorexpressedonmyeloidcells2(TREM2)extra-cellulardomain(sTREM2)inmouseEDTA-plasmasamples,weadaptedananti-TREM2ELISAsystemsimilartothatreportedbyKleinbergeretal.
[35-37].
ForthedetectionofsTREM2,plateswereincubatedovernightwithpolyclonalsheepanti-TREM2captureantibody(0.
25μg/ml)(R&DSystems,Minneapolis,MN).
Thefollowingdayplateswerewashedthreetimeswithwashingbuffer(0.
05%Tween20inPBS)andblockedin5%BSAand0.
05%Tween20inPBS(pH7.
4)for2hatroomtemperature.
Afterblocking,theplateswerewashedtwiceandloadedwith10μlplasmainto90μlblockingsolutionandincubatedovernight(4°C).
ArecombinantmouseTREM2protein(LifeTechnologies,GrandIsle,NY)wasdilutedinassaybufferinatwofoldserialdilutionandusedforthestandardcurvewithaconcentrationrangeof1000,500,250,125,62,31,15,and0pg/ml.
Thenextday,sampleswereremovedandplateswerewashedthreetimesfor5minwithwashingbufferbeforeincubationfor2hatroomtemperaturewithmousemonoclonalanti-TREM2antibody(1μg/ml)(SantaCruzBiotechnology;B-3)dilutedinblockingbuffer.
Afterthreeadditionalwashingsteps,plateswereincubatedwithanti-mouseHRP-conjugatedsec-ondaryantibody(1:4000)andincubatedfor1hbeforebeingwashedthreetimes.
Followinga30-minincuba-tionwithtetramethylbenzidine,plateswereanalyzedbymeasuringabsorbanceat620nm.
StandardcurvelinearityandinterplateandinterdayvariabilityforthesTREM2ELISAwasdeterminedusingdedicatedplasmasampleanchorsforallplates.
Repeatedfreeze-thawcycleshadnoeffectonsTREM2concentrationsinplasmaaspreviouslyreported[37].
ThespecificityoftheusedELISAsystemwasfurthervalidatedbyanti-TREM2immunoblottingshowingahighdegreeofcorrelationbetweentheELISAreadingsandimmu-noreactivityontheimmunoblotusingtheseantibodiesandanindependentanti-TREM2antibody,mouseanti-TREM22B5(R&DSystems,Minneapolis,MN).
Theplasmawasstoredat70°Cuntilused.
StatisticalanalysisAllstatisticalanalysesandgraphsweregeneratedusingGraphPadPrism5.
0(GraphPadSoftware,Inc.
,LaJolla,CA).
Errorbarsrepresentthestandarderrorofthemean(SEM).
ComparisonoftwomeanswasmadeusingStudent'sttest.
Comparisonofmorethantwogroupswasmadeusingone-wayanalysisofvariance(ANOVA)followedbyNewman-Keulspost-test.
ResultsEffectofLPSonBBBpermeability(singleinjection)Micewerestudied24hafterasingleIPinjectionofLPS.
ThehighestdoseofLPS(3mg/kg)administeredtoCD-1miceproducedasignificantincreaseinBBBpermeabilityasmeasuredwith14C-sucrose(Fig.
1),whereasthelowertwodoseswerewithouteffect.
Therewasasignificantdecreaseintheamountof14C-sucroseintheserum(12.
4±3.
9%injection/mlto8.
4±3.
4%injection/ml),indicatinganincreasedleakageofperipheralcapillarybeds.
IncontrasttoeffectsonBBBpermeability,alldosesofLPSproducedadecreaseinbodyweight(Fig.
2a).
NodoseofLPShadaneffectonbrainweight(Fig.
2b).
Theincreasein14C-sucrosewasevident24h,butnot4h,afteradoseof3mg/kgofLPS(Fig.
2c).
LPSalsoincreasedBBBpermeabilitytoalbumin(Fig.
2d).
TheeffectofLPSdifferedamongbrainregions(Table1).
Eightof11brainregionsshowedastatisticallysignifi-cantincreaseinBBBpermeabilityto14C-sucrose,butthehypothalamus,olfactorybulb,andoccipitalcortexhadarithmeticincreasesthatdidnotreachstatisticalsignificance(Table1).
Allotherstudiesusedthethree-injectionregimenofLPS.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page5of15EffectofNACandindomethacinonLPS-inducedBBBpermeabilityTodeterminewhethertheincreasedBBBpermeabilityinducedbyLPScouldbeblockedbytheadministrationoftheantioxidantNACortheCOXinhibitorindometh-acin,weadministeredtheseagentsintraperitoneally30minpriortotheinjectionsofLPS.
Forthesestudies,thethree-injectionregimenwasusedsoastomatchpreviouslypublishedBBBstudies[6,7,38,39].
AsshowninFig.
3,indomethacin(panelA),butnotNAC(panelB),inhibitedtheLPS-inducedincreaseinBBBpermeabilityto14C-sucrose.
IndomethacinalsopreventedtheLPS-induceddecreaseinbodyweight(datanotshown)ashasbeenpreviouslyreported[6].
NeitherLPSnorindomethacinhasaneffectonZO-1proteinlevelsasmeasuredbyWesternblotting(datanotshown).
EffectsofLPSandindomethacinonbraincytokinesTheeffectsofLPSandindomethacinonbraincytokinesweremeasuredusingaBio-Plexcytokineassaykit.
Ofthe23cytokinesanalyzed,onlyG-CSFandKCwerenotdetectable.
LPSproducedastatisticallysignificantincreaseinbrainlevelsforeightofthecytokines(Table2).
Indo-methacinpreventedanLPS-inducedincreaseofonlytwoofthese(IL-1βandIL-9)butfurtherincreasedlevelsforfourofthem(IL-1α,IL-4,IL-6,andMIP-1).
Forfivecytokines(IL-6,INF-γ,MIP-1α,MIP-1β,andRANTES),theLPS+indomethacin,butnottheLPS-onlygroup,hadincreasedvaluesascomparedtocontrols.
MicroglialandastrocyticactivationFigure4showstheresultsofimmunohistochemicalstainingformicroglia/macrophages(Iba1andF4/80)Fig.
1Dose-dependenceofLPSonBBBpermeabilityto14C-Sucrose.
Onlythe3mg/kgdoseincreasedBBBpermeability.
**pp>0.
05;*p<0.
05;**p<0.
01;***p<0.
001Fig.
3EffectsofindomethacinandN-acetylcysteineonLPS-inducedBBBdisruption.
Panelashowsthatpre-treatmentwithindomethacinpreventedLPS-inducedBBBdisruption(n=7–8/group),whereaspanelbshowsthatN-acetylcysteinewaswithouteffect(9–10/group).
*p<0.
05;**p<0.
01;****p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page7of15fromthoseofamonocultureofBECs.
Figure8showsthatLPSalsoinduceddisruptiontoTc-AlbinBECmonoculturesandthatthisdisruptionwaspartiallyblockedbyindomethacin.
DiscussionInflammation,includinginflammationinducedbyLPS,haslongbeenknowntodisrupttheBBB[3,4,43].
How-ever,manyaspectsofinflammation-inducedBBBdisruptionremainunexplored.
Here,weexaminedmechanismsthatunderlieinflammation-relatedBBBdisruption,beginningwithacharacterizationofthatdisruption.
Wefoundthatincomparisontoinductionofweightloss,ahighdoseofLPSwasrequiredtoinduceinvivoBBBdisruption.
Specifically,3mg/kg,butnot0.
3nor0.
03mg/kg,disruptedtheBBB.
Incontrast,alldosesofLPS,includingtheverylowdoseof0.
03mg/kg,inducedlossofbodyweight.
Bythismeasure,theBBBisresistanttoLPS-induceddisrup-tioninthatarelativelyhighdosewasneededtoinducedisruption.
ThisshowsthatLPScanactivateneuroimmunepathwaysandprocessessuchassick-nessbehaviorwithoutinducingorbeingdependentonBBBdisruption.
Incomparisontotherelativesensitivitytobodyweightloss,brainweightwasnotaffectedevenbythedosethatdisruptedtheBBB.
Thisisnotaltogetherex-pectedasbraindisruptionunderliesvasogenicedema;therefore,adisruptionoftheBBB,ifprolonged,wouldbeexpectedtoleadtobrainedemaand,hence,anincreaseinbrainweight.
BBBdisruptionasmeasuredbytheincreaseinsucrosespacewasnotuniformthroughoutthebrainbutvariedamongbrainregions.
Thehypothalamus,olfactorybulb,andoccipitalcortexhadsmallincreasesthatdidnotreachstatisticalsignificance,whereasthethalamus,frontalcortex,cerebellum,andpons-medullahadin-creasesofover50%.
Thispatterndiffersfromothercausesofdisruption.
Forexample,indiabetesmellitus,BBBdisruptionfirstoccursinthemidbrainwiththecerebellumbeinganarearesistanttodiabetes-inducedBBBdisruption[44].
Thisshowsthatregionalvulnerabil-itiesexistamongregionsoftheBBBbutsuggeststhatthoseregionsvaryasafunctionofinsult.
WefoundtheBBBwasdisruptedtobothalbuminandsucrose.
BBBintegrityisinducedbythreemodificationsofthecapillarybed:aninductionoftightjunctionsthatpreventsintercellular(paracellular)leakage,adecreaseTable2EffectsofindomethacinonLPS-inducedchangesincytokinelevelsinthebrain.
Valuesaremeans±SEMinunitsofpg/mgprotein(n)CytokineSaline(3)LPS(3)LPS+indo(4)SalinevsLPSSalinevsLPS+indoLPSvsLPS+indoIL-1α2.
5±0.
312.
7±1.
917.
9±1.
5indoincreases)IL-1β19.
7±2.
9120.
3±39.
834.
6±3.
2*NS*(indodecreases)IL-215.
8±2.
817.
8±2.
127.
3±3.
3NSNSNSIL-31.
4±0.
22.
1±0.
032.
6±0.
16***NSIL-40.
34±0.
020.
92±0.
081.
1±0.
05indoincreases)IL-50.
93±0.
071.
2±0.
161.
1±0.
1NSNSNSIL-61.
5±0.
1229.
7±16.
572.
8±13.
1NS**(indoincreases)IL-975.
0±3.
1156.
9±16.
489.
2±7.
0**NS**(indodecreases)IL-106.
3±0.
19.
0±0.
310.
4±0.
6****NSIL-12(p40)8.
5±1.
91084±648.
4385.
2±81.
8NSNSNSIL-12(p70)72.
5±6.
5102.
1±3.
197.
6±10.
3NSNSNSIL-1338.
1±2.
340.
0±3.
527.
7±3.
5NSNSNSIL-1719.
4±2.
324.
8±1.
620.
5±0.
9NSNSNSEotaxin2213±131.
52671±99.
82165±144.
3NSNSNSGM-CSF28.
6±2.
547.
1±1.
343.
9±2.
1****NSIFN-γ16.
1±2.
120.
6±1.
122.
9±1.
3NS*NSMCP-133.
0±4.
61550±300.
61612±275.
1****NSMIP-1a6.
8±0.
7128.
3±36.
1465.
2±108.
4NS**(indoincreases)MIP-1b56.
6±3.
5128.
9±15.
7190.
5±37.
0NS*NSRANTES1.
5±0.
3154.
8±37.
7280.
1±57.
3NS**NSTNF-α459.
9±34.
3482.
1±21.
3432.
2±16.
7NSNSNS*p<0.
05;**p<0.
01;***p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page8of15inmacropinocytosis,andalossofintracellularporesandfenestrae.
DisruptionoftheBBBcanbecausedbyreversalofanyorallofthesemodifications.
Sucrose,withamolecularweightof342Da,isthesmallestoftheclassicalvascularmarkersandthusisthemostsensitivefordetectingBBBdisruption.
Albuminatabout65kDaisthelargestoftheclassicalvascularmarkersusedtomeasureBBBdisruptionandthusrequiresamajordisruptionfordetection.
TEER,whichcanbeusedinvitro,requiresapatentchannelfortheexchangeofelec-trolytesbetweentheluminalandabluminalchambers.
AsmallamountofsucrosecrossestheBBBindependentlyofBBBdisruptionbythemechanismoftranscellulardiffusion,andasmallamountofalbuminenterstheCNSprimarilythroughtheextracellularpathways[45].
Hence,controlvaluesforneithersucrosenoralbuminarezero,andthevaluesobtainedhereincontrolmicearethoseexpectedbasedontheirentryratesofabout104ml/g-minforsucroseand105to106ml/g-minforalbumin.
Here,wefoundsignificantdisruptionsoftheBBBasassessedbybothsucroseandalbumininvivoandbyTEER,sucrose,andalbumininvitro.
PreviousworkhassuggestedthatBBBdisruptiontosmallermole-cules,butnotlargermolecules,isindicativeofopeningoftheparacellularrouteonly,whereasdisruptiontolar-gerandsmallermoleculesissuggestiveofopeningofFig.
4EffectsofLPSandindomethacinonmicroglial/macrophageandastrocyticactivation.
Microglial/macrophageactivationwasincreasedbyLPSbutnotblockedbyindomethacinasassessedbyIba1(left-handpanels)andbyF4/80(middlepanels)immunohistochemistry.
AstrocyticactivationwasincreasedbyLPSandblockedbyindomethacinasassessedbyGFAPstaining(right-handpanels).
ThebottomthreepanelsshowquantificationofIba1(n=5–6/statisticalcell),F4/80(n=5–6),andGFAP(n=4–5)immunohistochemicalstaining.
*p<0.
05,**p<0.
01,***p<0.
001,Mag=*20Banksetal.
JournalofNeuroinflammation(2015)12:223Page9of15boththeparacellularandthetranscellularroutes[17,18].
CytoarchitecturaltranslocationofthetightjunctionproteinsZO-1andoccludinalsosupportanincreaseinparacellularpermeability.
Claudin-5didnotshowachangewithLPStreatment,butthismaybebecauseitisthemostdeeplyembeddedofthesetightjunctionpro-teins[46]sothatitwouldbethelasttobetranslocatedinasequentialdisassemblyoftightjunctions.
Takento-gether,theinvivostudiesfindingdisruptiontobothsu-croseandtoalbuminandtheinvitrostudiesassessingTEER,tightjunctionproteinanalysis,andtheperme-abilitytosucroseandtoalbuminsuggestthatLPSre-sultsindisruptionbyboththeparacellularandthetranscellularpathways.
WefoundthatBBBdisruptionwaspresent24hafterinjectionofasingledoseof3mg/kgofLPS,butnot4haftertheinjection.
ArecentstudyhascharacterizedtheeffectofasimilarregimenofLPSonthelevelsof13cytokinesinthebrainandbloodandcanbeusedtoindicatewhichcytokinesarelesslikelytobeinvolvedinBBBdisruption[47].
Itislikelythatthosebraincytokinesnotelevatedateither4or24h(IL-1α,IL-13,IP-10,KC,TNF-α,GM-CSF)arelesslikelytobeinvolvedindisruptionthanthoseelevatedateither4orFig.
5EffectsofLPSplasmaTREM2.
PlasmaTREM2levelsareincreasedbyLPS,aneffectblockedbytreatmentwithindomethacin(n=8/group).
*p<0.
05Fig.
6EffectsofLPSonTEERofBMECsandcytoarchitectureofZO-1,claudin-5,andoccludin.
PanelsaandbshowthatLPSaddedeither24or48hearliertomonoculturesofBMECsdecreasedtheirTEERinadose-dependentmanner,consistentwithdisruptionoftheBBB.
ImmunostainingforZO-1showsincreasingdose-dependentcytoarchitecturaldisorganizationforZO-1(panelsc–f).
Immunostainingforclaudin-5(panelsgandh)doesnotclearlyshowsuchdisorganization,whereasimmunostainingforoccludindoes(panelsiandj).
*p<0.
05;***p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page10of15Fig.
7(Seelegendonnextpage.
)Banksetal.
JournalofNeuroinflammation(2015)12:223Page11of1524h(IL-1β,IL-6,IL-10,G-CSF,RANTES,MCP-1,MIP-1α).
Likewise,thosebraincytokinesfoundhereinwhichtheindomethacin+LPSgroupdidnotdifferfromtheLPS-onlygroup(Il-2,Il-3,Il-5,Il-10,Il-12(p40),Il-12(p70),Il-13,Il-17,eotaxin,TNF,GM-CSF,interferon-gamma,MCP-1,MIP-1β,RANTES)areunlikelytobeinvolvedinmediatingBBBdisruption.
WethendeterminedtheeffectsoftheantioxidantN-acetylcysteine(NAC)andthenonsteroidalanti-in-flammatorydrugindomethacinonLPS-inducedBBBdis-ruption.
NACrapidlycrossestheBBB[27,48],protectsBECfromoxidativestressinducedbymethamphetamineandantiretroviraldrugs[25,26,48],andreversesthedecreasedbrain-to-bloodtransportofamyloidbetapep-tideinducedbyLPS[27].
IndomethacinasaCOXinhibitordecreasesprostaglandin,prostacyclin,andthromboxanesynthesesandallowsthroughmassactionanincreaseinleukotrienes[49].
ItalsoreversestheeffectofLPSonamyloidbetapeptideefflux[23]andpotentiatesLPS-enhancedtransportofgp120acrosstheBBB[50]butiswithouteffectonLPS-inducedinhibitionofP-glycoproteinfunction[24].
Here,wefoundthatNACwaswithouteffectbutthatindomethacinpreventedLPS-inducedBBBdisruptionto14C-sucrose.
IndomethacinactsbyblockingCOXactivity,thusredu-cingprostaglandinproduction.
ThisstronglyindicatesthatLPSinducesBBBdisruptionthroughaCOX-dependentpathway,possiblyonethatinvolvessecretionofcytokinesfromtheBECs.
ReleaseofprostaglandinsfromBECsisknowntomediatethefeverinducedbyLPS,andindo-methacinattenuatesthatfeverbyblockingprostaglandinsynthesis[51,52].
ThatLPSisactingdirectlyonBECstoinducedisruptionandthatnoothercelltypeisrequiredforLPStoproducedisruptionundertheconditionsoftheseexperimentsareclearlyshownintheinvitrostudies.
AsshowninFig.
6,LPSdisruptedmono-layersofBECs;nocellotherthanBECswasincu-batedinthosemonolayers.
Therefore,LPSmustbeabletodisrupttheBBBbyactingdirectlyonBECs.
LPSisalsoknownfromotherstudiestoinduceneuroinflammation[53];wealsosawLPS-inducedneuroinflammationhereasevidencedbyincreasesinIba1,GFAP,andF4/80immunostainingandinbrainlevelsofeightcytokines.
Therefore,itisreasonabletoassumethatothercomponentsoftheneurovascu-larunit,suchasastrocytesorpericytes,wouldbeinvolvedinpromotingtheLPS-induceddisruptionoftheBBB.
However,wefoundthataddingneither(Seefigureonpreviouspage.
)Fig.
7EffectofLPSandindomethacin(Indo)onTEERand14C-sucrosepermeabilityinmonolayersofBECmonocultures(EOO,n=10),BEC+astrocyteco-cultures(EOA,n=5),BEC+pericyteco-cultures(EPO,n=5),andBEC+pericyte+astrocytetri-cultures(EPA,n=10).
PanelashowsthatinmonoculturesofBECs,LPSincreasedpermeabilitytosucroseandthatindomethacinpartiallyblockedthiseffect.
PanelbshowsthatLPSincreasedpermeabilityofmonolayermonoculturesofBECasmeasuredbyTEERandthatindomethacinhadnoeffectonLPS-inducedpermeability.
Co-culturesofBECswithastrocytes(panelscandd)orpericytes(panelseandf)ortri-culturesofBECswithpericytesandastrocytes(panelsgandh)didnotproduceresultssubstantiallydifferentfromthoseobtainedwithmonoculturesofBECs.
Y-axisis%ControlofPeinunitsofmicrolitersperminutepersquarecentimeter.
*p<0.
05,***p<0.
001;withoutbarcomparestorespective0value;withbarcomparesLPS10μg/mlwithoutindo-methacintoLPS10μg/mlwithindomethacinFig.
8EffectofLPSandindomethacinon14C-sucrose(upperpanel)andTc-Albpermeabilities(lowerpanel)inmonoculturesofBECs.
ResultsshowthatindomethacinpartiallyblockedtheLPS-inducedpermeabilityforbothsucroseandalbumin.
*p<0.
05,***p<0.
001;withoutbarcomparestorespective0value;withbarcomparesindicatedgroupsBanksetal.
JournalofNeuroinflammation(2015)12:223Page12of15pericytesnorastrocytesalteredtheresponseofBECstoLPS.
ThissuggeststhatBECsaloneareinvolvedinBBBdisruptioninourinvitromodel,althoughitisstillpossiblethatothercellscontributetoneuroinflammation-inducedBBBdisruptionunderotherexperimentalcondi-tions.
IncomparisontoLPS-induceddisruptionoftheBBB,LPS-inducedenhancementofinsulintransportacrosstheBBBinvolvesnitricoxidereleasefromnon-BBBcells[54]andLPS-enhancedtransportofHIV-1isenhancedbythepresenceofpericytes[50].
IndomethacinhadmixedeffectsonLPS-inducedin-flammation.
IndomethacindiddecreasetheLPS-inducedelevationinbrainlevelsofIL-1β,IL-9,andplasmaTREM2,thelatterusedasameasureofperipheralin-flammation.
IndomethacindecreasedtheLPS-inducedincreaseinGFAP,suggestingaroleforCOXinastro-cyticactivation,buthadnoeffectontheLPS-inducedincreaseinIba1orF4/80staining,suggestingthatactiva-tionofmicroglia/macrophagesisindependentofCOX.
Additionally,indomethacinfurtherincreasedoverLPSalonethelevelsoffourothercytokines.
Likewise,indomethacinhadamixedeffectonBBBdisruptionasmeasuredinvitro,havingnoeffectondisrup-tionasmeasuredbyTEER,butpartiallyblockingdisruptionasmeasuredbysucroseandalbumin.
BBBdisruptionasmeasuredbyTEERismoreassociatedwithparacellularpathways,whereasBBBdisruptionasmeasuredbysucroseandalbuminisassociatedwithtranscytosis.
ThissuggeststhatalthoughLPSinducesdisruptionbybothparacellularandtranscytoticpathways,theparacellularpathwayisme-diatedthroughCOX-independentmechanisms.
Thereareseveralimplicationsofthiswork.
First,althoughLPSisnotatruesepsismodel,itdoessuggestthatCOXinhibitionwouldbeprotectiveagainsttheBBBdisruptionseeninsepsisandinotherinflammatorystates.
Additionally,itisincreasinglyclearthatLPSentersthecirculationnotonlyindiseasestatessuchastheleakygutofAIDS[55]butalsoundermorephysio-logicconditions,suchasafteringestionofahigh-fatmealormarathonrunning[56,57].
ThelatterstudiessuggestthatLPSmayhaverolesinneuroimmunemodu-lationthatarenotstrictlypathological.
Forexample,LPSislikelyoneofthemediatorsresponsibleforthedifferentialresponseoftissues,includingthebrain,tohealthyandpathologicmicrobiomes[58,59].
ThesestudiesfoundthathighdosesofLPSarerequiredtodisrupttheBBBwhentheLPSexposureisacutebutdidnotinvestigatetheeffectsofchronic,low-doseexposuretoLPSonBBBintegrity.
ConclusionsTheseresultsshowthattheBBBisrelativelyresistanttodisruptionbyLPSincomparisontoanotherclassiceffectofLPS,thatofweightloss.
NotallregionsoftheBBBareequallysensitivetoLPS-inducedBBBdisrup-tion,involvementofnon-BECsisnotrequiredforLPStoinducedisruption,anddisruptionoccursthroughbothparacellularandtranscytoticmechanismswithtranscytoticdisruptionbeingprostaglandin-dependent.
AbbreviationsBBB:blood-brainbarrier;BECs:brainendothelialcells;BMECs:brainmicrovascularendothelialcells;BSA:bovineserumalbumin;COX:cyclooxygenase;I-Alb:iodine-labeledalbumin;IL:interleukin;ImPCs:immortalizedmousebrainpericytes;LPS:lipopolysaccharide;NAC:N-acetylcysteine;Tc-Alb:technetium-labeledalbumin;TEER:transendothelialelectricalresistance;TREM2:triggeringreceptorexpressedonmyeloidcells2.
CompetinginterestsNoauthorhasafinancialornon-financialcompetinginterest.
Authors'contributionsWilliamA.
Banks:conceivedoverallapproachandquestion,performedmostoftheexperimentaldesign,andwrotetheMS.
AliciaM.
Gray,MichelleA.
Erickson,andThereseS.
Salameh:conductedinvivostudiesandcontributedtoinvivoexperimentaldesign.
MamathaDamodarasamyandMayJ.
Reed:IHC.
NaderSheibani:providedimmortalizedpericytes.
JamesS.
MeabonandDavidG.
Cook:TREM2assays.
EmilyE.
WingandYoichiMorofuji:invitroassays.
Allauthorsreadandapprovedthefinalmanuscript.
AcknowledgementsWewouldliketothankDr.
JessicaHamerman(UniversityofWashington)forTREM2KOmousematerialsandtheratanti-TREM2antibody.
SupportedbytheVAandR01AG029839(WAB).
Authordetails1GeriatricResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA.
2DivisionofGerontologyandGeriatricMedicine,DepartmentofInternalMedicine,UniversityofWashingtonSchoolofMedicine,Seattle,WA,USA.
3UniversityofWashingtonSchoolofMedicine,Seattle,WA,USA.
4OphthalmologyandVisualSciences,UniversityofWisconsinSchoolofMedicineandPublicHealth,Madison,WI,USA.
5MentalHealthResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA.
6DepartmentofNeurosurgery,UniversityofNagasaki,Nagasaki,Japan.
Received:13July2015Accepted:14November2015References1.
SkoogT.
Onthevitalstainingofthecentralnervoussystem.
ActaOtolaryngologica.
1937;25:365–78.
2.
RapoportSI.
Pathologicalalterationsoftheblood-brainbarrier.
In:Blood-brainbarrierinphysiologyandmedicine.
NewYork:Raven;1976.
p.
129–52.
3.
AllenIV.
Theeffectofbacterialpyrogenontheblood-brainbarrierfortrypanblue.
JPatholBacteriol.
1965;89:481–94.
4.
EckmanPL,KingWM,BrunsonJG.
Studiesonthebloodbrainbarrier.
I.
Effectsproducedbyasingleinjectionofgram-negativeendotoxinonthepermeabilityofthecerebralvessels.
AmJPathol.
1958;34:631–43.
5.
PersidskyY,StinsM,WayD,WitteMH,WeinandM,KimKS,etal.
Amodelformonocytemigrationthroughtheblood-brainbarrierduringHIV-1encephalitis.
JImmunol.
1997;158:3499–510.
6.
BanksWA,KastinAJ,BrennanJM,VallanceKL.
AdsorptiveendocytosisofHIV-1gp120byblood-brainbarrierisenhancedbylipopolysaccharide.
ExpNeurol.
1999;156:165–71.
7.
XaioH,BanksWA,NiehoffML,MorleyJE.
EffectofLPSonthepermeabilityoftheblood-brainbarriertoinsulin.
BrainRes.
2001;896:36–42.
8.
MinamiT,OkazakiJ,KawabataA,KurodaR,OkazakiY.
Penetrationofcisplatinintomousebrainbylipopolysaccharide.
Toxicology.
1998;130:107–13.
9.
PanW,YuC,HsuchouH,ZhangY,KastinAJ.
NeuroinflammationfacilitatesLIFentryintobrain:roleofTNF.
AmJPhysiolCellPhysiol.
2008;294:C1436–42.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page13of1510.
TucsekZ,TothP,SosnowskaD,GautamT,MitschelenM,KollerA,etal.
Obesityinagingexacerbatesblood-brainbarrierdisruption,neuroinflammation,andoxidativestressinthemousehippocampus:effectsonexpressionofgenesinvolvedinbeta-amyloidgenerationandAlzheimer'sdisease.
JGerontolABiolSciMedSci.
2013,epub.
11.
SengilloJD,WinklerEA,WalkerCT,SullivanJS,JohnsonM,ZlokovicBV.
Deficiencyinmuralvascularcellscoincideswithblood-brainbarrierdisruptioninAlzheimer'sdisease.
BrainPathol.
2012;23:303–10.
12.
StarrJM,WardlawJ,FergusonK,MacLullichA,DearyIJ,MarshallI.
Increasedblood-brainbarrierpermeabilityintypeIIdiabetesdemonstratedbygadoliniummagneticresonanceimaging.
JNeurolNeurosurgPsychiatry.
2003;74:70–6.
13.
AbrahamCS,HaradaN,DeliMA,NiwaM.
Transientforebrainischemiaincreasestheblood-brainbarrierpermeabilityforalbumininstroke-pronespontaneouslyhypertensiverats.
CellMolNeurobiol.
2003;22:455–62.
14.
PozzilliC,BernardiS,MansiL,PicozziP,IannottiF,AlfanoB,etal.
Quantitativeassessmentoftheblood-brainbarrierpermeabilityinmultiplesclerosisusing68-Ga-EDTAandpositronemissiontomography.
JNeurolNeurosurgPsychiatry.
1988;51:1058–62.
15.
ReeseTS,KarnovskyMJ.
Finestructurallocalizationofablood-brainbarriertoendogenousperoxidase.
JCellBiol.
1967;34:207–17.
16.
BrightmanMW,ReeseTS.
Junctionsbetweenintimatelyapposedcellmembranesinthevertebratebrain.
JCellBiol.
1969;40:648–77.
17.
MayhanWG,HeistadDD.
Permeabilityofblood-brainbarriertovarioussizedmolecules.
AmJPhysiology.
1985;248:H712–8.
18.
ZiylanYZ,RobinsonPJ,RapoportSI.
Blood-brainbarrierpermeabilitytosucroseanddextranafterosmoticopening.
AmJPhysiol.
1984;247:R634–8.
19.
KnowlandD,AracA,SekiguchiKJ,HsuM,LutzSE,PerrinoJ,etal.
Stepwiserecruitmentoftranscellularandparacellularpathwaysunderliesblood-brainbarrierbreakdowninstroke.
Neuron.
2014;82:603–17.
20.
Fleegal-DeMottaMA,DohguS,BanksWA.
AngiotensinIImodulatesBBBpermeabilityviaactivationoftheAT1receptorinbrainendothelialcells.
JCerebBloodFlowMetab.
2009;29:640–7.
21.
DeVriesHE,Blom-RoosemalenMCM,DeBoerAG,vanBerkelTJ,BreimerDD,KuiperJ.
Effectofendotoxinonpermeabilityofbovinecerebralendothelialcelllayersinvitro.
JPharmacolExpTher.
1996;277:1418–23.
22.
MinamiT,OkazakiJ,KawabataA,KawakiH,OkazakiY,TohnoY.
Rolesofnitricoxideandprostaglandinsintheincreasedpermeabilityoftheblood-brainbarriercausedbylipopolysaccharide.
EnvironToxicolPharmacol.
1998;5:35–41.
23.
JaegerJB,DohguS,LynchJL,Fleegal-DeMottaMA,BanksWA.
Effectsoflipopolysaccharideontheblood-brainbarriertransportofamyloidbetaprotein:amechanismforinflammationintheprogressionofAlzheimer'sdisease.
BrainBehavImmun.
2009;23:507–17.
24.
SalkeniMA,LynchJL,PriceTO,BanksWA.
Lipopolysaccharideimpairsblood-brainbarrierP-glycoproteinfunctioninmicethroughprostaglandin-andnitricoxide-independentpathwaysandnitricoxide-independentpathways.
JNeuroimmunePharmacology.
2009;4:276–82.
25.
ZhangX,BanerjeeA,BanksWA,ErcalN.
N-acetylamideprotectsagainstmethamphetamine-inducedoxidativestressandneurotoxicityinimmortalizedhumanbrainendothelialcells.
BrainRes.
2009;1275:87–95.
26.
MandaKR,BanerjeeA,BanksWA,ErcalN.
Highlyactiveantiretroviraltherapydrugcombinationinducesoxidativestressandmitochondrialdysfunctioninimmortalizedhumanblood-brainbarrierendothelialcells.
FreeRadicBiolMed.
2011;50:801–10.
27.
EricksonMA,HansenK,BanksWA.
Inflammation-induceddysfunctionofthelow-densitylipoproteinreceptor-relatedprotein-1attheblood-brainbarrier:protectionbytheantioxidantN-acetylcysteine.
BrainBehavImmun.
2012;26:1085–94.
28.
CoisneC,DehouckL,FaveeuwC,DelplaceY,MillerF,LandryC,etal.
Mousesyngenicinvitroblood-brainbarriermodel:anewtooltoexamineinflammatoryeventsincerebralendothelium.
LabInvest.
2005;85:734–46.
29.
JacobA,HackB,ChiangE,GarciaJG,QuiggRJ,AlexanderJJ.
C5aaltersblood-brainbarrierintegrityinexperimentallupus.
FASEBJ.
2010;24:1682–8.
30.
PerriereN,DemeuseP,GarciaE,ReginaA,DebrayM,AndreuxJP,etal.
Puromycin-basedpurificationofratbraincapillaryendothelialcellcultures.
JNeurochem.
2005;93:279–89.
31.
ShahGN,PriceTO,BanksWA,MorofujiY,KovacA,ErcalN,etal.
Pharmacologicalinhibitionofmitochondrialcarbonicanhydrasesprotectsmousecerebralpericytesfromhighglucose-inducedoxidativestressandapoptosis.
JPharmacolExpTherap.
2013;344:637–45.
32.
NakagawaS,DeliMA,KawaguchiH,ShimizudaniT,ShimonoT,KittelA,etal.
Anewblood-brainbarriermodelusingprimaryratbrainendothelialcells,pericytesandastrocytes.
NeurochemInt.
2009;54:253–63.
33.
HoheiselD,NitsT,FrankeH,WegenerJ,HakvoortA,TillingT,etal.
Hydrocortisonereinforcestheblood-brainbarrierpropertiesinaserumfreecellculturesystem.
BiochemBiophysResCommun.
1998;217:312–5.
34.
DehouckMP,Jolliet-RiantP,BreeF,FruchartJC,CecchelliR,TillementJP.
Drugtransferacrosstheblood-brainbarrier:correlationbetweeninvitroandinvivomodels.
JNeurochem.
1992;58:1790–7.
35.
ScimemiA,MeabonJS,WoltjerRL,SullivanJM,DiamondJS,CookDG.
Amyloid-β1-42slowsclearanceofsynapticallyreleasedglutamatebymislocalizingastrocyticGLT-1.
JNeurosci.
2013;33:5312–8.
36.
DawsMR,LanierLL,SeamanWE,RyanJC.
CloningandcharacterizationofanovelmousemyeloidDAP12-associatedreceptorfamily.
EurJImmunol.
2001;31:783–91.
37.
KleinbergerG,YamanishiY,Suarez-CalvetM,CzirrE,LohmannE,CuyversE,etal.
TREM2mutationsimplicatedinneurodegenerationimpaircellsurfacetransportandphagocytosis.
SciTranslMed.
2014;6:243ra286.
38.
NonakaN,ShiodaS,BanksWA.
Effectoflipopolysaccharideonthetransportofpituitaryadenylatecyclaseactivatingpolypeptideacrosstheblood-brainbarrier.
ExpNeurol.
2005;191:137–44.
39.
EricksonMA,HartvigsonPE,MorofujiY,OwenJB,ButterfieldDA,BanksWA.
Lipopolysaccharideimpairsamyloidbetaeffluxfrombrain:alteredvascularsequestration,cerebrospinalfluidreabsorption,peripheralclearanceandtransporterfunctionattheblood-brainbarrier.
JNeuroinflammation.
2012;9:150.
40.
TurnbullIR,GilfillanS,CellaM,AoshiT,MillerMC,PiccioL,etal.
Cuttingedge:TREM-2attenuatesmacrophageactivation.
JImmunol.
2006;177:3520–4.
41.
HamermanJA,JarjouraJR,HumphreyMB,NakamuraMC,SeamanWE,LanierLL.
Cuttingedge:inhibitionofTLRandFcRresponsesinmacrophagesbytriggeringreceptorexpressedonmyeloidcells(TREM0-2andDAP12).
JImmunol.
2006;177:2051–5.
42.
SchmidCD,MelchiorB,MasekK,PuntambekarSS,DanielsonPE,LoDD,etal.
DifferentialgeneexpressioninLPS/IFNgammaactivatedmicrogliaandmacrophages:invitroversusinvivo.
Neurochem.
2009;109Suppl1:117–25.
43.
WispelweyB,LesseAJ,HansenEJ,ScheldWM.
Haemophilusinfluenzaelipopolysaccharide-inducedbloodbrainbarrierpermeabilityduringexperimentalmeningitisintherat.
JClinInvestig.
1988;82:1339–46.
44.
HuberJD,VanGilderRL,HouserKA.
Streptozotocin-induceddiabetesprogressivelyincreasesblood-brainbarrierpermeabilityinspecificbrainregionsinrats.
AmJPhysiol.
2006;291:H2660–8.
45.
KimYS,LeeMH,WisniewskiHM.
Aluminuminducedreversiblechangeinpermeabilityoftheblood-brainbarrierto[14C]sucrose.
BrainRes.
1986;377:286–91.
46.
BrownRC,DavisTP.
Calciummodulationofadherenstightjunctionfunction:apotentialmechanismforblood-brainbarrierdisruptionafterstroke.
Stroke.
2002;33:1706–11.
47.
EricksonMA,BanksWA.
Cytokineandchemokineresponsesinserumandbrainaftersingleandrepeatedinjectionsoflipopolysaccharide:multiplexquantificationwithpathanalysis.
Brain,Behavior,&Immunity.
2011;25:1637–48.
48.
FarrSA,PoonHF,Dogrukol-AkD,DrakeJ,BanksWA,EyermanE,etal.
Theantioxidantsalpha-lipoicacidandN-acetylcysteinereversememoryimpairmentandbrainoxidativestressinagedSAMP8mice.
JournalofNeurochemisrty.
2003;84:1173–83.
49.
VaneJR,BottingRM.
Mechanismofactionofanti-inflammatorydrugs.
AdvExpMedBiol.
1997;433:133–8.
50.
DohguS,BanksWA.
Lipopolysaccharide-enhancedtranscellulartransportofHIV-1acrosstheblood-brainbarrierismediatedbythep38mitogen-activatedproteinkinasepathway.
ExpNeurol.
2008;210:740–9.
51.
EngstromL,RuudJ,EskilssonA,LarssonA,MackerlovaL,KugelbergU,etal.
Lipopolysaccharide-inducedfeverdependsonprostaglandinE2productionspecificallyinbrainendothelialcells.
Endocrinology.
2012;153:4849–61.
52.
InoueW,MatsumuraK,YamagataK,TakemiyaT,ShirakiT,KobayashiS.
Brain-specificendothelialinductionofprostaglandinE(2)synthesisenzymesanditstemporalrelationtofever.
NeurosciRes.
2002;44:51–61.
53.
QinL,WuX,BlockML,LiuY,BreeseGR,HongJS,etal.
SystemicLPScauseschronicneuroinflammationandprogressiveneurodegeneration.
Glia.
2007;55:453–62.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page14of1554.
BanksWA,DohguS,NakaokeR,LynchJL,Fleegal-DeMottaMA,EricksonMA,etal.
NitricoxideisoenzymesregulateLPS-enhancedinsulintransportacrosstheblood-brainbarrier.
Endocrinology.
2008;149:1514–23.
55.
BrenchleyJM,PriceDA,SchackerTW,AsherTE,SilvestriG,RaoS,etal.
MicrobialtranslocationisacauseofsystemicimmuneactivationinchronicHIVinjection.
NatMed.
2006;12:1365–71.
56.
NgQY,LeeKW,ByrneC,HoTF,LimCL.
Plasmaendotoxinandimmuneresponsesduringa21-kmroadraceunderawarmandhumidenvironment.
AnnAcadMedSingapore.
2008;37:307–14.
57.
AmarJ,BurcelinR,RuidavetsJB,CaniPD,FauvelJ,AlessiMC,etal.
Energyintakeisassociatedwithendotoxemiainapparentlyhealthymen.
AmJClinNutr.
2008;87:1219–23.
58.
JasarevicE,HowertonCL,HowardCD,BaleTL.
Alterationsinthevaginalmicrobiomebymaternalstressareassociatedwithmetabolicreprogrammingoftheoffspringgutandbrain.
Endocrinology.
2015;156:3265–76.
59.
BanksWA.
Avaginamonologue:mom'sstress,bugs,andbaby'sbrain.
Endocrinology.
2015;156:3066–8.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Banksetal.
JournalofNeuroinflammation(2015)12:223Page15of15
Banks1,2*,AliciaM.
Gray3,MichelleA.
Erickson1,2,ThereseS.
Salameh1,MamathaDamodarasamy2,NaderSheibani4,JamesS.
Meabon5,EmilyE.
Wing1,YoichiMorofuji1,2,6,DavidG.
Cook1andMayJ.
Reed2AbstractBackground:Disruptionoftheblood-brainbarrier(BBB)occursinmanydiseasesandisoftenmediatedbyinflammatoryandneuroimmunemechanisms.
InflammationiswellestablishedasacauseofBBBdisruption,butmanymechanisticquestionsremain.
Methods:Weusedlipopolysaccharide(LPS)toinduceinflammationandBBBdisruptioninmice.
BBBdisruptionwasmeasuredusing14C-sucroseandradioactivelylabeledalbumin.
Braincytokineresponsesweremeasuredusingmultiplextechnologyanddependenceoncyclooxygenase(COX)andoxidativestressdeterminedbytreatmentswithindomethacinandN-acetylcysteine.
Astrocyteandmicroglia/macrophageresponsesweremeasuredusingbrainimmunohistochemistry.
InvitrostudiesusedTranswellculturesofprimarybrainendothelialcellsco-ortri-culturedwithastrocytesandpericytestomeasureeffectsofLPSontransendothelialelectricalresistance(TEER),cellulardistributionoftightjunctionproteins,andpermeabilityto14C-sucroseandradioactivealbumin.
Results:IncomparisontoLPS-inducedweightloss,theBBBwasrelativelyresistanttoLPS-induceddisruption.
DisruptionoccurredonlywiththehighestdoseofLPSandwasmostevidentinthefrontalcortex,thalamus,pons-medulla,andcerebellumwithnodisruptioninthehypothalamus.
TheinvitroandinvivopatternsofLPS-induceddisruptionasmeasuredwith14C-sucrose,radioactivealbumin,andTEERsuggestedinvolvementofbothparacellularandtranscytoticpathways.
Disruptionasmeasuredwithalbuminand14C-sucrose,butnotTEER,wasblockedbyindomethacin.
N-acetylcysteinedidnotaffectdisruption.
Invivo,themeasuresofneuroinflammationinducedbyLPSweremainlynotreversedbyindomethacin.
Invitro,theeffectsonLPSandindomethacinwerenotalteredwhenbrainendothelialcells(BECs)wereculturedwithastrocytesorpericytes.
Conclusions:TheBBBisrelativelyresistanttoLPS-induceddisruptionwithsomebrainregionsmorevulnerablethanothers.
LPS-induceddisruptionappearsistobedependentonCOXbutnotonoxidativestress.
Basedoninvivoandinvitromeasuresofneuroinflammation,itappearsthatastrocytes,microglia/macrophages,andpericytesplaylittleroleintheLPS-mediateddisruptionoftheBBB.
Keywords:Blood-brainbarrier,Neurovascularunit,Neuroinflammation,Brainendothelialcells,Indomethacin,Lipopolysaccharide*Correspondence:wabanks1@uw.
edu1GeriatricResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA2DivisionofGerontologyandGeriatricMedicine,DepartmentofInternalMedicine,UniversityofWashingtonSchoolofMedicine,Seattle,WA,USAFulllistofauthorinformationisavailableattheendofthearticle2015Banksetal.
OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Banksetal.
JournalofNeuroinflammation(2015)12:223DOI10.
1186/s12974-015-0434-1BackgroundThevascularblood-brainbarrier(BBB)protectsthecentralnervoussystemfromblood-bornesubstancesthatareotherwiseneurotoxic.
InflammationhaslongbeenknowntodisrupttheBBB.
Skoogin1937foundthatanallergicreactioncoulddisrupttheBBB[1].
Meningitis,encephalitis,sepsis,andlocalandsystemicinfectionshavebeenassociatedwithalteredpermeabilityoftheBBBtomanysubstancesandimmunecells[2].
Eckmanetal.
asearlyas1958andAllenafewyearslatershowedthatgram-negativeendotoxinwasassociatedwithBBBdisruption[3,4].
Gram-negativeendotoxininitsmorepurifiedformoflipopolysaccharide(LPS)isknowntodisrupttheBBBandalsoaltersmanyotheraspectsofBBBfunc-tion,includingadsorptivetranscytosis,immunecelltrafficking,andvarioustransportfunctions[5–9].
Morerecently,anumberofdiseasesthatincludemultiplesclerosis,Alzheimer'sdisease,diabetesmel-litus,obesity,andstrokehavebeenassociatedwithbothinflammationandBBBdisruption[10–14].
Thebarrierfunctionsofthecapillarybedofthebrainareknowntoarisefromthreemodifications:thepresenceoftightjunctionsbetweenendothelialcells,anearabsenceofmacropinocytosis,andlossoffenestrae[15,16].
Together,thesethreemodifica-tionspreventtheproductionofanultrafiltratebythebrain'scapillarybed.
InflammationcaninduceBBBdisruptionbyalteringtightjunctionfunction,thuspromotingparacellularleakage,andre-inducingvesicularprocesses,thuspromotingtranscytoticleak-age.
Insomecauses,transcytoticmechanismsmaybethedominantformofBBBdisruption[17,18]andmayprecedeparacellularopening[19,20].
MechanismsbywhichLPSaffectsBBBfunctionarenotwellunderstood.
Thecyclooxygenase(COX)inhibitorindomethacinreversessomeLPS-induceddysfunctionsoftheBBB,includinginvitrodisrup-tion[21,22]andinvivoimpairedamyloidbetapeptideefflux[23].
However,indomethacinhasnoeffectonLPS-inducedinhibitionofP-glycoproteinactivity[24].
TheantioxidantN-acetylcysteine(NAC)protectsthebrainendothelialcell(BEC)fromoxida-tivestressinducedbymethamphetamineandanti-retroviraldrugs[25,26]andreversesthedecreasedbrain-to-bloodtransportofamyloidbetapeptideinducedbyLPS[27].
TheeffectofNAConLPS-inducedBBBdisruptionhasnotbeenexaminedinvivo.
Here,wefurtherexaminedthemechanismsbywhichLPSinducesBBBdisruptionbothinvivoandinvitrobyinvestigatingbraincytokines,prostaglan-dininhibition,oxidativestress,andastrocyteandmicroglialactivation.
MethodsAnimalsAllmiceweretreatedinaccordancewithNIHGuidelinesfortheCareandUseofLaboratoryAnimalsinanAAALAC-accreditedfacilityandapprovedbytheInstitu-tionalAnimalCareandUseCommitteeoftheVAPugetSoundHealthCareSystem.
MaleCD-1miceat6–8weeksofagewerepurchasedfromCharlesRiverandkeptona12/12-hlight/darkcyclewithadlibitumfoodandwater.
RadioactiveprobesSucroselabeledwith14CwaspurchasedfromPerkin-Elmer(Waltham,MA).
Bovineserumalbumin(BSA)waslabeledwith125Ibythechloramine-Tmethod,andtheresultingradioactivealbumin(iodine-labeledalbumin(I-Alb))waspurifiedonaG-10Sephadexcolumn.
BSAwaslabeledwith99mTc(technetium-labeledalbumin(Tc-Alb))andpurifiedonaG-10Sephadexcolumn.
Lipopolysaccharide(LPS)doseresponseandtimestudiesMaleCD-1miceaged6–10weekswereweighedandgivenanintraperitoneal(IP)injectionof0.
03,0.
3,or3mg/kgLPSfromSalmonellatyphimurium(SigmaAldrich,St.
Louis,MO,USA)dissolvedinsterilenormalsaline.
Micewerereweighedabout23haftertheLPSinjection,anesthetizedwithurethane,andthejugularveinsexposed.
Themiceweregivenanivinjectionof14C-sucrose(106dpmin0.
2mloflactatedRinger'ssolutionwith1%BSA)24h±20minaftertheLPSinjection.
Arterialbloodwascollectedfromacutinthedescendingabdominalaorta.
Thevascularspaceofthebrainwaswashedfreeofbloodbyopeningthethorax,clampingthedescendingthoracicaorta,severingbothjugularveins,andperfusing20mloflactatedRinger'ssolutionthroughtheleftventricleoftheheartinlessthan1min.
Afterwashout,themousewasimmediatelydecapitatedandthewholebrainwasremovedandweighed.
Serumwasobtainedbycentrifugingthecarotidarterybloodfor10minat4000*g.
Thebrainsweresolu-bilized,andthelevelofradioactivityinthebrainsandseraweredeterminedinabetacounter.
Asubsetofmicethatreceived3mg/kgofLPSwasstudiedfor14C-sucrosepermeation4haftertheLPSinjection.
Anothersubsetofmicethatwerestudiedfor14C-sucrosepermeation24hafterreceiving3mg/kgofLPShadtheirbrainsdissectedintotheolfactorybulb,frontalcortex,parietalcortex,occipitalcortex,striatum,hippocampus,hypothalamus,thalamus,cerebellum,pons-medulla,andmidbrain.
OthermicereceivedaninjectionofI-Albinsteadof14C-sucrose,butwereotherwisetreatedthesame,receiving3mg/kgofLPSandbeingstudiedat24h.
Levelsofradioactivityintheserumandbrainweredeterminedinagammacounter.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page2of15Resultswerecalculatedbydividingthecountspermi-nuteperbrainorbrainregionbythecountsperminutepermicroliterinthecorrespondingserumandbytheweightofthebrainorbrainregion.
Theresultswerethusexpressedasmicroliterspergramofbraintissue.
Bloodlevelswerecalculatedasthepercentoftheinjecteddosepresentpermilliliterofserum(%injec-tion/ml)bydividingthecountsperminutepermilliliterbythecpminjectedivandmultiplyingby100.
AdministrationofNACorindomethacinIntheNACstudy,maleCD-1micewereassignedtooneoffourgroups.
Allmicereceivedinjectionsof100μlofsalineat30min,0,6,and24h.
Ingroups1and3,the30-mininjectionwassaline,andingroups2and4,itwassalinecontainingNAC(100mg/kg;SigmaAldrich,St.
Louis,MO).
Ingroups1and2,theremaininginjections(0,6,24h)weresaline,whereasingroups3and4,thesalinevehiclecontainedLPS(3mg/kg).
Fourhoursafterthelastinjection,micereceivedaninjectionof106cpmof14C-sucroseandwerestudiedasdescribedabove.
Indomethacin(5mg/kg)wasstudiedinthesamedesignusingitinplaceofNAC.
Forthefirstinjection,7%NaHCO3wasusedasthevehicleinsteadofsaline.
CytokinemeasurementsWholebrainlysatesfrommicetreatedwiththethree-injectionregimenofLPSdescribedaboveweregentlyhomogenizedin150μlofNP40buffer(Invi-trogen,GrandIsland,NY).
Sampleswerecentrifugedfor5minat4°Cand12,000*g.
ProteincontentofthesupernatantwasthendeterminedaccordingtotheBCAassayprotocolsuppliedbythemanufac-turer.
Proteinconcentrationsareattached.
Apanelof23cytokines(interleukin(IL)-1α;IL-1β;IL-2;IL-3;IL-4;IL-5;IL-6;IL-9;IL-10;IL-12(p40);IL-12(p70);IL-13;IL-17;eotaxin(CCL11);granulocytecolony-stimulatingfactor(G-CSF);granulocyte-macrophagecolony-stimulatingfactor(GM-CSF);interferon(IFN)-γ;keratinocytechemoattractant(KC)(CXCL1);monocytechemoattract-antprotein(MCP)-1(CCL2);macrophageinflammatoryprotein(MIP)-1α(CCL3);MIP-1β(CCL4);regulatedonactivation,normalTcellexpressedandsecreted(RANTES;CCL5)andtumornecrosisfactor(TNF)-α)weremeasuredinwholebrainlysatesusingamurineBio-PlexProassaykit(Bio-RadLaboratories,Inc.
;Hercules,CA).
Allsampleswerediluted1:3insampledi-luentprovidedinthekitandprocessedaccordingtothemanufacturer'sprotocol.
PlateswerereadonaBio-Plex200(Bio-RadLaboratories,Inc.
;Hercules,CA).
ImmunohistochemistryControlmiceormicetreatedwiththeLPS±indometh-acinregimendescribedabovewereeuthanized,andtheirbrainsremovedandfixedin10%neutral-bufferedformalin,paraffin-embedded,andsectionedat5μm.
Sectionswerede-paraffinized,blockedin2%goatserum,andexposedto2–5μg/mlofmouseanti-F4/80(Serotec)orrabbitanti-Iba1(Wako).
SectionswerethenrinsedinTris-bufferedsalineandexposedto5μg/mlofbiotinylatedanti-mouseoranti-rabbitIgGandthentoVectastainavidin-biotincomplex(ABC)kit(Vector)inconjunctionwith3,3′-diaminobenzidine(DAB,Vector)toderiveaninsolublestainthatcouldbequantified.
Forquantification,aminimumoftwodigitalimagespermousecerebralcortexweretakenat*20magnifica-tion.
TheimageswereprocessedinImageJ,andthebrightnessandcontrastadjustedbeforeconvertingtoanRGBstackimage.
ThethresholdofthebluestackimageisadjusteduntilthestainedtissueshowsoptimalcontrastwithhighlightingoftheDABstaininred.
Thestainingareaanddensityweremeasured,andtheresultwasexpressedasanareafraction,whichisthepercentoftheenclosedareathatishighlightedinred.
Relativestainingintensitywasthencalculatedforthecerebralcorticesforeachgroupofmice.
WesternblottingforZO-1Individualbrainextractsofequivalenttotalproteincontentwereresolvedbysodiumdodecylsulfate-polyacrylamidegelelectrophoresis(SDS-PAGE)(50μgtotalprotein/lane)underreducingconditions,trans-ferredtonitrocellulose,andprobedwith1μg/mlofrabbitpolyclonalantibodiestoZO-1(Invitrogen).
Blotswerethenprobedwithanti-rabbithorseradishperoxidase-conjugatedsecondaryantibody(JacksonImmunoResearch,WestGrove,PA)(1μg/ml)andvisual-izedbyenhancedchemiluminescence(GEHealthcareLifeSciences,Piscataway,NJ).
DensitiesofthebandswerequantifiedusingImageJ.
Isolationofprimarybrainmicrovascularendothelialcells(BMECs)Primarybrainmicrovascularendothelialcells(BMECs)wereisolatedfrom8-week-oldCD-1miceaccordingtoexistingprotocols[28,29]withsomemodifications.
BMECswereculturedinBMECmedium,consistingofDulbecco'smodifiedEagle'smedium(DMEM)/F12supplementedwith20%plasma-derivedfetalbovineserum(AnimalTechnologies),1%GlutaMAX(LifeTechnologies),basicfibroblastgrowthfactor(bFGF,1ng/ml;RocheLifeSciences),heparin(100μg/ml),insulin(5μg/ml),transferrin(5μg/ml),selenium(5ng/ml)(insulin-transferrin-seleniummediumsupplement;LifeTechnologies),andgentamicin(50μg/ml;SigmaAldrich).
Puromycin(4μg/ml;SigmaAldrich)isaddedtotheBMECmediumforthefirst48hafterplatingtoremovepericytesandincreaseendothelialcellpurity[30].
CulturesBanksetal.
JournalofNeuroinflammation(2015)12:223Page3of15weremaintainedat37°Cinahumidifiedatmosphereof5%CO2/95%air.
Themediumischanged24hafterplatingtoremovenon-adheringcells,redbloodcells,anddebris.
At48hafterplating,themediumwaschangedagainwithanewmediumcontainingallthecomponentslistedabove,exceptpuromycin.
ThepurifiedprimaryBMECswereusedtoconstructinvitromodelswhen80%confluent,typicallythe5thdayafterisolation.
ImmortalizedmousebrainpericytesImmortalizedmousebrainpericytes(ImPCs)werepre-paredaspreviouslydescribed[31].
ImPCsweregrownonuncoatedflasksinlow-glucoseDMEMsupplementedwith2mML-glutamine,10%fetalcalfserum,1%non-essentialaminoacids(LifeTechnologies),andinterferongamma(5.
6ng/ml).
ImPCshavebeenpreviouslycharacterized[31]andstainpositivelyforα-smoothmuscleactin,CD-13,andplatelet-derivedgrowthfactorreceptorβandwerenegativeforfactorVIII.
ImPCswereusedatpassages13–15.
IsolationofprimaryastrocytesMousecerebralastrocyteswereobtainedfromneonatalCD-1mice.
Themeningeswerecarefullyremovedfromcorticesusingadissectingmicroscope.
Then,thecleanedcorticesweremechanicallydissociatedinastrocyteculturemedium.
Astrocytesweregrownonpoly-L-lysine-coated24-wellplatesinhighglucoseDMEM(LifeTechnologies)supplementedwith10%fetalbovineserum.
Constructionofinvitroblood-brainbarriermodelBMECswereculturedalone(monocultures),co-culturedwitheitherpericytesorastrocytes,ortri-culturedwithpericytesandastrocytesaccordingtopreviouslypub-lishedmethods[32].
Thetriple-culturemethodwasadjustedforco-cultureandendothelialcellmonoculturevariants.
Inbrief,immortalizedpericytes(5000cells/well),ifpresent,wereseededonthebottomofapolyes-terTranswellinsert(0.
33cm2,0.
4-μmporesize;CorningInc.
)andallowedtoadherefor4h.
EndothelialcellswerebrieflytrypsinizedandseededontheinsideoftheTranswellinsert,whichwascoatedwithfibronectinandcollagentypeIV(0.
1mg/ml,each),atadensityof4*104cellsperwell.
Theinsertswerethenplacedina24-wellplatecontainingprimaryastrocytes.
Themediumusedtoplatethecellsinthe24-wellTranswellscontainedallthecomponentsoftheBMECmedium,listedabove,withtheadditionof500nMhydrocortisonetoreinforcetightjunc-tions[33].
Themediumintheluminalchamber(ortheinsideoftheTranswellinsert)waschanged24hafterseeding.
BMECmonolayerswereculturedfor3daysbeforeuseinexperiments.
AnEVOMvoltohmmeterequippedwithaSTX-2electrode(WorldPrecisionInstruments;Sarasota,FL)wasusedtomeasuretransendothelialelectricalresistance(TEER,inohmspersquarecentimeter).
TheTEERofcell-freeTranswell-clearinsertswassubtractedfromobtainedvalues.
TEERwasmeasuredpriortotreatmentand24haftertreatment.
TheTEERvaluesre-portedinallfiguresaretheTEERpost-treatment.
TreatmentwithindomethacinandLPSCellswerepre-treatedwith50μlBMEC+HCwithorwithoutindomethacin(200μM).
After30min,50μlBMEC+HCwithorwithoutLPS(20μg/ml)wasaddedtowells.
Cellsweretreatedfor24h(indomethacinfinalconcentration:100μM,LPSfinalconcentration:10μg/ml).
TransendothelialpermeabilityForpermeabilityexperiments,Transwellinsertswerewashedwithserum-freeBMEC+HCmedium+0.
1%BSA.
Thesamemediumwasaddedtothewellsofanew24-wellplate,andthewashedinsertswereplacedinthisplate.
Toinitiatetransportexperiments,14C-sucrose(106cpm/ml)inmediumwasaddedtotheluminalchamber.
Forotherexperiments,99mTc-albumin(106cpm/ml)wasaddedtotheloadingsolutioninadditiontothe14C-sucrose.
Samples(500μl)werecollectedfromtheabluminalchamberat10,20,30,and45min,andwhensampleswereremoved,anequalvolumeoffresh1%BSA/serum-freeBMEC+HCmediumwasimmediatelyaddedtotheabluminalchamber.
Iftheloadingsolutiononlycontained14C-sucrose,liquidscintillationfluidwasaddedtoeachsampleandtheradioactivitywasmeasuredusingaliquidscintillationcounter.
Iftheloadingsolutioncontained99mTc-Alband14C-sucrose,eachsamplewasacidprecipitatedwith30%trichloroaceticacidandcentrifugedat5500*gfor10minat4°C.
Thepelletwascountedinagammacounterforpresenceof99mTc.
Thesupernatantwasremovedandplacedintoscintillationvials.
Liquidscintillationfluidwasaddedtothesupernatantsamplesafter3days,allowingforanyunbound99mTctodecay,andcountedinabetacounter.
Thepermeabilitycoefficientandclearanceofradio-activitywascalculatedaccordingtopreviouslypublishedmethods[34].
Clearancewasexpressedasmicrolitersofradioactivetracerdiffusingfromtheluminaltoablum-inalchamberandwascalculatedusingtheinitialamountofradioactivityintheloadingchamberandthemea-suredamountofradioactivityinthecollectedsamples.
ClearanceμlCCVC=CL;where[C]Listheinitialamountofradioactivitypermicroliterofthesolutionloadedintotheinsert(incountsperminutepermicroliter),[C]Cistheradioactivitypermicroliterinthecollectedsample(incountsperminutepermicroliter),andVCisthevolumeofcollectingBanksetal.
JournalofNeuroinflammation(2015)12:223Page4of15chamber(inmicroliters).
Theclearancevolumeincreasedlinearlywithtime.
Thevolumeclearedwasplottedversustime,andtheslopewasestimatedbylinearregressionanalysis.
TheslopeofclearancecurvesfortheBMECmonolayerplusTranswellmembranewasdenotedbyPSapp,wherePSisthepermeability*surfaceareaproduct(inmicrolitersperminute).
TheslopeoftheclearancecurvewithaTranswellmembranewithoutBMECswasdenotedbyPSmembrane.
TherealPSvaluefortheBMECmonolayer(PSe)wascalculatedfrom1=PSapp1=PSmembrane1=PSe:ThePSevaluesweredividedbythesurfaceareaoftheTranswellinsertstogeneratetheendothelialper-meabilitycoefficient(Pe,inmicrolitersperminutepersquarecentimeter).
ImmunohistochemistryforBMECBMECsgrownonTranswellinsertswerewashedinphosphate-bufferedsaline(PBS)andfixedwith4%PFAfor10minat4°C.
Cellswerepermeabilizedwith0.
1%TRITON-X100,blockedwith5%BSA,andthenincubatedwithanti-ZO-1ratmonoclonalantibody(Millipore,St.
Charles,MO,USA),claudin-5antibody(Abcam,Cambridge,MA),oroccludinantibody(Abcam)followedbyincubationwithAlexaFluor-568-conjugatedsecondaryantibody(Invitrogen,GrandIsland,NY,USA).
InsertsweremountedinantifademediumcontainingDAPI(nuclear)counterstain(SigmaAldrich)andphotographedwithaNikonECLIPSEE800fluorescencemicroscope.
SolubleTREM2ELISAToquantifytheconcentrationsofsolubletriggeringreceptorexpressedonmyeloidcells2(TREM2)extra-cellulardomain(sTREM2)inmouseEDTA-plasmasamples,weadaptedananti-TREM2ELISAsystemsimilartothatreportedbyKleinbergeretal.
[35-37].
ForthedetectionofsTREM2,plateswereincubatedovernightwithpolyclonalsheepanti-TREM2captureantibody(0.
25μg/ml)(R&DSystems,Minneapolis,MN).
Thefollowingdayplateswerewashedthreetimeswithwashingbuffer(0.
05%Tween20inPBS)andblockedin5%BSAand0.
05%Tween20inPBS(pH7.
4)for2hatroomtemperature.
Afterblocking,theplateswerewashedtwiceandloadedwith10μlplasmainto90μlblockingsolutionandincubatedovernight(4°C).
ArecombinantmouseTREM2protein(LifeTechnologies,GrandIsle,NY)wasdilutedinassaybufferinatwofoldserialdilutionandusedforthestandardcurvewithaconcentrationrangeof1000,500,250,125,62,31,15,and0pg/ml.
Thenextday,sampleswereremovedandplateswerewashedthreetimesfor5minwithwashingbufferbeforeincubationfor2hatroomtemperaturewithmousemonoclonalanti-TREM2antibody(1μg/ml)(SantaCruzBiotechnology;B-3)dilutedinblockingbuffer.
Afterthreeadditionalwashingsteps,plateswereincubatedwithanti-mouseHRP-conjugatedsec-ondaryantibody(1:4000)andincubatedfor1hbeforebeingwashedthreetimes.
Followinga30-minincuba-tionwithtetramethylbenzidine,plateswereanalyzedbymeasuringabsorbanceat620nm.
StandardcurvelinearityandinterplateandinterdayvariabilityforthesTREM2ELISAwasdeterminedusingdedicatedplasmasampleanchorsforallplates.
Repeatedfreeze-thawcycleshadnoeffectonsTREM2concentrationsinplasmaaspreviouslyreported[37].
ThespecificityoftheusedELISAsystemwasfurthervalidatedbyanti-TREM2immunoblottingshowingahighdegreeofcorrelationbetweentheELISAreadingsandimmu-noreactivityontheimmunoblotusingtheseantibodiesandanindependentanti-TREM2antibody,mouseanti-TREM22B5(R&DSystems,Minneapolis,MN).
Theplasmawasstoredat70°Cuntilused.
StatisticalanalysisAllstatisticalanalysesandgraphsweregeneratedusingGraphPadPrism5.
0(GraphPadSoftware,Inc.
,LaJolla,CA).
Errorbarsrepresentthestandarderrorofthemean(SEM).
ComparisonoftwomeanswasmadeusingStudent'sttest.
Comparisonofmorethantwogroupswasmadeusingone-wayanalysisofvariance(ANOVA)followedbyNewman-Keulspost-test.
ResultsEffectofLPSonBBBpermeability(singleinjection)Micewerestudied24hafterasingleIPinjectionofLPS.
ThehighestdoseofLPS(3mg/kg)administeredtoCD-1miceproducedasignificantincreaseinBBBpermeabilityasmeasuredwith14C-sucrose(Fig.
1),whereasthelowertwodoseswerewithouteffect.
Therewasasignificantdecreaseintheamountof14C-sucroseintheserum(12.
4±3.
9%injection/mlto8.
4±3.
4%injection/ml),indicatinganincreasedleakageofperipheralcapillarybeds.
IncontrasttoeffectsonBBBpermeability,alldosesofLPSproducedadecreaseinbodyweight(Fig.
2a).
NodoseofLPShadaneffectonbrainweight(Fig.
2b).
Theincreasein14C-sucrosewasevident24h,butnot4h,afteradoseof3mg/kgofLPS(Fig.
2c).
LPSalsoincreasedBBBpermeabilitytoalbumin(Fig.
2d).
TheeffectofLPSdifferedamongbrainregions(Table1).
Eightof11brainregionsshowedastatisticallysignifi-cantincreaseinBBBpermeabilityto14C-sucrose,butthehypothalamus,olfactorybulb,andoccipitalcortexhadarithmeticincreasesthatdidnotreachstatisticalsignificance(Table1).
Allotherstudiesusedthethree-injectionregimenofLPS.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page5of15EffectofNACandindomethacinonLPS-inducedBBBpermeabilityTodeterminewhethertheincreasedBBBpermeabilityinducedbyLPScouldbeblockedbytheadministrationoftheantioxidantNACortheCOXinhibitorindometh-acin,weadministeredtheseagentsintraperitoneally30minpriortotheinjectionsofLPS.
Forthesestudies,thethree-injectionregimenwasusedsoastomatchpreviouslypublishedBBBstudies[6,7,38,39].
AsshowninFig.
3,indomethacin(panelA),butnotNAC(panelB),inhibitedtheLPS-inducedincreaseinBBBpermeabilityto14C-sucrose.
IndomethacinalsopreventedtheLPS-induceddecreaseinbodyweight(datanotshown)ashasbeenpreviouslyreported[6].
NeitherLPSnorindomethacinhasaneffectonZO-1proteinlevelsasmeasuredbyWesternblotting(datanotshown).
EffectsofLPSandindomethacinonbraincytokinesTheeffectsofLPSandindomethacinonbraincytokinesweremeasuredusingaBio-Plexcytokineassaykit.
Ofthe23cytokinesanalyzed,onlyG-CSFandKCwerenotdetectable.
LPSproducedastatisticallysignificantincreaseinbrainlevelsforeightofthecytokines(Table2).
Indo-methacinpreventedanLPS-inducedincreaseofonlytwoofthese(IL-1βandIL-9)butfurtherincreasedlevelsforfourofthem(IL-1α,IL-4,IL-6,andMIP-1).
Forfivecytokines(IL-6,INF-γ,MIP-1α,MIP-1β,andRANTES),theLPS+indomethacin,butnottheLPS-onlygroup,hadincreasedvaluesascomparedtocontrols.
MicroglialandastrocyticactivationFigure4showstheresultsofimmunohistochemicalstainingformicroglia/macrophages(Iba1andF4/80)Fig.
1Dose-dependenceofLPSonBBBpermeabilityto14C-Sucrose.
Onlythe3mg/kgdoseincreasedBBBpermeability.
**pp>0.
05;*p<0.
05;**p<0.
01;***p<0.
001Fig.
3EffectsofindomethacinandN-acetylcysteineonLPS-inducedBBBdisruption.
Panelashowsthatpre-treatmentwithindomethacinpreventedLPS-inducedBBBdisruption(n=7–8/group),whereaspanelbshowsthatN-acetylcysteinewaswithouteffect(9–10/group).
*p<0.
05;**p<0.
01;****p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page7of15fromthoseofamonocultureofBECs.
Figure8showsthatLPSalsoinduceddisruptiontoTc-AlbinBECmonoculturesandthatthisdisruptionwaspartiallyblockedbyindomethacin.
DiscussionInflammation,includinginflammationinducedbyLPS,haslongbeenknowntodisrupttheBBB[3,4,43].
How-ever,manyaspectsofinflammation-inducedBBBdisruptionremainunexplored.
Here,weexaminedmechanismsthatunderlieinflammation-relatedBBBdisruption,beginningwithacharacterizationofthatdisruption.
Wefoundthatincomparisontoinductionofweightloss,ahighdoseofLPSwasrequiredtoinduceinvivoBBBdisruption.
Specifically,3mg/kg,butnot0.
3nor0.
03mg/kg,disruptedtheBBB.
Incontrast,alldosesofLPS,includingtheverylowdoseof0.
03mg/kg,inducedlossofbodyweight.
Bythismeasure,theBBBisresistanttoLPS-induceddisrup-tioninthatarelativelyhighdosewasneededtoinducedisruption.
ThisshowsthatLPScanactivateneuroimmunepathwaysandprocessessuchassick-nessbehaviorwithoutinducingorbeingdependentonBBBdisruption.
Incomparisontotherelativesensitivitytobodyweightloss,brainweightwasnotaffectedevenbythedosethatdisruptedtheBBB.
Thisisnotaltogetherex-pectedasbraindisruptionunderliesvasogenicedema;therefore,adisruptionoftheBBB,ifprolonged,wouldbeexpectedtoleadtobrainedemaand,hence,anincreaseinbrainweight.
BBBdisruptionasmeasuredbytheincreaseinsucrosespacewasnotuniformthroughoutthebrainbutvariedamongbrainregions.
Thehypothalamus,olfactorybulb,andoccipitalcortexhadsmallincreasesthatdidnotreachstatisticalsignificance,whereasthethalamus,frontalcortex,cerebellum,andpons-medullahadin-creasesofover50%.
Thispatterndiffersfromothercausesofdisruption.
Forexample,indiabetesmellitus,BBBdisruptionfirstoccursinthemidbrainwiththecerebellumbeinganarearesistanttodiabetes-inducedBBBdisruption[44].
Thisshowsthatregionalvulnerabil-itiesexistamongregionsoftheBBBbutsuggeststhatthoseregionsvaryasafunctionofinsult.
WefoundtheBBBwasdisruptedtobothalbuminandsucrose.
BBBintegrityisinducedbythreemodificationsofthecapillarybed:aninductionoftightjunctionsthatpreventsintercellular(paracellular)leakage,adecreaseTable2EffectsofindomethacinonLPS-inducedchangesincytokinelevelsinthebrain.
Valuesaremeans±SEMinunitsofpg/mgprotein(n)CytokineSaline(3)LPS(3)LPS+indo(4)SalinevsLPSSalinevsLPS+indoLPSvsLPS+indoIL-1α2.
5±0.
312.
7±1.
917.
9±1.
5indoincreases)IL-1β19.
7±2.
9120.
3±39.
834.
6±3.
2*NS*(indodecreases)IL-215.
8±2.
817.
8±2.
127.
3±3.
3NSNSNSIL-31.
4±0.
22.
1±0.
032.
6±0.
16***NSIL-40.
34±0.
020.
92±0.
081.
1±0.
05indoincreases)IL-50.
93±0.
071.
2±0.
161.
1±0.
1NSNSNSIL-61.
5±0.
1229.
7±16.
572.
8±13.
1NS**(indoincreases)IL-975.
0±3.
1156.
9±16.
489.
2±7.
0**NS**(indodecreases)IL-106.
3±0.
19.
0±0.
310.
4±0.
6****NSIL-12(p40)8.
5±1.
91084±648.
4385.
2±81.
8NSNSNSIL-12(p70)72.
5±6.
5102.
1±3.
197.
6±10.
3NSNSNSIL-1338.
1±2.
340.
0±3.
527.
7±3.
5NSNSNSIL-1719.
4±2.
324.
8±1.
620.
5±0.
9NSNSNSEotaxin2213±131.
52671±99.
82165±144.
3NSNSNSGM-CSF28.
6±2.
547.
1±1.
343.
9±2.
1****NSIFN-γ16.
1±2.
120.
6±1.
122.
9±1.
3NS*NSMCP-133.
0±4.
61550±300.
61612±275.
1****NSMIP-1a6.
8±0.
7128.
3±36.
1465.
2±108.
4NS**(indoincreases)MIP-1b56.
6±3.
5128.
9±15.
7190.
5±37.
0NS*NSRANTES1.
5±0.
3154.
8±37.
7280.
1±57.
3NS**NSTNF-α459.
9±34.
3482.
1±21.
3432.
2±16.
7NSNSNS*p<0.
05;**p<0.
01;***p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page8of15inmacropinocytosis,andalossofintracellularporesandfenestrae.
DisruptionoftheBBBcanbecausedbyreversalofanyorallofthesemodifications.
Sucrose,withamolecularweightof342Da,isthesmallestoftheclassicalvascularmarkersandthusisthemostsensitivefordetectingBBBdisruption.
Albuminatabout65kDaisthelargestoftheclassicalvascularmarkersusedtomeasureBBBdisruptionandthusrequiresamajordisruptionfordetection.
TEER,whichcanbeusedinvitro,requiresapatentchannelfortheexchangeofelec-trolytesbetweentheluminalandabluminalchambers.
AsmallamountofsucrosecrossestheBBBindependentlyofBBBdisruptionbythemechanismoftranscellulardiffusion,andasmallamountofalbuminenterstheCNSprimarilythroughtheextracellularpathways[45].
Hence,controlvaluesforneithersucrosenoralbuminarezero,andthevaluesobtainedhereincontrolmicearethoseexpectedbasedontheirentryratesofabout104ml/g-minforsucroseand105to106ml/g-minforalbumin.
Here,wefoundsignificantdisruptionsoftheBBBasassessedbybothsucroseandalbumininvivoandbyTEER,sucrose,andalbumininvitro.
PreviousworkhassuggestedthatBBBdisruptiontosmallermole-cules,butnotlargermolecules,isindicativeofopeningoftheparacellularrouteonly,whereasdisruptiontolar-gerandsmallermoleculesissuggestiveofopeningofFig.
4EffectsofLPSandindomethacinonmicroglial/macrophageandastrocyticactivation.
Microglial/macrophageactivationwasincreasedbyLPSbutnotblockedbyindomethacinasassessedbyIba1(left-handpanels)andbyF4/80(middlepanels)immunohistochemistry.
AstrocyticactivationwasincreasedbyLPSandblockedbyindomethacinasassessedbyGFAPstaining(right-handpanels).
ThebottomthreepanelsshowquantificationofIba1(n=5–6/statisticalcell),F4/80(n=5–6),andGFAP(n=4–5)immunohistochemicalstaining.
*p<0.
05,**p<0.
01,***p<0.
001,Mag=*20Banksetal.
JournalofNeuroinflammation(2015)12:223Page9of15boththeparacellularandthetranscellularroutes[17,18].
CytoarchitecturaltranslocationofthetightjunctionproteinsZO-1andoccludinalsosupportanincreaseinparacellularpermeability.
Claudin-5didnotshowachangewithLPStreatment,butthismaybebecauseitisthemostdeeplyembeddedofthesetightjunctionpro-teins[46]sothatitwouldbethelasttobetranslocatedinasequentialdisassemblyoftightjunctions.
Takento-gether,theinvivostudiesfindingdisruptiontobothsu-croseandtoalbuminandtheinvitrostudiesassessingTEER,tightjunctionproteinanalysis,andtheperme-abilitytosucroseandtoalbuminsuggestthatLPSre-sultsindisruptionbyboththeparacellularandthetranscellularpathways.
WefoundthatBBBdisruptionwaspresent24hafterinjectionofasingledoseof3mg/kgofLPS,butnot4haftertheinjection.
ArecentstudyhascharacterizedtheeffectofasimilarregimenofLPSonthelevelsof13cytokinesinthebrainandbloodandcanbeusedtoindicatewhichcytokinesarelesslikelytobeinvolvedinBBBdisruption[47].
Itislikelythatthosebraincytokinesnotelevatedateither4or24h(IL-1α,IL-13,IP-10,KC,TNF-α,GM-CSF)arelesslikelytobeinvolvedindisruptionthanthoseelevatedateither4orFig.
5EffectsofLPSplasmaTREM2.
PlasmaTREM2levelsareincreasedbyLPS,aneffectblockedbytreatmentwithindomethacin(n=8/group).
*p<0.
05Fig.
6EffectsofLPSonTEERofBMECsandcytoarchitectureofZO-1,claudin-5,andoccludin.
PanelsaandbshowthatLPSaddedeither24or48hearliertomonoculturesofBMECsdecreasedtheirTEERinadose-dependentmanner,consistentwithdisruptionoftheBBB.
ImmunostainingforZO-1showsincreasingdose-dependentcytoarchitecturaldisorganizationforZO-1(panelsc–f).
Immunostainingforclaudin-5(panelsgandh)doesnotclearlyshowsuchdisorganization,whereasimmunostainingforoccludindoes(panelsiandj).
*p<0.
05;***p<0.
001Banksetal.
JournalofNeuroinflammation(2015)12:223Page10of15Fig.
7(Seelegendonnextpage.
)Banksetal.
JournalofNeuroinflammation(2015)12:223Page11of1524h(IL-1β,IL-6,IL-10,G-CSF,RANTES,MCP-1,MIP-1α).
Likewise,thosebraincytokinesfoundhereinwhichtheindomethacin+LPSgroupdidnotdifferfromtheLPS-onlygroup(Il-2,Il-3,Il-5,Il-10,Il-12(p40),Il-12(p70),Il-13,Il-17,eotaxin,TNF,GM-CSF,interferon-gamma,MCP-1,MIP-1β,RANTES)areunlikelytobeinvolvedinmediatingBBBdisruption.
WethendeterminedtheeffectsoftheantioxidantN-acetylcysteine(NAC)andthenonsteroidalanti-in-flammatorydrugindomethacinonLPS-inducedBBBdis-ruption.
NACrapidlycrossestheBBB[27,48],protectsBECfromoxidativestressinducedbymethamphetamineandantiretroviraldrugs[25,26,48],andreversesthedecreasedbrain-to-bloodtransportofamyloidbetapep-tideinducedbyLPS[27].
IndomethacinasaCOXinhibitordecreasesprostaglandin,prostacyclin,andthromboxanesynthesesandallowsthroughmassactionanincreaseinleukotrienes[49].
ItalsoreversestheeffectofLPSonamyloidbetapeptideefflux[23]andpotentiatesLPS-enhancedtransportofgp120acrosstheBBB[50]butiswithouteffectonLPS-inducedinhibitionofP-glycoproteinfunction[24].
Here,wefoundthatNACwaswithouteffectbutthatindomethacinpreventedLPS-inducedBBBdisruptionto14C-sucrose.
IndomethacinactsbyblockingCOXactivity,thusredu-cingprostaglandinproduction.
ThisstronglyindicatesthatLPSinducesBBBdisruptionthroughaCOX-dependentpathway,possiblyonethatinvolvessecretionofcytokinesfromtheBECs.
ReleaseofprostaglandinsfromBECsisknowntomediatethefeverinducedbyLPS,andindo-methacinattenuatesthatfeverbyblockingprostaglandinsynthesis[51,52].
ThatLPSisactingdirectlyonBECstoinducedisruptionandthatnoothercelltypeisrequiredforLPStoproducedisruptionundertheconditionsoftheseexperimentsareclearlyshownintheinvitrostudies.
AsshowninFig.
6,LPSdisruptedmono-layersofBECs;nocellotherthanBECswasincu-batedinthosemonolayers.
Therefore,LPSmustbeabletodisrupttheBBBbyactingdirectlyonBECs.
LPSisalsoknownfromotherstudiestoinduceneuroinflammation[53];wealsosawLPS-inducedneuroinflammationhereasevidencedbyincreasesinIba1,GFAP,andF4/80immunostainingandinbrainlevelsofeightcytokines.
Therefore,itisreasonabletoassumethatothercomponentsoftheneurovascu-larunit,suchasastrocytesorpericytes,wouldbeinvolvedinpromotingtheLPS-induceddisruptionoftheBBB.
However,wefoundthataddingneither(Seefigureonpreviouspage.
)Fig.
7EffectofLPSandindomethacin(Indo)onTEERand14C-sucrosepermeabilityinmonolayersofBECmonocultures(EOO,n=10),BEC+astrocyteco-cultures(EOA,n=5),BEC+pericyteco-cultures(EPO,n=5),andBEC+pericyte+astrocytetri-cultures(EPA,n=10).
PanelashowsthatinmonoculturesofBECs,LPSincreasedpermeabilitytosucroseandthatindomethacinpartiallyblockedthiseffect.
PanelbshowsthatLPSincreasedpermeabilityofmonolayermonoculturesofBECasmeasuredbyTEERandthatindomethacinhadnoeffectonLPS-inducedpermeability.
Co-culturesofBECswithastrocytes(panelscandd)orpericytes(panelseandf)ortri-culturesofBECswithpericytesandastrocytes(panelsgandh)didnotproduceresultssubstantiallydifferentfromthoseobtainedwithmonoculturesofBECs.
Y-axisis%ControlofPeinunitsofmicrolitersperminutepersquarecentimeter.
*p<0.
05,***p<0.
001;withoutbarcomparestorespective0value;withbarcomparesLPS10μg/mlwithoutindo-methacintoLPS10μg/mlwithindomethacinFig.
8EffectofLPSandindomethacinon14C-sucrose(upperpanel)andTc-Albpermeabilities(lowerpanel)inmonoculturesofBECs.
ResultsshowthatindomethacinpartiallyblockedtheLPS-inducedpermeabilityforbothsucroseandalbumin.
*p<0.
05,***p<0.
001;withoutbarcomparestorespective0value;withbarcomparesindicatedgroupsBanksetal.
JournalofNeuroinflammation(2015)12:223Page12of15pericytesnorastrocytesalteredtheresponseofBECstoLPS.
ThissuggeststhatBECsaloneareinvolvedinBBBdisruptioninourinvitromodel,althoughitisstillpossiblethatothercellscontributetoneuroinflammation-inducedBBBdisruptionunderotherexperimentalcondi-tions.
IncomparisontoLPS-induceddisruptionoftheBBB,LPS-inducedenhancementofinsulintransportacrosstheBBBinvolvesnitricoxidereleasefromnon-BBBcells[54]andLPS-enhancedtransportofHIV-1isenhancedbythepresenceofpericytes[50].
IndomethacinhadmixedeffectsonLPS-inducedin-flammation.
IndomethacindiddecreasetheLPS-inducedelevationinbrainlevelsofIL-1β,IL-9,andplasmaTREM2,thelatterusedasameasureofperipheralin-flammation.
IndomethacindecreasedtheLPS-inducedincreaseinGFAP,suggestingaroleforCOXinastro-cyticactivation,buthadnoeffectontheLPS-inducedincreaseinIba1orF4/80staining,suggestingthatactiva-tionofmicroglia/macrophagesisindependentofCOX.
Additionally,indomethacinfurtherincreasedoverLPSalonethelevelsoffourothercytokines.
Likewise,indomethacinhadamixedeffectonBBBdisruptionasmeasuredinvitro,havingnoeffectondisrup-tionasmeasuredbyTEER,butpartiallyblockingdisruptionasmeasuredbysucroseandalbumin.
BBBdisruptionasmeasuredbyTEERismoreassociatedwithparacellularpathways,whereasBBBdisruptionasmeasuredbysucroseandalbuminisassociatedwithtranscytosis.
ThissuggeststhatalthoughLPSinducesdisruptionbybothparacellularandtranscytoticpathways,theparacellularpathwayisme-diatedthroughCOX-independentmechanisms.
Thereareseveralimplicationsofthiswork.
First,althoughLPSisnotatruesepsismodel,itdoessuggestthatCOXinhibitionwouldbeprotectiveagainsttheBBBdisruptionseeninsepsisandinotherinflammatorystates.
Additionally,itisincreasinglyclearthatLPSentersthecirculationnotonlyindiseasestatessuchastheleakygutofAIDS[55]butalsoundermorephysio-logicconditions,suchasafteringestionofahigh-fatmealormarathonrunning[56,57].
ThelatterstudiessuggestthatLPSmayhaverolesinneuroimmunemodu-lationthatarenotstrictlypathological.
Forexample,LPSislikelyoneofthemediatorsresponsibleforthedifferentialresponseoftissues,includingthebrain,tohealthyandpathologicmicrobiomes[58,59].
ThesestudiesfoundthathighdosesofLPSarerequiredtodisrupttheBBBwhentheLPSexposureisacutebutdidnotinvestigatetheeffectsofchronic,low-doseexposuretoLPSonBBBintegrity.
ConclusionsTheseresultsshowthattheBBBisrelativelyresistanttodisruptionbyLPSincomparisontoanotherclassiceffectofLPS,thatofweightloss.
NotallregionsoftheBBBareequallysensitivetoLPS-inducedBBBdisrup-tion,involvementofnon-BECsisnotrequiredforLPStoinducedisruption,anddisruptionoccursthroughbothparacellularandtranscytoticmechanismswithtranscytoticdisruptionbeingprostaglandin-dependent.
AbbreviationsBBB:blood-brainbarrier;BECs:brainendothelialcells;BMECs:brainmicrovascularendothelialcells;BSA:bovineserumalbumin;COX:cyclooxygenase;I-Alb:iodine-labeledalbumin;IL:interleukin;ImPCs:immortalizedmousebrainpericytes;LPS:lipopolysaccharide;NAC:N-acetylcysteine;Tc-Alb:technetium-labeledalbumin;TEER:transendothelialelectricalresistance;TREM2:triggeringreceptorexpressedonmyeloidcells2.
CompetinginterestsNoauthorhasafinancialornon-financialcompetinginterest.
Authors'contributionsWilliamA.
Banks:conceivedoverallapproachandquestion,performedmostoftheexperimentaldesign,andwrotetheMS.
AliciaM.
Gray,MichelleA.
Erickson,andThereseS.
Salameh:conductedinvivostudiesandcontributedtoinvivoexperimentaldesign.
MamathaDamodarasamyandMayJ.
Reed:IHC.
NaderSheibani:providedimmortalizedpericytes.
JamesS.
MeabonandDavidG.
Cook:TREM2assays.
EmilyE.
WingandYoichiMorofuji:invitroassays.
Allauthorsreadandapprovedthefinalmanuscript.
AcknowledgementsWewouldliketothankDr.
JessicaHamerman(UniversityofWashington)forTREM2KOmousematerialsandtheratanti-TREM2antibody.
SupportedbytheVAandR01AG029839(WAB).
Authordetails1GeriatricResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA.
2DivisionofGerontologyandGeriatricMedicine,DepartmentofInternalMedicine,UniversityofWashingtonSchoolofMedicine,Seattle,WA,USA.
3UniversityofWashingtonSchoolofMedicine,Seattle,WA,USA.
4OphthalmologyandVisualSciences,UniversityofWisconsinSchoolofMedicineandPublicHealth,Madison,WI,USA.
5MentalHealthResearchEducationandClinicalCenter-VAPugetSoundHealthCareSystem,Seattle,WA,USA.
6DepartmentofNeurosurgery,UniversityofNagasaki,Nagasaki,Japan.
Received:13July2015Accepted:14November2015References1.
SkoogT.
Onthevitalstainingofthecentralnervoussystem.
ActaOtolaryngologica.
1937;25:365–78.
2.
RapoportSI.
Pathologicalalterationsoftheblood-brainbarrier.
In:Blood-brainbarrierinphysiologyandmedicine.
NewYork:Raven;1976.
p.
129–52.
3.
AllenIV.
Theeffectofbacterialpyrogenontheblood-brainbarrierfortrypanblue.
JPatholBacteriol.
1965;89:481–94.
4.
EckmanPL,KingWM,BrunsonJG.
Studiesonthebloodbrainbarrier.
I.
Effectsproducedbyasingleinjectionofgram-negativeendotoxinonthepermeabilityofthecerebralvessels.
AmJPathol.
1958;34:631–43.
5.
PersidskyY,StinsM,WayD,WitteMH,WeinandM,KimKS,etal.
Amodelformonocytemigrationthroughtheblood-brainbarrierduringHIV-1encephalitis.
JImmunol.
1997;158:3499–510.
6.
BanksWA,KastinAJ,BrennanJM,VallanceKL.
AdsorptiveendocytosisofHIV-1gp120byblood-brainbarrierisenhancedbylipopolysaccharide.
ExpNeurol.
1999;156:165–71.
7.
XaioH,BanksWA,NiehoffML,MorleyJE.
EffectofLPSonthepermeabilityoftheblood-brainbarriertoinsulin.
BrainRes.
2001;896:36–42.
8.
MinamiT,OkazakiJ,KawabataA,KurodaR,OkazakiY.
Penetrationofcisplatinintomousebrainbylipopolysaccharide.
Toxicology.
1998;130:107–13.
9.
PanW,YuC,HsuchouH,ZhangY,KastinAJ.
NeuroinflammationfacilitatesLIFentryintobrain:roleofTNF.
AmJPhysiolCellPhysiol.
2008;294:C1436–42.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page13of1510.
TucsekZ,TothP,SosnowskaD,GautamT,MitschelenM,KollerA,etal.
Obesityinagingexacerbatesblood-brainbarrierdisruption,neuroinflammation,andoxidativestressinthemousehippocampus:effectsonexpressionofgenesinvolvedinbeta-amyloidgenerationandAlzheimer'sdisease.
JGerontolABiolSciMedSci.
2013,epub.
11.
SengilloJD,WinklerEA,WalkerCT,SullivanJS,JohnsonM,ZlokovicBV.
Deficiencyinmuralvascularcellscoincideswithblood-brainbarrierdisruptioninAlzheimer'sdisease.
BrainPathol.
2012;23:303–10.
12.
StarrJM,WardlawJ,FergusonK,MacLullichA,DearyIJ,MarshallI.
Increasedblood-brainbarrierpermeabilityintypeIIdiabetesdemonstratedbygadoliniummagneticresonanceimaging.
JNeurolNeurosurgPsychiatry.
2003;74:70–6.
13.
AbrahamCS,HaradaN,DeliMA,NiwaM.
Transientforebrainischemiaincreasestheblood-brainbarrierpermeabilityforalbumininstroke-pronespontaneouslyhypertensiverats.
CellMolNeurobiol.
2003;22:455–62.
14.
PozzilliC,BernardiS,MansiL,PicozziP,IannottiF,AlfanoB,etal.
Quantitativeassessmentoftheblood-brainbarrierpermeabilityinmultiplesclerosisusing68-Ga-EDTAandpositronemissiontomography.
JNeurolNeurosurgPsychiatry.
1988;51:1058–62.
15.
ReeseTS,KarnovskyMJ.
Finestructurallocalizationofablood-brainbarriertoendogenousperoxidase.
JCellBiol.
1967;34:207–17.
16.
BrightmanMW,ReeseTS.
Junctionsbetweenintimatelyapposedcellmembranesinthevertebratebrain.
JCellBiol.
1969;40:648–77.
17.
MayhanWG,HeistadDD.
Permeabilityofblood-brainbarriertovarioussizedmolecules.
AmJPhysiology.
1985;248:H712–8.
18.
ZiylanYZ,RobinsonPJ,RapoportSI.
Blood-brainbarrierpermeabilitytosucroseanddextranafterosmoticopening.
AmJPhysiol.
1984;247:R634–8.
19.
KnowlandD,AracA,SekiguchiKJ,HsuM,LutzSE,PerrinoJ,etal.
Stepwiserecruitmentoftranscellularandparacellularpathwaysunderliesblood-brainbarrierbreakdowninstroke.
Neuron.
2014;82:603–17.
20.
Fleegal-DeMottaMA,DohguS,BanksWA.
AngiotensinIImodulatesBBBpermeabilityviaactivationoftheAT1receptorinbrainendothelialcells.
JCerebBloodFlowMetab.
2009;29:640–7.
21.
DeVriesHE,Blom-RoosemalenMCM,DeBoerAG,vanBerkelTJ,BreimerDD,KuiperJ.
Effectofendotoxinonpermeabilityofbovinecerebralendothelialcelllayersinvitro.
JPharmacolExpTher.
1996;277:1418–23.
22.
MinamiT,OkazakiJ,KawabataA,KawakiH,OkazakiY,TohnoY.
Rolesofnitricoxideandprostaglandinsintheincreasedpermeabilityoftheblood-brainbarriercausedbylipopolysaccharide.
EnvironToxicolPharmacol.
1998;5:35–41.
23.
JaegerJB,DohguS,LynchJL,Fleegal-DeMottaMA,BanksWA.
Effectsoflipopolysaccharideontheblood-brainbarriertransportofamyloidbetaprotein:amechanismforinflammationintheprogressionofAlzheimer'sdisease.
BrainBehavImmun.
2009;23:507–17.
24.
SalkeniMA,LynchJL,PriceTO,BanksWA.
Lipopolysaccharideimpairsblood-brainbarrierP-glycoproteinfunctioninmicethroughprostaglandin-andnitricoxide-independentpathwaysandnitricoxide-independentpathways.
JNeuroimmunePharmacology.
2009;4:276–82.
25.
ZhangX,BanerjeeA,BanksWA,ErcalN.
N-acetylamideprotectsagainstmethamphetamine-inducedoxidativestressandneurotoxicityinimmortalizedhumanbrainendothelialcells.
BrainRes.
2009;1275:87–95.
26.
MandaKR,BanerjeeA,BanksWA,ErcalN.
Highlyactiveantiretroviraltherapydrugcombinationinducesoxidativestressandmitochondrialdysfunctioninimmortalizedhumanblood-brainbarrierendothelialcells.
FreeRadicBiolMed.
2011;50:801–10.
27.
EricksonMA,HansenK,BanksWA.
Inflammation-induceddysfunctionofthelow-densitylipoproteinreceptor-relatedprotein-1attheblood-brainbarrier:protectionbytheantioxidantN-acetylcysteine.
BrainBehavImmun.
2012;26:1085–94.
28.
CoisneC,DehouckL,FaveeuwC,DelplaceY,MillerF,LandryC,etal.
Mousesyngenicinvitroblood-brainbarriermodel:anewtooltoexamineinflammatoryeventsincerebralendothelium.
LabInvest.
2005;85:734–46.
29.
JacobA,HackB,ChiangE,GarciaJG,QuiggRJ,AlexanderJJ.
C5aaltersblood-brainbarrierintegrityinexperimentallupus.
FASEBJ.
2010;24:1682–8.
30.
PerriereN,DemeuseP,GarciaE,ReginaA,DebrayM,AndreuxJP,etal.
Puromycin-basedpurificationofratbraincapillaryendothelialcellcultures.
JNeurochem.
2005;93:279–89.
31.
ShahGN,PriceTO,BanksWA,MorofujiY,KovacA,ErcalN,etal.
Pharmacologicalinhibitionofmitochondrialcarbonicanhydrasesprotectsmousecerebralpericytesfromhighglucose-inducedoxidativestressandapoptosis.
JPharmacolExpTherap.
2013;344:637–45.
32.
NakagawaS,DeliMA,KawaguchiH,ShimizudaniT,ShimonoT,KittelA,etal.
Anewblood-brainbarriermodelusingprimaryratbrainendothelialcells,pericytesandastrocytes.
NeurochemInt.
2009;54:253–63.
33.
HoheiselD,NitsT,FrankeH,WegenerJ,HakvoortA,TillingT,etal.
Hydrocortisonereinforcestheblood-brainbarrierpropertiesinaserumfreecellculturesystem.
BiochemBiophysResCommun.
1998;217:312–5.
34.
DehouckMP,Jolliet-RiantP,BreeF,FruchartJC,CecchelliR,TillementJP.
Drugtransferacrosstheblood-brainbarrier:correlationbetweeninvitroandinvivomodels.
JNeurochem.
1992;58:1790–7.
35.
ScimemiA,MeabonJS,WoltjerRL,SullivanJM,DiamondJS,CookDG.
Amyloid-β1-42slowsclearanceofsynapticallyreleasedglutamatebymislocalizingastrocyticGLT-1.
JNeurosci.
2013;33:5312–8.
36.
DawsMR,LanierLL,SeamanWE,RyanJC.
CloningandcharacterizationofanovelmousemyeloidDAP12-associatedreceptorfamily.
EurJImmunol.
2001;31:783–91.
37.
KleinbergerG,YamanishiY,Suarez-CalvetM,CzirrE,LohmannE,CuyversE,etal.
TREM2mutationsimplicatedinneurodegenerationimpaircellsurfacetransportandphagocytosis.
SciTranslMed.
2014;6:243ra286.
38.
NonakaN,ShiodaS,BanksWA.
Effectoflipopolysaccharideonthetransportofpituitaryadenylatecyclaseactivatingpolypeptideacrosstheblood-brainbarrier.
ExpNeurol.
2005;191:137–44.
39.
EricksonMA,HartvigsonPE,MorofujiY,OwenJB,ButterfieldDA,BanksWA.
Lipopolysaccharideimpairsamyloidbetaeffluxfrombrain:alteredvascularsequestration,cerebrospinalfluidreabsorption,peripheralclearanceandtransporterfunctionattheblood-brainbarrier.
JNeuroinflammation.
2012;9:150.
40.
TurnbullIR,GilfillanS,CellaM,AoshiT,MillerMC,PiccioL,etal.
Cuttingedge:TREM-2attenuatesmacrophageactivation.
JImmunol.
2006;177:3520–4.
41.
HamermanJA,JarjouraJR,HumphreyMB,NakamuraMC,SeamanWE,LanierLL.
Cuttingedge:inhibitionofTLRandFcRresponsesinmacrophagesbytriggeringreceptorexpressedonmyeloidcells(TREM0-2andDAP12).
JImmunol.
2006;177:2051–5.
42.
SchmidCD,MelchiorB,MasekK,PuntambekarSS,DanielsonPE,LoDD,etal.
DifferentialgeneexpressioninLPS/IFNgammaactivatedmicrogliaandmacrophages:invitroversusinvivo.
Neurochem.
2009;109Suppl1:117–25.
43.
WispelweyB,LesseAJ,HansenEJ,ScheldWM.
Haemophilusinfluenzaelipopolysaccharide-inducedbloodbrainbarrierpermeabilityduringexperimentalmeningitisintherat.
JClinInvestig.
1988;82:1339–46.
44.
HuberJD,VanGilderRL,HouserKA.
Streptozotocin-induceddiabetesprogressivelyincreasesblood-brainbarrierpermeabilityinspecificbrainregionsinrats.
AmJPhysiol.
2006;291:H2660–8.
45.
KimYS,LeeMH,WisniewskiHM.
Aluminuminducedreversiblechangeinpermeabilityoftheblood-brainbarrierto[14C]sucrose.
BrainRes.
1986;377:286–91.
46.
BrownRC,DavisTP.
Calciummodulationofadherenstightjunctionfunction:apotentialmechanismforblood-brainbarrierdisruptionafterstroke.
Stroke.
2002;33:1706–11.
47.
EricksonMA,BanksWA.
Cytokineandchemokineresponsesinserumandbrainaftersingleandrepeatedinjectionsoflipopolysaccharide:multiplexquantificationwithpathanalysis.
Brain,Behavior,&Immunity.
2011;25:1637–48.
48.
FarrSA,PoonHF,Dogrukol-AkD,DrakeJ,BanksWA,EyermanE,etal.
Theantioxidantsalpha-lipoicacidandN-acetylcysteinereversememoryimpairmentandbrainoxidativestressinagedSAMP8mice.
JournalofNeurochemisrty.
2003;84:1173–83.
49.
VaneJR,BottingRM.
Mechanismofactionofanti-inflammatorydrugs.
AdvExpMedBiol.
1997;433:133–8.
50.
DohguS,BanksWA.
Lipopolysaccharide-enhancedtranscellulartransportofHIV-1acrosstheblood-brainbarrierismediatedbythep38mitogen-activatedproteinkinasepathway.
ExpNeurol.
2008;210:740–9.
51.
EngstromL,RuudJ,EskilssonA,LarssonA,MackerlovaL,KugelbergU,etal.
Lipopolysaccharide-inducedfeverdependsonprostaglandinE2productionspecificallyinbrainendothelialcells.
Endocrinology.
2012;153:4849–61.
52.
InoueW,MatsumuraK,YamagataK,TakemiyaT,ShirakiT,KobayashiS.
Brain-specificendothelialinductionofprostaglandinE(2)synthesisenzymesanditstemporalrelationtofever.
NeurosciRes.
2002;44:51–61.
53.
QinL,WuX,BlockML,LiuY,BreeseGR,HongJS,etal.
SystemicLPScauseschronicneuroinflammationandprogressiveneurodegeneration.
Glia.
2007;55:453–62.
Banksetal.
JournalofNeuroinflammation(2015)12:223Page14of1554.
BanksWA,DohguS,NakaokeR,LynchJL,Fleegal-DeMottaMA,EricksonMA,etal.
NitricoxideisoenzymesregulateLPS-enhancedinsulintransportacrosstheblood-brainbarrier.
Endocrinology.
2008;149:1514–23.
55.
BrenchleyJM,PriceDA,SchackerTW,AsherTE,SilvestriG,RaoS,etal.
MicrobialtranslocationisacauseofsystemicimmuneactivationinchronicHIVinjection.
NatMed.
2006;12:1365–71.
56.
NgQY,LeeKW,ByrneC,HoTF,LimCL.
Plasmaendotoxinandimmuneresponsesduringa21-kmroadraceunderawarmandhumidenvironment.
AnnAcadMedSingapore.
2008;37:307–14.
57.
AmarJ,BurcelinR,RuidavetsJB,CaniPD,FauvelJ,AlessiMC,etal.
Energyintakeisassociatedwithendotoxemiainapparentlyhealthymen.
AmJClinNutr.
2008;87:1219–23.
58.
JasarevicE,HowertonCL,HowardCD,BaleTL.
Alterationsinthevaginalmicrobiomebymaternalstressareassociatedwithmetabolicreprogrammingoftheoffspringgutandbrain.
Endocrinology.
2015;156:3265–76.
59.
BanksWA.
Avaginamonologue:mom'sstress,bugs,andbaby'sbrain.
Endocrinology.
2015;156:3066–8.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Banksetal.
JournalofNeuroinflammation(2015)12:223Page15of15
- fibroblastbluestack相关文档
- definedbluestack
- handlesbluestack
- textboxbluestack
- underlyingbluestack
- 支援全部的產品線
- errorbluestack
咖啡主机22元/月起,美国洛杉矶弹性轻量云主机仅13元/月起,高防云20G防御仅18元/月
咖啡主机怎么样?咖啡主机是一家国人主机销售商,成立于2016年8月,之前云服务器网已经多次分享过他家的云服务器产品了,商家主要销售香港、洛杉矶等地的VPS产品,Cera机房 三网直连去程 回程CUVIP优化 本产品并非原生地区本土IP,线路方面都有CN2直连国内,机器比较稳定。咖啡主机目前推出美国洛杉矶弹性轻量云主机仅13元/月起,高防云20G防御仅18元/月;香港弹性云服务器,香港HKBN CN...

虎跃云-物理机16H/32G/50M山东枣庄高防BGP服务器低至550元每月!
虎跃科技怎么样?虎跃科技(虎跃云)是一家成立于2017年的国内专业服务商,专业主营云服务器和独立服务器(物理机)高防机房有着高端华为T级清洗能力,目前产品地区有:山东,江苏,浙江等多地区云服务器和独立服务器,今天虎跃云给大家带来了优惠活动,为了更好的促销,枣庄高防BGP服务器最高配置16核32G仅需550元/月,有需要的小伙伴可以来看看哦!产品可以支持24H无条件退款(活动产品退款请以活动规则为准...

快云科技,免云服务器75折优惠服务器快云21元/月
近日快云科技发布了最新的夏季优惠促销活动,主要针对旗下的香港CN2 GIA系列的VPS云服务器产品推送的最新的75折优惠码,国内回程三网CN2 GIA,平均延迟50ms以下,硬件配置方面采用E5 2696v2、E5 2696V4 铂金Platinum等,基于KVM虚拟架构,采用SSD硬盘存储,RAID10阵列保障数据安全,有需要香港免备案CN2服务器的朋友可以关注一下。快云科技怎么样?快云科技好不...
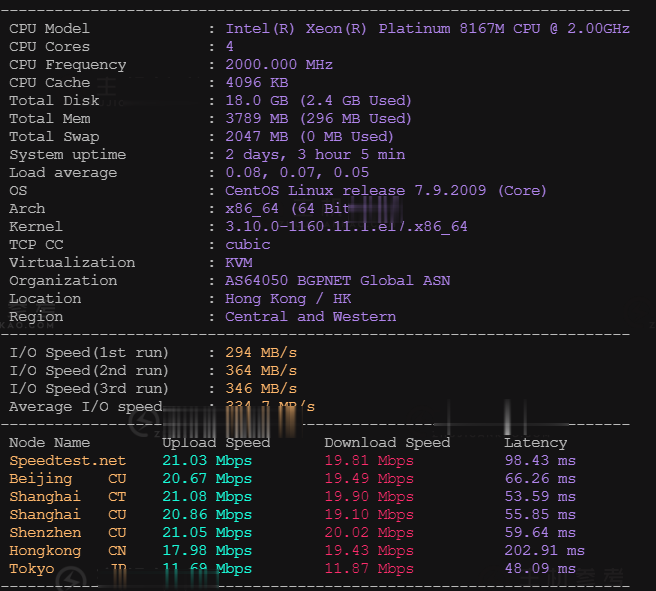
bluestack为你推荐
-
郭彩妮介紹點好聽的音樂給我、大家湖南商标注册湖南商标注册怎么办理雅虎社区有什么网站的论坛内容丰富 资讯较新 适合年轻人的?依赖注入依赖注入是什么意思?手机区号手机号码前怎样填写正确的国内区号?网店推广网站可以介绍几个可以做店铺推广的网站吗?苹果5怎么越狱苹果5怎么越狱?直播加速怎么让已拍摄好的视频加速mate8价格现在买华为mate8高配划算吗网页打开很慢为什么我打开网页很慢