higherapche
apche 时间:2021-01-17 阅读:()
RESEARCHARTICLEOpenAccessPrognosticsignificanceofAPACHEIIscoreandplasmasuPARinChinesepatientswithsepsis:aprospectiveobservationalstudyXuanLiu,YongShen,ZhihuaLi,AihuaFei,HairongWang,QinminGeandShumingPan*AbstractBackground:Timelyriskstratificationisthekeystrategytoimproveprognosisofpatientswithsepsis.
PreviousstudyhasproposedtodevelopapowerfulriskassessmentrulebythecombinationofAcutePhysiologyandChronicHealthEvaluationII(APACHEII)scoreandplasmasolubleurokinaseplasminogenactivatorreceptor(suPAR).
ThatreaffirmationofsuPARasaprognosticmarkerinChinesepatientswithseveresepsisistheaimofthestudy.
Methods:Atotalof137consecutiveChinesepatientswithsepsiswereenrolledinaprospectivestudycohort.
Demographicandclinicalcharacteristics,conventionalriskfactorsandimportantlaboratorydatawereprospectivelyrecorded.
SequentialplasmasuPARconcentrationsweremeasuredbyanenzymeimmunoabsorbentassayondays1,3,and7afteradmissiontotheintensivecareunit(ICU).
Receiveroperatingcharacteristic(ROC)curvesandCoxregressionanalysiswereusedtoexaminetheperformanceofsuPARindevelopingaruleforriskstratification.
Results:TheresultsshowedthatplasmasuPARconcentrationsremainedrelativelystablewithinsurvivorsandnon-survivorsduringthefirstweekofdiseasecourse.
RegressionanalysisindicatedthatAPACHEII≥15andsuPAR≥10.
82ng/mLwereindependentlyassociatedwithunfavorableoutcome.
WiththeabovecutoffsofAPACHEIIandsuPAR,strataofdiseaseseverityweredetermined.
Themortalityofeachstratumdifferedsignificantlyfromtheothers.
Conclusions:CombinationofAPACHEIIscoreandsuPARmaysupplythepowerfulprognosticutilityforthemortalityofsepsis.
Keywords:Sepsis,Riskstratification,Solubleurokinaseplasminogenactivatorreceptor(suPAR),AcutePhysiologyandChronicHealthEvaluationII(APACHEII)BackgroundTheincidenceofsepsisinadultshasbeenincreasing,withseveresepsisandsepticshockremainingamongthemajorcausesofdeathworldwide[1].
Despitethemortalityisonadecliningtrendinrecentyears[2],lowawareness,laterecognition,andimpropertreatmentarestillcommon[3].
Oneofthefundamentalprinciplesfortheappropriatemanagementofsepsisistimelydiscriminationofthepa-tientsathighriskfordeath[4].
Thisisgenerallydependentontheapplicationofscoresystemsandplasmabiomarkers.
Althoughthewell-recognizedscoreistheAcutePhysiologyandChronicHealthEvaluationII(APACHEII),APACHEIIscorehassomepotentialpitfallsthatmayleadtoinaccurateevaluation.
Takeyoungpatientswithseveresepsisbutwithoutchronicorgandysfunctionforinstance,theAPACHEIIscoremayberelativelylowdespitetheriskforanunfavorableoutcomeishigh[5].
Althoughvariousbiologicalmarkersarewidelyex-plored[6–9],onlyafewhavebeenappliedintheclinicalpractice.
Thesolubleurokinaseplasminogenactivatorreceptor(suPAR),whichexistsinthreeforms(I-III,II-IIIandI),isregardedasanovelbiomarkerofimmunesystemactivation[10].
Urokinaseplasminogenactivator*Correspondence:drshumingpan@hotmail.
comDepartmentofEmergency,XinhuaHospital,ShanghaiJiaotongUniversitySchoolofMedicine,1665KongjiangRoad,Shanghai200092,China2016Liuetal.
OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Liuetal.
BMCAnesthesiology(2016)16:46DOI10.
1186/s12871-016-0212-3receptor(uPAR)isembeddedinthecellmembranesofvariousimmunologicallyactivecellsand,withitsligand,urokinaseplasminogenactivator(uPA),takespartinarangeofimmunologicactivities[11].
Uponinflammatorystimulation,uPARiscleavedfromthecellsurfacebyproteasesintothesolubleformofthereceptor-suPAR-whichcanbeassessedinblood,urine,bronchoalveolarlavage,andcerebrospinalfluid[12,13].
RecentstudieshaverevealedthatsuPARmayhavetheabilitytopredictthemortalityofsepsis[14–17].
ItisnoteworthythatGiamarellos-Bourboulisetal.
haveproposedanewprog-nosticationruleforpredictingtheoutcomeofsepsisbyAPACHEIIscoreandsuPAR[5].
Theprimarypurposeofthepresentstudywastofur-therreaffirmthepredictionruleforthemortalityinChinesepatientswithsepsisbycombiningAPACHEIIscoreandplasmasuPARconcentrations.
MethodsStudydesignThisprospectivetrialinvolvedconsecutiveChinesepa-tientswithsepsispresentingtotheintensivecareunit(ICU)oftheDepartmentofEmergency,XinhuaHos-pital,ShanghaiJiaotongUniversitySchoolofMedicine,fromMarch2013toFebruary2015.
Foreachpatientwithsuspectedinfection,acompletediagnosticwork-upwasperformed.
Thework-upcom-priseddemographicandclinicalcharacteristics,conven-tionalriskfactors,andimportantlaboratorydataincludingbloodroutineexamination,microbiologicalculturing,chestx-ray,andchestorabdominalcomputedtomographyifnecessary.
Broadspectrumantimicrobialtreatmentwasusedwithin1hfromtherecognitionofthesepticstatus.
Patientswereeligibleiftheymettheinclusioncriteria:(1)ageofatleast18years;(2)sepsisduetooneofthefollowinginfections:communityacquiredpneumonia,hospitalacquiredpneumonia,ventilator-associatedpneumonia,acutepyelonephritis,intra-abdominalinfec-tion,orprimarybacteremia;and(3)bloodsamplingwithin24hfromthepresentationofsignsofsepsis.
Pa-tientsaffectedbyadvancedcancerorterminalpatientswithotherpathologieswereexcluded.
Alleligiblepatientswerefurtherclassifiedaccordingtostandarddefinitionsofsepsis,severesepsis,andsepticshock[18].
Morespecifically,sepsiswasdefinedasthepresenceofsuspectedorconfirmedinfectiontogetherwithtwoormorecriteriaforasystemicinflammatoryresponse;severesepsiswasdefinedassepsiswithsepsis-inducedorgandysfunction,hypotensionorhypoperfusion;septicshockwasde-finedasrefractoryhypotensionorhypoperfusiondes-pitesufficientfluidresuscitation.
BloodmeasurementsVenousblood(3mL)wascollectedfrompatientspre-sentingtotheICU(day1)andrepeatedonthefollowingday3andday7afteradmission.
WholebloodwasdrawnintoacentrifugetubecontainingEDTAanti-coagulant.
Aftercentrifugationat3,000gfor10minat4°C,plasmasampleswerekeptfrozenat80°Cuntilassayed.
suPARwasdeterminedinduplicatebyacom-mercialdoublemonoclonalantibodysandwichenzymeimmunoassay(suPARnosticStandardkit;ViroGatesA/S,Birkerd,Denmark)inaccordancewiththeinstructionsofthemanufacturer.
Every45bloodsam-plescanbemeasuredwithinabout4h.
Thelinearityofthisassayiscomprisedbetween2.
0and15.
6ng/mL,andthetotalimprecision,expressedascoefficientofvari-ation(CV%),rangesfrom2.
3to6.
0%.
StudyoutcomesPatientswhosurvivedwerefurtherfollowedupbytele-phonecalls.
Theunfavorableoutcomeofthestudywasdefinedasdeathfromanycausewithin28daysafterad-missiontotheICU.
StatisticalanalysisContinuousvariableswerepresentedasmeanvalues±standarddeviation(SD)ormedianwithinterquartileranges(IQR),whilecategoricalvariableswereexpressedasper-centages.
Thestatisticalsignificanceofintergroupdiffer-enceswascomparedthroughunpairedStudent'st-testorMann–WhitneyUtestforcontinuousvariablesandthroughPearson'sχ2testforcategoricalvariables.
Thefollowingstepswereperformedtoestablishariskstratificationrule:First,receiveroperatingcharacteristic(ROC)analysiswasconductedwithbaselinelevelsofAPACHEIIscoreandsuPARtodeterminethepredic-tionsensitivityandspecificityofthevariables.
Second,weusedunivariateandmultivariateCoxregressionana-lysestocalculatehazardratios(HR)with95%confi-denceintervals(CIs).
Third,strataofdiseaseseveritywereestablishedusingthecutoffsofAPACHEIIscoreandsuPAR.
Oddsratios(OR)and95%CIsforriskpre-dictionwithineachstratumwereassessedusingMantelandHaenszelstatistics.
Fourth,mortalitiesbetweenstratawereestimatedusingthelog-ranktest.
Atwo-sidedPvalue<0.
05wasconsideredstatisti-callysignificant.
AllanalyseswereperformedbytheIBMSPSSStatisticssoftwareversion19.
0(SPSS,Chi-cago,IL,USA).
ResultsBaselinecharacteristicsofthestudypopulationAtotalof137consecutivepatients(51.
09%men;meanage,69.
53±9.
28years)wereeligibleforenrollmentinthestudy.
AftertheinitialevaluationperformedintheLiuetal.
BMCAnesthesiology(2016)16:46Page2of9ICU,patientsweredividedintothreegroupsaccord-ingthediseaseseverity:group1,patientswithsepsis(n=56);group2,thosewithseveresepsis(n=49);andgroup3,thosewithsepticshock(n=32).
ThebaselineclinicalandlaboratorycharacteristicsofthepatientsareelaboratedinTable1.
Themostcommonlocationsofinfectionwerelungandurinarytract,andthedistributionoflocationswassimilaramongthethreegroups.
ThecommonestisolatedpathogensfromthestudycohortwereGram-negativemicroor-ganismswithapredominanceofEscherichiacoli,andbloodcultureswerepositivein43.
80%ofallpatients.
Therewasnotanydifferenceinpathogenstrainsamongthedifferentgroups(Table1).
Therewerenosignificantlystatisticaldifferencesinpa-tientswithsepsiscomparedtothoseinseveresepsisorsepticshockforgenderorage.
Patientswithseveresep-sisorsepticshocktendedtohavehigherbaselinelevelsTable1BaselineclinicalandlaboratorycharacteristicsofthestudysubjectsPatientgroupCharacteristicsSepsisSeveresepsisSepticshockPvalueDemographicsandunderlyingconditionsNumberofpatients564932-Males,no.
(%)29(51.
79%)27(55.
10%)14(43.
75%)0.
418Age(years),mean±SDCOPD,no(%)Hypertension,no(%)Diabetesmellitus,no(%)68.
04±9.
3620(35.
71%)23(41.
07%)9(16.
07%)71.
39±8.
8524(48.
98%)23(46.
94%)9(18.
37%)69.
16±9.
7319(59.
38%)17(53.
13%)7(21.
88%)0.
2460.
032*0.
4730.
381Baselineparameters,mean±SDAPACHEIIscoreSOFAscore9.
87±3.
125.
26±2.
0912.
50±4.
757.
83±2.
5318.
34±6.
0911.
42±3.
740.
001**0.
002**SuPAR(ng/mL)PCT(ng/mL)Whitebloodcellcount(109/L)6.
58±3.
176.
14±3.
5411.
96±2.
8668.
62±4.
8011.
05±4.
6018.
26±3.
9815.
97±5.
4427.
69±7.
2826.
67±7.
040.
001**<0.
001**0.
037*Lacticacid(mmol/L)1.
75±1.
163.
27±1.
486.
03±3.
820.
012*BUN(mmol/L)Scr(μmol/L)ALT(U/L)AST(U/L)Bilirubin(mg/dL)Platelet(109/L)Plasmaglucose(mmol/L)Hemoglobin(g/L)6.
42±3.
8570.
32±19.
5631.
23±10.
2732.
95±11.
0214.
60±8.
03154.
19±71.
527.
25±4.
89109.
84±33.
149.
05±4.
13103.
59±31.
0745.
62±16.
4460.
38±21.
3716.
23±9.
15134.
08±75.
178.
35±5.
18117.
08±20.
4911.
91±9.
39154.
08±40.
87153.
89±48.
01196.
35±65.
2920.
01±9.
66127.
60±65.
9510.
02±7.
11118.
05±20.
650.
017*0.
021*0.
013*0.
009**0.
6940.
7410.
3890.
436Pathogenstrains,no(%)0.
058EscherichiacoliKlebsiellapneumoniaPseudomonasaeruginosaAcinetobacterbaumanniiOtherGram-negativebacteriaStaphylococcusaureusEnterococcusspp6(10.
71%)5(8.
93%)2(3.
57%)3(5.
36%)2(3.
57%)1(1.
79%)1(1.
79%)6(12.
24%)4(8.
16%)3(6.
12%)4(8.
16%)2(4.
08%)2(4.
08%)1(2.
04%)5(15.
63%)4(12.
50%)3(9.
38%)3(9.
38%)1(3.
13%)2(6.
25%)0(0.
00%)-------Siteofinfection,no(%)0.
713LungUrinarytractAbdomenOther18(32.
14%)15(26.
79%)11(19.
64%)12(21.
43%)23(46.
94%)13(26.
53%)7(14.
29%)6(12.
24%)15(46.
88%)8(25.
00%)6(18.
75%)3(9.
38%)----Intervention,no(%)MechanicalventilationCRRTVasopressorusageStudyoutcome,no(%)28-daymortality3(5.
36%)2(3.
57%)0(0.
00%)2(3.
57%)4(8.
16%)6(12.
24%)4(8.
16%)4(8.
16%)12(37.
50%)15(46.
88%)13(40.
63%)14(43.
75%)0.
005**0.
004**0.
001**0.
001**Abbreviations:COPDchronicobstructivepulmonarydisorder,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitonin,BUNbloodureanitrogen,Scrserumcreatinine,ALTalaninetransaminase,ASTaspartatetransaminase,CRRTcontinuousrenalreplacementtherapyDataareexpressedasno.
(%),ormean(standarddeviation,SD)asappropriateSignificantdifferencesaremarkedby*(P<0.
05)or**(P<0.
01)Liuetal.
BMCAnesthesiology(2016)16:46Page3of9ofAPACHEIIscore,SequentialOrganFailureAssess-ment(SOFA)score,suPAR,procalcitonin(PCT)andlacticacidcomparedwithpatientswithsepsis.
Inaddition,therewere19patients(13.
87%)receivingmechanicalventilationtreatment,23patients(16.
79%)receivingcontinuousrenalreplacementtherapy,and17patients(12.
41%)receivingvasopressorsupport.
Thereweresignificantdifferencesintheproportionofpatientsreceivingmechanicalventilation,continuousrenalre-placementtherapyorvasopressorsupportamongthethreegroups(Table1).
KineticsofsuPARAmongtheenrolledpatients,atotalof117patientssur-vivedand20died.
AsshowninFig.
1a,patientswhodiedhadsignificantlyhighersuPARconcentrations(15.
82±2.
72ng/mL)onadmissionincomparisonwiththesurvivors(9.
04±3.
41ng/mL,P<0.
01).
Toinvesti-gatewhetherplasmasuPARconcentrationsremaincon-stantovertime,serialplasmadeterminationswerefurtherconductedonday3andday7afteradmission.
Ateachindicateddayofsampling,plasmasuPARcon-centrationsweremarkedlyhigheramongnon-survivorsthanamongsurvivors.
PlasmasuPARconcentrationsremainedstableseparatelywithinsurvivorsandwithinnon-survivorsduringthefirstweekofthediseasecourse.
Inaddition,inthesepticshockgroup14patientsdiedand18survived.
Thesenon-survivorshadsignifi-cantlyhighersuPARconcentrations(17.
05±2.
96ng/mL)onadmissionwhencomparedwiththesurvivors(10.
48±1.
86ng/mL,P<0.
01)inthesepticshockgroup(Fig.
1b).
ValueofindicatorsinpredictingpooroutcomeROCanalysiswasconstructedtoexaminetheperform-anceofindicatorsaspredictorsofpooroutcome,andtheareaunderthecurve(AUC)foreachindicatorwascalculated,respectively.
TheAUC,optimalcutoffvalue,sensitivityandspecificityofeachindicatorarepresentedinTable2.
ROCcurvesindicatedthatsuPARhadastrongpowerforpredictingunfavorableoutcomeassug-gestedbyAUCof0.
788±0.
058,whichwaslessthanthatofAPACHEIIscore(0.
813±0.
055,P<0.
05)butgreaterthanthatofSOFAscore(0.
779±0.
075,P<0.
05)andPCT(0.
651±0.
081,P<0.
01)(Fig.
2).
CoordinatepointsofROCsindicatedthatanAPACHEIIscoreofatleast15asacutoffhadaspecificityofgreaterthan70%topredictdeathandsuPARofatleast10.
82ng/mLshowedaspecificityofgreaterthan70%topredictdeath.
Furthermore,ROCanalysisofthecombinationofAPACHEIIscoreandsuPARwasfurtherperformed.
WefoundthattheAUCsweregreaterforthecombin-ationofAPACHEIIscoreandsuPAR(0.
878±0.
042)thanforthesingleAPACHEIIscoreorsinglesuPAR(Fig.
3),demonstratingthatcombinationofAPACHEIIscoreandsuPARmaysupplythemorepowerfulprog-nosticutilityforthemortalityofsepsis.
UnivariateCoxregressionanalysisWeperformedunivariateCoxregressionanalysistoexaminetheassociationsofeachvariablewithunfavor-ableoutcomeandcalculatedthestandardizedregressioncoefficient(β)andtheHRforeachvariable.
AsshowninTable3,baselineAPACHEIIscorehadthegreatestab-solutevalueofstandardizedβvalue(0.
2457).
Theabso-lutevalueofstandardizedβvalueforsuPARwas0.
1482andtheunadjustedHRwas2.
18(95%confidenceinter-val[CI],1.
77-2.
95,P=0.
000),indicatingthatsuPARhadapowerforpredictingunfavorableoutcome.
MultivariateCoxregressionanalysisAmultivariateCoxregressionanalysiswasconductedusingaforwardstep-wisemannertodetermineanovelriskstratificationrule.
Alltheobservedbaselineparame-terslikeage,gender,lacticacid,bloodureanitrogen,serumcreatinine,APACHEIIscore,SOFAscore,suPARFig.
1PlasmasuPARconcentrationsamongsurvivorsandnon-survivorsduringthecourseof7days.
aPlasmasuPARconcentrationsamong117survivorsand20non-survivorsfromallthepatients.
bPlasmasuPARconcentrationsamong18survivorsand14non-survivorsfromthepatientswithsepticshock.
Valuesareexpressedasmean±SD.
**P<0.
01betweensurvivorsandnon-survivorsattheindicateddayofsampling.
suPAR,solubleurokinaseplasminogenactivatorreceptorLiuetal.
BMCAnesthesiology(2016)16:46Page4of9andPCTwereincludedinthepredictionmodelwhenad-ventofdeathwassetasthedependentvariable.
There-sultsareshowninTable4.
Accordingtothisanalysis,APACHEIIscoreofatleast15andplasmasuPARcon-centrationsofatleast10.
82ng/mLweretheindependentpredictorswhichenteredtheequation,demonstratingthattheseabovedefinedcutoffvaluesmaybesafelyusedtocreateastratificationruleforevaluatingunfavorableout-comeinsepsis.
TheprognosticsignificanceofsuPARwasfurtherconfirmedaftertheriskstratificationrulewasgener-ated(Table5).
Moreprecisely,ORfordeathwithsuPARofatleast10.
82ng/mLamongpatientswithanAPACHEIIscoreoflessthan15was4.
72;ORwas2.
04withsuPARofatleast10.
82ng/mLamongpatientswithanAPACHEIIscoreofatleast15.
ThecalculatedORsweresignificantlydifferent,demon-stratingthatAPACHEIIscoreandsuPARwereinde-pendentlyassociatedwiththeunfavorableoutcomeandcouldbothbeintegratedintoariskstratificationrule.
RiskstratificationruleofAPACHEIIscoreandsuPAROnthebasisoftheabovecutoffsofAPACHEIIscoreandsuPAR,riskstratificationrulewasdeterminedasfol-lows:(A)patientswithanAPACHEIIscoreoflessthan15andsuPARoflessthan10.
82ng/mL,(B)patientswithanAPACHEIIscoreoflessthan15andsuPARofatleast10.
82ng/mL,(C)patientswithanAPACHEIIscoreofatleast15andsuPARoflessthan10.
82ng/mL,and(D)patientswithanAPACHEIIscoreofatleast15andsuPARofatleast10.
82ng/mL.
Therewere72,27,18,and20patientsineachstratum,withrespectivemor-talitiesof1.
39%(n=1),11.
11%(n=3),27.
78%(n=5),and55.
0%(n=11).
AsshowinFig.
4,eachstratumdif-feredsignificantlyfromtheothers(P=0.
002bythelog-ranktestwithinthedefinedstrata).
Thispredictionscorecorrespondedtodifferentgradesofdiseaseseverity,Table2PerformanceofvariablesinpredictingunfavorableoutcomeVariablesAUCROCPvalueCutoffvalueSensitivity(%)Specificity(%)APACHEIIscoreSOFAscore0.
813±0.
0550.
779±0.
075<0.
001**<0.
001**≥15.
00≥8.
5089.
680.
774.
872.
1suPAR0.
788±0.
058<0.
001**≥10.
8284.
977.
6PCT0.
651±0.
0810.
078≥24.
9757.
569.
2Abbreviations:AUCROCareaunderthereceiveroperatingcharacteristiccurve,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitoninSignificantdifferencesaremarkedby**(P<0.
01)Fig.
2Receiveroperatingcharacteristic(ROC)curvesofsuPAR,PCT,APACHEIIscore,andSOFAscoreonday1.
suPARhadastrongpowerforpredictingunfavorableoutcomeassuggestedbyareaunderthecurve(AUC)of0.
788±0.
058,P=0.
001.
suPAR,solubleurokinaseplasminogenactivatorreceptor;PCT,procalcitonin;APACHEII,AcutePhysiologyandChronicHealthEvaluationII;SOFA,SequentialOrganFailureAssessmentLiuetal.
BMCAnesthesiology(2016)16:46Page5of9thereforepatientswithseveresepsis/septicshocktendedtohavescorelevels(C)and(D)whenpatientswithsepsistendedtohavescorelevels(A)and(B).
DiscussionUndoubtedly,APACHEIIscorehasbeenadvocatedasthegoldstandardforriskevaluationincriticallyillpa-tients[19].
Nevertheless,agrowingbodyofevidencehassuggestedthatthescoremaysupplyinaccurateinforma-tioninthecertainpatients,suchasdisproportionatelyhighscoresinpatientswhoarelossofconsciousness[20].
Thistranslatesintoareal-worldcontextinwhichtheefficacyofAPACHEIIscoretopredictdeathisnotaspowerfulasclinicianswouldconsider.
Toourknowledge,previousstudyconductedbyGiamarellos-Bourboulisetal.
hasproposedanewprog-nosticationruleforpredictingtheoutcomeofsepsisbyAPACHEIIscoreandsuPAR[5].
Ourstudywastofur-therreaffirmtheriskstratificationsystemforChinesepatientswithsepsisbycombiningAPACHEIIscoreandplasmasuPARconcentrations.
Thereweresomediffer-encesbetweenourstudyandGiamarellos-Bourboulis'sstudy.
First,theenrolledpatientsofthetwostudieswerefromdifferentethnicgroups.
WeenrolledAsianpopula-tions(Chineseorigin),whileGiamarellos-Bourboulisetal.
mainlyenrolledtheEuropeanpopulations.
Second,thecutoffsofAPACHEIIandsuPARwhichwereusedtodeterminethestrataofdiseaseseveritywerenotuni-formlythesame.
Specifically,ourstudyindicatedthatFig.
3Receiveroperatingcharacteristic(ROC)curvesofsuPAR,APACHEIIscore,andtheircombinationonday1.
ThecombinationofsuPARandAPACHEIIscorehadastrongpowerforpredictingunfavorableoutcomeassuggestedbyareaunderthecurve(AUC)of0.
878±0.
042,P=0.
000.
suPAR,solubleurokinaseplasminogenactivatorreceptor;APACHEII,AcutePhysiologyandChronicHealthEvaluationIITable3PredictorsofunfavorableoutcomebyunivariateCoxregressionanalysisVariablesStandardβHazardratio95%CIPvalueAgeGenderLacticacidBUNScr0.
06830.
08150.
03680.
02400.
02171.
071.
341.
021.
011.
000.
84–1.
500.
91–1.
830.
82–1.
150.
57–1.
120.
53–1.
040.
6340.
7590.
3320.
4580.
465APACHEIIscoreSOFAscore0.
24570.
12433.
011.
682.
26–4.
691.
14–2.
39<0.
001**<0.
001**SuPARPCT0.
14820.
08912.
181.
671.
77–2.
951.
42–2.
08<0.
001**0.
024*Abbreviations:BUNbloodureanitrogen,Scrserumcreatinine,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitonin,CIconfidenceintervalThehazardratioindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby*(P<0.
05)or**(P<0.
01)Table4IndependentpredictorsofunfavorableoutcomebymultivariateCoxregressionanalysisVariablesStandardβHazardratio95%CIPvalueAPACHEIIscore0.
27433.
572.
38–4.
40<0.
001**SuPAR0.
15302.
261.
94–2.
87<0.
001**Abbreviations:APACHEIIAcutePhysiologyandChronicHealthEvaluationII,suPARsolubleurokinaseplasminogenactivatorreceptor,CIconfidenceintervalThehazardratioindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby**(P<0.
01)Liuetal.
BMCAnesthesiology(2016)16:46Page6of9APACHEII≥15andsuPAR≥10.
82ng/mLwereinde-pendentlyassociatedwithunfavorableoutcomewhileGiamarellos-Bourboulis'sstudyshowedthatAPACHEII≥17andsuPAR≥12ng/mlweretheoptimalcutoffs.
Third,weconstructedROCanalysisandcalculatedtheAUCtocomparetheperformanceofsuPAR,PCT,APA-CHEIIscore,andSOFAscoreaspredictorsofpoorout-come.
WefoundthatsuPARhadastrongpowerforpredictingunfavorableoutcomeassuggestedbyAUCof0.
788±0.
058,whichwaslessthanthatofAPACHEIIscore(0.
813±0.
055)butgreaterthanthatofSOFAscore(0.
779±0.
075)andPCT(0.
651±0.
081).
However,Giamarellos-Bourboulisetal.
justconductedROCana-lysiswithsuPARandAPACHEIIscoreasindependentvariablestopredictunfavorableoutcome.
Takento-gether,givenenrolledpatientswerefromdifferentethnicgroups,ourstudymayfurtherconfirmthepreliminaryconclusionthatapredictionrulewithfourlevelsofriskinsepsisbasedonAPACHEIIscoreandsuPARwasproposed.
Similartothefindingsofapreviousclinicaltrialcon-cerningplasmasuPARmeasurement[15],ourstudyclearlyshowedthatsuPARconcentrationswererelativelystableinthesystemiccirculationinbothsurvivorsandnon-survivorsduringthefirstweekofthediseasecourse.
Therefore,weinferthatthevalidityofthedevelopedprognosticationscoreremainsconstantevenifsuPARisnotmeasuredduringtheveryfirstdaysafterICUadmissionduetothestabilityofsuPARconcentra-tionsoverthediseasecourse.
Thesefindingswerecom-parabletootherdiseasesincludingchronicobstructivepulmonarydisease(COPD)[21]oracuterespiratorydis-tresssyndrome(ARDS)[22],inwhichsuPARwasregardedasanindependentpredictorforunfavorableoutcomes.
Severesepsishasareportedannualincidenceinadultsofupto300casesper100,000population[23,24].
Af-fectedpatientshavehighmortalities,complications,andresourceutilization.
Althoughfigureshaveimprovedintherecentyears[2,3],theriskfordeathremainshigh[25].
Consequently,improvingoutcomemaybeadaunt-ingwork.
Oneofpivotalmeasuresistoidentifythesep-ticpatientswithpoorprognosisrapidly[4].
OurstudysuggestedonecompositerulefordeterminingpatientswithsepsisathighriskonthebasisofAPACHEIIscoreandplasmasuPARconcentrations.
Actually,themeas-urementprocedureissosimplethatwecancompletethemeasurementforevery45patientsampleswithinabout4h.
Thepriceforthemeasurementisalsorela-tivelyreasonableandweonlyspend6,000CNY(about924USD)onevaluating45patientsamples,thatmeansweneedspendabout133CNY(20USD)onmeasuringTable5ValidationofthenovelstratificationruleAPACHEIIscoresuPARSurvivors,Number(%)Non-survivors,Number(%)PvalueOR(95%CI)<15<10.
8271(98.
61%)1(1.
39%)<0.
001**4.
72(3.
36–5.
81)≥10.
8224(88.
89%)3(11.
11%)≥15<10.
8213(72.
22%)5(27.
78%)<0.
001**2.
04(1.
85–3.
50)≥10.
829(45.
00%)11(55.
00%)Abbreviations:APACHEIIAcutePhysiologyandChronicHealthEvaluationII,suPARsolubleurokinaseplasminogenactivatorreceptor,ORoddsratio,CIconfidenceintervalTheORindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby**(P<0.
01)Fig.
4Kaplan-Meierestimatesofsurvivalofpatientsstratifiedintofourstrataofseverity.
Everystratumdifferedsignificantlyfromtheothers.
P=0.
002bythelog-ranktestwithinthefourdefinedstrata.
APACHEII,AcutePhysiologyandChronicHealthEvaluationII;suPAR,solubleurokinaseplasminogenactivatorreceptorLiuetal.
BMCAnesthesiology(2016)16:46Page7of9onepatientsample.
Undoubtedly,thesuPARmeasure-mentisrelativelycost-effective.
Therefore,giventhesimpleandinexpensivemeasurement,thecombinationofAPACHEIIscoreandplasmasuPARconcentrationsmaycontributetointensivecaremanagementinthesepticpatientsproperly.
Currently,evidencehassuggestedthatthevalueofsinglescoringsystemasastandardofclinicaldecision-makinginsepticpatientsisquestionable.
APACHEIIscoreislikelytorecognizeeitherlow-riskpatientsorvery-high-riskpatients,butnotthesepatientsbetweenthetwoextremes[20].
Theproposedriskstratificationrulefulfillsthisneedbecauseitdiscriminatesnotonlypatientslyingatoneofthetwoextremes-strata(A)and(D)-butalsopatientswithmoderatediseasesever-ity,namelypatientswithanAPACHEIIscoreoflessthan15andsuPARofatleast10.
82ng/mLorpatientswithanAPACHEIIscoreofatleast15andsuPARoflessthan10.
82ng/mL,whobelongtostrata(B)and(C),respectively.
ConclusionsInsummary,combinationofAPACHEIIscoreandsuPARmaysupplythepowerfulprognosticutilityforthemortalityofsepsis.
Ourfindingssuggestthatincorp-oratingsuPARintoAPACHEIIscoreasacompositeriskstratificationruleforsepsisisworthconsidering.
AbbreviationsAPACHEII,AcutePhysiologyandChronicHealthEvaluationII;ARDS,acuterespiratorydistresssyndrome;AUC,areaunderthecurve;CI,confidenceinterval;COPD,chronicobstructivepulmonarydisease;ICU,intensivecareunit;IQR,interquartileranges;OR,oddsratio;PCT,procalcitonin;ROC,receiveroperatingcharacteristic;SD,standarddeviation;SOFA,sequentialorganfailureassessment;suPAR,solubleurokinaseplasminogenactivatorreceptor;uPA,urokinaseplasminogenactivator;uPAR,urokinaseplasminogenactivatorreceptorAcknowledgementsNone.
FundingThisworkwasfinanciallysupportedbythegrantfromthe2013-2014Na-tionalClinicalKeySpecialtyConstructionProject.
AvailabilityofdataandmaterialsAlldatasetsarepresentedinthemainpaperoradditionalsupportingfiles.
Authors'contributionsXLandSPhavemadesubstantialcontributionstoconceptionanddesign,oracquisitionofdata,oranalysisandinterpretationofdata;XL,YS,andZLhavebeeninvolvedindraftingthemanuscriptorrevisingitcriticallyforimportantintellectualcontent;AFandHWhavegivenfinalapprovaloftheversiontobepublished;QGandSPhaveagreedtobeaccountableforallaspectsoftheworkinensuringthatquestionsrelatedtotheaccuracyorintegrityofanypartoftheworkareappropriatelyinvestigatedandresolved.
Allauthorsreadandapprovedthefinalmanuscript.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
ConsentforpublicationNotapplicable.
EthicsapprovalandconsenttoparticipateThestudywasapprovedbyShanghaiJiaotongUniversityXinhuaHospitalEthicsCommitteeandwascarriedoutinaccordancewiththeDeclarationofHelsinki.
Informedconsentswereobtainedfromallpatients.
Received:12January2016Accepted:15July2016References1.
ARISEInvestigators;ANZICSClinicalTrialsGroup,PeakeSL,DelaneyA,BaileyM,BellomoR,CameronPA,CooperDJ,HigginsAM,HoldgateA,HoweBD,etal.
Goal-directedresuscitationforpatientswithearlysepticshock.
NEnglJMed.
2014;371:1496–506.
2.
KaukonenKM,BaileyM,SuzukiS,PilcherD,BellomoR.
MortalityrelatedtoseveresepsisandsepticshockamongcriticallyillpatientsinAustraliaandNewZealand,2000–2012.
JAMA.
2014;311:1308–16.
3.
ReinhartK,DanielsR,KissoonN,O'BrienJ,MachadoFR,JimenezE,GSAExecutiveBoardandWSDExecutiveBoard.
Theburdenofsepsis-acalltoactioninsupportofWorldSepsisDay2013.
JCritCare.
2013;28:526–8.
4.
DellingerRP,LevyMM,RhodesA,AnnaneD,GerlachH,OpalSM,SevranskyJE,SprungCL,DouglasIS,JaeschkeR,etal.
SurvivingSepsisCampaign:internationalguidelinesformanagementofseveresepsisandsepticshock,2012.
IntensiveCareMed.
2013;39:165–228.
5.
Giamarellos-BourboulisEJ,Norrby-TeglundA,MylonaV,SavvaA,TsangarisI,DimopoulouI,MouktaroudiM,RaftogiannisM,GeorgitsiM,LinnérA,etal.
Riskassessmentinsepsis:anewprognosticationrulebyAPACHEIIscoreandserumsolubleurokinaseplasminogenactivatorreceptor.
CritCare.
2012;16:R149.
6.
VeraS,MartínezR,GormazJG,GajardoA,GalleguillosF,RodrigoR.
Novelrelationshipsbetweenoxidativestressandangiogenesis-relatedfactorsinsepsis:Newbiomarkersandtherapies.
AnnMed.
2015;47:289–300.
7.
HongDY,KimJW,PaikJH,JungHM,BaekKJ,ParkSO,LeeKR.
Valueofplasmaneutrophilgelatinase-associatedlipocalininpredictingthemortalityofpatientswithsepsisattheemergencydepartment.
ClinChimActa.
2015;452:177–81.
8.
LinderA,ArnoldR,BoydJH,ZindovicM,ZindovicI,LangeA,PaulssonM,NybergP,RussellJA,PritchardD,etal.
Heparin-BindingProteinMeasurementImprovesthePredictionofSevereInfectionWithOrganDysfunctionintheEmergencyDepartment.
CritCareMed.
2015;43:2378–86.
9.
HurM,KimH,KimHJ,YangHS,MagriniL,MarinoR,CardelliP,DiSommaS,GREATNetwork.
SolubleST2hasaprognosticroleinpatientswithsuspectedsepsis.
AnnLabMed.
2015;35:570–7.
10.
BackesY,vanderSluijsKF,MackieDP,TackeF,KochA,TenhunenJJ,SchultzMJ.
UsefulnessofsuPARasabiologicalmarkerinpatientswithsystemicinflammationorinfection:asystematicreview.
IntensiveCareMed.
2012;38:1418–28.
11.
MadsenCD,SideniusN.
Theinteractionbetweenurokinasereceptorandvitronectinincelladhesionandsignaling.
EurJCellBiol.
2008;87:617–29.
12.
MekonnenG,CorbanMT,HungOY,EshtehardiP,EapenDJ,Al-KassemH,Rasoul-ArzrumlyE,GogasBD,McDanielMC,PielakT,etal.
Plasmasolubleurokinase-typeplasminogenactivatorreceptorlevelisindependentlyassociatedwithcoronarymicrovascularfunctioninpatientswithnon-obstructivecoronaryarterydisease.
Atherosclerosis.
2015;239:55–60.
13.
TzanakakiG,PaparoupaM,KyprianouM,BarbouniA,Eugen-OlsenJ,Kourea-KremastinouJ.
ElevatedsolubleurokinasereceptorvaluesinCSF,ageandbacterialmeningitisinfectionareindependentandadditiveriskfactorsoffataloutcome.
EurJClinMicrobiolInfectDis.
2012;31:1157–62.
14.
HuttunenR,SyrjnenJ,VuentoR,HurmeM,HuhtalaH,LaineJ,PessiT,AittoniemiJ.
Plasmalevelofsolubleurokinase-typeplasminogenactivatorreceptorasapredictorofdiseaseseverityandcasefatalityinpatientswithbacteraemia:aprospectivecohortstudy.
JInternMed.
2011;270:32–40.
15.
KochA,VoigtS,KruschinskiC,SansonE,DückersH,HornA,YagmurE,ZimmermannH,TrautweinC,TackeF.
Circulatingsolubleurokinaseplasminogenactivatorreceptorisstablyelevatedduringthefirstweekoftreatmentintheintensivecareunitandpredictsmortalityincriticallyillpatients.
CritCare.
2011;15:R63.
16.
HoeniglM,RaggamRB,WagnerJ,ValentinT,LeitnerE,SeeberK,Zollner-SchwetzI,KrammerW,PrüllerF,GrisoldAJ,etal.
Diagnosticaccuracyofsolubleurokinaseplasminogenactivatorreceptor(suPAR)forpredictionofbacteremiainpatientswithsystemicinflammatoryresponsesyndrome.
ClinBiochem.
2013;46:225–9.
Liuetal.
BMCAnesthesiology(2016)16:46Page8of917.
OkuluE,ArsanS,AkinIM,AtesC,AlanS,KilicA,AtasayB.
SerumLevelsofSolubleUrokinasePlasminogenActivatorReceptorinInfantswithLate-onsetSepsis.
JClinLabAnal.
2015;29:347–52.
18.
LevyMM,FinkMP,MarshallJC,AbrahamE,AngusD,CookD,CohenJ,OpalSM,VincentJL,RamsayG,SCCM/ESICM/ACCP/ATS/SIS.
2001SCCM/ESICM/ACCP/ATS/SISinternationalsepsisdefinitionsconference.
CritCareMed.
2003;31:1250–6.
19.
CorrêaTD,SanchesPR,deMoraisLC,ScarinFC,SilvaE,BarbasCS.
Performanceofnoninvasiveventilationinacuterespiratoryfailureincriticallyillpatients:aprospective,observational,cohortstudy.
BMCPulmMed.
2015;15:144.
20.
VincentJL,OpalSM,MarshallJC.
TenreasonswhyweshouldNOTuseseverityscoresasentrycriteriaforclinicaltrialsorinourtreatmentdecisions.
CritCareMed.
2010;38:283–7.
21.
Can,GüzelantA,YerlikayaFH,Yosunkaya.
Theroleofserumsolubleurokinase-typeplasminogenactivatorreceptorinstablechronicobstructivepulmonarydisease.
JInvestigMed.
2014;62:938–43.
22.
GeboersDG,deBeerFM,Tuip-deBoerAM,vanderPollT,HornJ,CremerOL,BontenMJ,OngDS,SchultzMJ,BosLD.
PlasmasuPARasaprognosticbiologicalmarkerforICUmortalityinARDSpatients.
IntensiveCareMed.
2015;41:1281–90.
23.
JawadI,LukiI,RafnssonSB.
Assessingavailableinformationontheburdenofsepsis:globalestimatesofincidence,prevalenceandmortality.
JGlobHealth.
2012;2:010404.
24.
GaieskiDF,EdwardsJM,KallanMJ,CarrBG.
BenchmarkingtheincidenceandmortalityofseveresepsisintheUnitedStates.
CritCareMed.
2013;41:1167–74.
25.
HarrisonDA,WelchCA,EddlestonJM.
TheepidemiologyofseveresepsisinEngland,WalesandNorthernIreland,1996to2004:secondaryanalysisofahighqualityclinicaldatabase,theICNARCCaseMixProgrammeDatabase.
CritCare.
2006;10:R42.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Liuetal.
BMCAnesthesiology(2016)16:46Page9of9
PreviousstudyhasproposedtodevelopapowerfulriskassessmentrulebythecombinationofAcutePhysiologyandChronicHealthEvaluationII(APACHEII)scoreandplasmasolubleurokinaseplasminogenactivatorreceptor(suPAR).
ThatreaffirmationofsuPARasaprognosticmarkerinChinesepatientswithseveresepsisistheaimofthestudy.
Methods:Atotalof137consecutiveChinesepatientswithsepsiswereenrolledinaprospectivestudycohort.
Demographicandclinicalcharacteristics,conventionalriskfactorsandimportantlaboratorydatawereprospectivelyrecorded.
SequentialplasmasuPARconcentrationsweremeasuredbyanenzymeimmunoabsorbentassayondays1,3,and7afteradmissiontotheintensivecareunit(ICU).
Receiveroperatingcharacteristic(ROC)curvesandCoxregressionanalysiswereusedtoexaminetheperformanceofsuPARindevelopingaruleforriskstratification.
Results:TheresultsshowedthatplasmasuPARconcentrationsremainedrelativelystablewithinsurvivorsandnon-survivorsduringthefirstweekofdiseasecourse.
RegressionanalysisindicatedthatAPACHEII≥15andsuPAR≥10.
82ng/mLwereindependentlyassociatedwithunfavorableoutcome.
WiththeabovecutoffsofAPACHEIIandsuPAR,strataofdiseaseseverityweredetermined.
Themortalityofeachstratumdifferedsignificantlyfromtheothers.
Conclusions:CombinationofAPACHEIIscoreandsuPARmaysupplythepowerfulprognosticutilityforthemortalityofsepsis.
Keywords:Sepsis,Riskstratification,Solubleurokinaseplasminogenactivatorreceptor(suPAR),AcutePhysiologyandChronicHealthEvaluationII(APACHEII)BackgroundTheincidenceofsepsisinadultshasbeenincreasing,withseveresepsisandsepticshockremainingamongthemajorcausesofdeathworldwide[1].
Despitethemortalityisonadecliningtrendinrecentyears[2],lowawareness,laterecognition,andimpropertreatmentarestillcommon[3].
Oneofthefundamentalprinciplesfortheappropriatemanagementofsepsisistimelydiscriminationofthepa-tientsathighriskfordeath[4].
Thisisgenerallydependentontheapplicationofscoresystemsandplasmabiomarkers.
Althoughthewell-recognizedscoreistheAcutePhysiologyandChronicHealthEvaluationII(APACHEII),APACHEIIscorehassomepotentialpitfallsthatmayleadtoinaccurateevaluation.
Takeyoungpatientswithseveresepsisbutwithoutchronicorgandysfunctionforinstance,theAPACHEIIscoremayberelativelylowdespitetheriskforanunfavorableoutcomeishigh[5].
Althoughvariousbiologicalmarkersarewidelyex-plored[6–9],onlyafewhavebeenappliedintheclinicalpractice.
Thesolubleurokinaseplasminogenactivatorreceptor(suPAR),whichexistsinthreeforms(I-III,II-IIIandI),isregardedasanovelbiomarkerofimmunesystemactivation[10].
Urokinaseplasminogenactivator*Correspondence:drshumingpan@hotmail.
comDepartmentofEmergency,XinhuaHospital,ShanghaiJiaotongUniversitySchoolofMedicine,1665KongjiangRoad,Shanghai200092,China2016Liuetal.
OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Liuetal.
BMCAnesthesiology(2016)16:46DOI10.
1186/s12871-016-0212-3receptor(uPAR)isembeddedinthecellmembranesofvariousimmunologicallyactivecellsand,withitsligand,urokinaseplasminogenactivator(uPA),takespartinarangeofimmunologicactivities[11].
Uponinflammatorystimulation,uPARiscleavedfromthecellsurfacebyproteasesintothesolubleformofthereceptor-suPAR-whichcanbeassessedinblood,urine,bronchoalveolarlavage,andcerebrospinalfluid[12,13].
RecentstudieshaverevealedthatsuPARmayhavetheabilitytopredictthemortalityofsepsis[14–17].
ItisnoteworthythatGiamarellos-Bourboulisetal.
haveproposedanewprog-nosticationruleforpredictingtheoutcomeofsepsisbyAPACHEIIscoreandsuPAR[5].
Theprimarypurposeofthepresentstudywastofur-therreaffirmthepredictionruleforthemortalityinChinesepatientswithsepsisbycombiningAPACHEIIscoreandplasmasuPARconcentrations.
MethodsStudydesignThisprospectivetrialinvolvedconsecutiveChinesepa-tientswithsepsispresentingtotheintensivecareunit(ICU)oftheDepartmentofEmergency,XinhuaHos-pital,ShanghaiJiaotongUniversitySchoolofMedicine,fromMarch2013toFebruary2015.
Foreachpatientwithsuspectedinfection,acompletediagnosticwork-upwasperformed.
Thework-upcom-priseddemographicandclinicalcharacteristics,conven-tionalriskfactors,andimportantlaboratorydataincludingbloodroutineexamination,microbiologicalculturing,chestx-ray,andchestorabdominalcomputedtomographyifnecessary.
Broadspectrumantimicrobialtreatmentwasusedwithin1hfromtherecognitionofthesepticstatus.
Patientswereeligibleiftheymettheinclusioncriteria:(1)ageofatleast18years;(2)sepsisduetooneofthefollowinginfections:communityacquiredpneumonia,hospitalacquiredpneumonia,ventilator-associatedpneumonia,acutepyelonephritis,intra-abdominalinfec-tion,orprimarybacteremia;and(3)bloodsamplingwithin24hfromthepresentationofsignsofsepsis.
Pa-tientsaffectedbyadvancedcancerorterminalpatientswithotherpathologieswereexcluded.
Alleligiblepatientswerefurtherclassifiedaccordingtostandarddefinitionsofsepsis,severesepsis,andsepticshock[18].
Morespecifically,sepsiswasdefinedasthepresenceofsuspectedorconfirmedinfectiontogetherwithtwoormorecriteriaforasystemicinflammatoryresponse;severesepsiswasdefinedassepsiswithsepsis-inducedorgandysfunction,hypotensionorhypoperfusion;septicshockwasde-finedasrefractoryhypotensionorhypoperfusiondes-pitesufficientfluidresuscitation.
BloodmeasurementsVenousblood(3mL)wascollectedfrompatientspre-sentingtotheICU(day1)andrepeatedonthefollowingday3andday7afteradmission.
WholebloodwasdrawnintoacentrifugetubecontainingEDTAanti-coagulant.
Aftercentrifugationat3,000gfor10minat4°C,plasmasampleswerekeptfrozenat80°Cuntilassayed.
suPARwasdeterminedinduplicatebyacom-mercialdoublemonoclonalantibodysandwichenzymeimmunoassay(suPARnosticStandardkit;ViroGatesA/S,Birkerd,Denmark)inaccordancewiththeinstructionsofthemanufacturer.
Every45bloodsam-plescanbemeasuredwithinabout4h.
Thelinearityofthisassayiscomprisedbetween2.
0and15.
6ng/mL,andthetotalimprecision,expressedascoefficientofvari-ation(CV%),rangesfrom2.
3to6.
0%.
StudyoutcomesPatientswhosurvivedwerefurtherfollowedupbytele-phonecalls.
Theunfavorableoutcomeofthestudywasdefinedasdeathfromanycausewithin28daysafterad-missiontotheICU.
StatisticalanalysisContinuousvariableswerepresentedasmeanvalues±standarddeviation(SD)ormedianwithinterquartileranges(IQR),whilecategoricalvariableswereexpressedasper-centages.
Thestatisticalsignificanceofintergroupdiffer-enceswascomparedthroughunpairedStudent'st-testorMann–WhitneyUtestforcontinuousvariablesandthroughPearson'sχ2testforcategoricalvariables.
Thefollowingstepswereperformedtoestablishariskstratificationrule:First,receiveroperatingcharacteristic(ROC)analysiswasconductedwithbaselinelevelsofAPACHEIIscoreandsuPARtodeterminethepredic-tionsensitivityandspecificityofthevariables.
Second,weusedunivariateandmultivariateCoxregressionana-lysestocalculatehazardratios(HR)with95%confi-denceintervals(CIs).
Third,strataofdiseaseseveritywereestablishedusingthecutoffsofAPACHEIIscoreandsuPAR.
Oddsratios(OR)and95%CIsforriskpre-dictionwithineachstratumwereassessedusingMantelandHaenszelstatistics.
Fourth,mortalitiesbetweenstratawereestimatedusingthelog-ranktest.
Atwo-sidedPvalue<0.
05wasconsideredstatisti-callysignificant.
AllanalyseswereperformedbytheIBMSPSSStatisticssoftwareversion19.
0(SPSS,Chi-cago,IL,USA).
ResultsBaselinecharacteristicsofthestudypopulationAtotalof137consecutivepatients(51.
09%men;meanage,69.
53±9.
28years)wereeligibleforenrollmentinthestudy.
AftertheinitialevaluationperformedintheLiuetal.
BMCAnesthesiology(2016)16:46Page2of9ICU,patientsweredividedintothreegroupsaccord-ingthediseaseseverity:group1,patientswithsepsis(n=56);group2,thosewithseveresepsis(n=49);andgroup3,thosewithsepticshock(n=32).
ThebaselineclinicalandlaboratorycharacteristicsofthepatientsareelaboratedinTable1.
Themostcommonlocationsofinfectionwerelungandurinarytract,andthedistributionoflocationswassimilaramongthethreegroups.
ThecommonestisolatedpathogensfromthestudycohortwereGram-negativemicroor-ganismswithapredominanceofEscherichiacoli,andbloodcultureswerepositivein43.
80%ofallpatients.
Therewasnotanydifferenceinpathogenstrainsamongthedifferentgroups(Table1).
Therewerenosignificantlystatisticaldifferencesinpa-tientswithsepsiscomparedtothoseinseveresepsisorsepticshockforgenderorage.
Patientswithseveresep-sisorsepticshocktendedtohavehigherbaselinelevelsTable1BaselineclinicalandlaboratorycharacteristicsofthestudysubjectsPatientgroupCharacteristicsSepsisSeveresepsisSepticshockPvalueDemographicsandunderlyingconditionsNumberofpatients564932-Males,no.
(%)29(51.
79%)27(55.
10%)14(43.
75%)0.
418Age(years),mean±SDCOPD,no(%)Hypertension,no(%)Diabetesmellitus,no(%)68.
04±9.
3620(35.
71%)23(41.
07%)9(16.
07%)71.
39±8.
8524(48.
98%)23(46.
94%)9(18.
37%)69.
16±9.
7319(59.
38%)17(53.
13%)7(21.
88%)0.
2460.
032*0.
4730.
381Baselineparameters,mean±SDAPACHEIIscoreSOFAscore9.
87±3.
125.
26±2.
0912.
50±4.
757.
83±2.
5318.
34±6.
0911.
42±3.
740.
001**0.
002**SuPAR(ng/mL)PCT(ng/mL)Whitebloodcellcount(109/L)6.
58±3.
176.
14±3.
5411.
96±2.
8668.
62±4.
8011.
05±4.
6018.
26±3.
9815.
97±5.
4427.
69±7.
2826.
67±7.
040.
001**<0.
001**0.
037*Lacticacid(mmol/L)1.
75±1.
163.
27±1.
486.
03±3.
820.
012*BUN(mmol/L)Scr(μmol/L)ALT(U/L)AST(U/L)Bilirubin(mg/dL)Platelet(109/L)Plasmaglucose(mmol/L)Hemoglobin(g/L)6.
42±3.
8570.
32±19.
5631.
23±10.
2732.
95±11.
0214.
60±8.
03154.
19±71.
527.
25±4.
89109.
84±33.
149.
05±4.
13103.
59±31.
0745.
62±16.
4460.
38±21.
3716.
23±9.
15134.
08±75.
178.
35±5.
18117.
08±20.
4911.
91±9.
39154.
08±40.
87153.
89±48.
01196.
35±65.
2920.
01±9.
66127.
60±65.
9510.
02±7.
11118.
05±20.
650.
017*0.
021*0.
013*0.
009**0.
6940.
7410.
3890.
436Pathogenstrains,no(%)0.
058EscherichiacoliKlebsiellapneumoniaPseudomonasaeruginosaAcinetobacterbaumanniiOtherGram-negativebacteriaStaphylococcusaureusEnterococcusspp6(10.
71%)5(8.
93%)2(3.
57%)3(5.
36%)2(3.
57%)1(1.
79%)1(1.
79%)6(12.
24%)4(8.
16%)3(6.
12%)4(8.
16%)2(4.
08%)2(4.
08%)1(2.
04%)5(15.
63%)4(12.
50%)3(9.
38%)3(9.
38%)1(3.
13%)2(6.
25%)0(0.
00%)-------Siteofinfection,no(%)0.
713LungUrinarytractAbdomenOther18(32.
14%)15(26.
79%)11(19.
64%)12(21.
43%)23(46.
94%)13(26.
53%)7(14.
29%)6(12.
24%)15(46.
88%)8(25.
00%)6(18.
75%)3(9.
38%)----Intervention,no(%)MechanicalventilationCRRTVasopressorusageStudyoutcome,no(%)28-daymortality3(5.
36%)2(3.
57%)0(0.
00%)2(3.
57%)4(8.
16%)6(12.
24%)4(8.
16%)4(8.
16%)12(37.
50%)15(46.
88%)13(40.
63%)14(43.
75%)0.
005**0.
004**0.
001**0.
001**Abbreviations:COPDchronicobstructivepulmonarydisorder,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitonin,BUNbloodureanitrogen,Scrserumcreatinine,ALTalaninetransaminase,ASTaspartatetransaminase,CRRTcontinuousrenalreplacementtherapyDataareexpressedasno.
(%),ormean(standarddeviation,SD)asappropriateSignificantdifferencesaremarkedby*(P<0.
05)or**(P<0.
01)Liuetal.
BMCAnesthesiology(2016)16:46Page3of9ofAPACHEIIscore,SequentialOrganFailureAssess-ment(SOFA)score,suPAR,procalcitonin(PCT)andlacticacidcomparedwithpatientswithsepsis.
Inaddition,therewere19patients(13.
87%)receivingmechanicalventilationtreatment,23patients(16.
79%)receivingcontinuousrenalreplacementtherapy,and17patients(12.
41%)receivingvasopressorsupport.
Thereweresignificantdifferencesintheproportionofpatientsreceivingmechanicalventilation,continuousrenalre-placementtherapyorvasopressorsupportamongthethreegroups(Table1).
KineticsofsuPARAmongtheenrolledpatients,atotalof117patientssur-vivedand20died.
AsshowninFig.
1a,patientswhodiedhadsignificantlyhighersuPARconcentrations(15.
82±2.
72ng/mL)onadmissionincomparisonwiththesurvivors(9.
04±3.
41ng/mL,P<0.
01).
Toinvesti-gatewhetherplasmasuPARconcentrationsremaincon-stantovertime,serialplasmadeterminationswerefurtherconductedonday3andday7afteradmission.
Ateachindicateddayofsampling,plasmasuPARcon-centrationsweremarkedlyhigheramongnon-survivorsthanamongsurvivors.
PlasmasuPARconcentrationsremainedstableseparatelywithinsurvivorsandwithinnon-survivorsduringthefirstweekofthediseasecourse.
Inaddition,inthesepticshockgroup14patientsdiedand18survived.
Thesenon-survivorshadsignifi-cantlyhighersuPARconcentrations(17.
05±2.
96ng/mL)onadmissionwhencomparedwiththesurvivors(10.
48±1.
86ng/mL,P<0.
01)inthesepticshockgroup(Fig.
1b).
ValueofindicatorsinpredictingpooroutcomeROCanalysiswasconstructedtoexaminetheperform-anceofindicatorsaspredictorsofpooroutcome,andtheareaunderthecurve(AUC)foreachindicatorwascalculated,respectively.
TheAUC,optimalcutoffvalue,sensitivityandspecificityofeachindicatorarepresentedinTable2.
ROCcurvesindicatedthatsuPARhadastrongpowerforpredictingunfavorableoutcomeassug-gestedbyAUCof0.
788±0.
058,whichwaslessthanthatofAPACHEIIscore(0.
813±0.
055,P<0.
05)butgreaterthanthatofSOFAscore(0.
779±0.
075,P<0.
05)andPCT(0.
651±0.
081,P<0.
01)(Fig.
2).
CoordinatepointsofROCsindicatedthatanAPACHEIIscoreofatleast15asacutoffhadaspecificityofgreaterthan70%topredictdeathandsuPARofatleast10.
82ng/mLshowedaspecificityofgreaterthan70%topredictdeath.
Furthermore,ROCanalysisofthecombinationofAPACHEIIscoreandsuPARwasfurtherperformed.
WefoundthattheAUCsweregreaterforthecombin-ationofAPACHEIIscoreandsuPAR(0.
878±0.
042)thanforthesingleAPACHEIIscoreorsinglesuPAR(Fig.
3),demonstratingthatcombinationofAPACHEIIscoreandsuPARmaysupplythemorepowerfulprog-nosticutilityforthemortalityofsepsis.
UnivariateCoxregressionanalysisWeperformedunivariateCoxregressionanalysistoexaminetheassociationsofeachvariablewithunfavor-ableoutcomeandcalculatedthestandardizedregressioncoefficient(β)andtheHRforeachvariable.
AsshowninTable3,baselineAPACHEIIscorehadthegreatestab-solutevalueofstandardizedβvalue(0.
2457).
Theabso-lutevalueofstandardizedβvalueforsuPARwas0.
1482andtheunadjustedHRwas2.
18(95%confidenceinter-val[CI],1.
77-2.
95,P=0.
000),indicatingthatsuPARhadapowerforpredictingunfavorableoutcome.
MultivariateCoxregressionanalysisAmultivariateCoxregressionanalysiswasconductedusingaforwardstep-wisemannertodetermineanovelriskstratificationrule.
Alltheobservedbaselineparame-terslikeage,gender,lacticacid,bloodureanitrogen,serumcreatinine,APACHEIIscore,SOFAscore,suPARFig.
1PlasmasuPARconcentrationsamongsurvivorsandnon-survivorsduringthecourseof7days.
aPlasmasuPARconcentrationsamong117survivorsand20non-survivorsfromallthepatients.
bPlasmasuPARconcentrationsamong18survivorsand14non-survivorsfromthepatientswithsepticshock.
Valuesareexpressedasmean±SD.
**P<0.
01betweensurvivorsandnon-survivorsattheindicateddayofsampling.
suPAR,solubleurokinaseplasminogenactivatorreceptorLiuetal.
BMCAnesthesiology(2016)16:46Page4of9andPCTwereincludedinthepredictionmodelwhenad-ventofdeathwassetasthedependentvariable.
There-sultsareshowninTable4.
Accordingtothisanalysis,APACHEIIscoreofatleast15andplasmasuPARcon-centrationsofatleast10.
82ng/mLweretheindependentpredictorswhichenteredtheequation,demonstratingthattheseabovedefinedcutoffvaluesmaybesafelyusedtocreateastratificationruleforevaluatingunfavorableout-comeinsepsis.
TheprognosticsignificanceofsuPARwasfurtherconfirmedaftertheriskstratificationrulewasgener-ated(Table5).
Moreprecisely,ORfordeathwithsuPARofatleast10.
82ng/mLamongpatientswithanAPACHEIIscoreoflessthan15was4.
72;ORwas2.
04withsuPARofatleast10.
82ng/mLamongpatientswithanAPACHEIIscoreofatleast15.
ThecalculatedORsweresignificantlydifferent,demon-stratingthatAPACHEIIscoreandsuPARwereinde-pendentlyassociatedwiththeunfavorableoutcomeandcouldbothbeintegratedintoariskstratificationrule.
RiskstratificationruleofAPACHEIIscoreandsuPAROnthebasisoftheabovecutoffsofAPACHEIIscoreandsuPAR,riskstratificationrulewasdeterminedasfol-lows:(A)patientswithanAPACHEIIscoreoflessthan15andsuPARoflessthan10.
82ng/mL,(B)patientswithanAPACHEIIscoreoflessthan15andsuPARofatleast10.
82ng/mL,(C)patientswithanAPACHEIIscoreofatleast15andsuPARoflessthan10.
82ng/mL,and(D)patientswithanAPACHEIIscoreofatleast15andsuPARofatleast10.
82ng/mL.
Therewere72,27,18,and20patientsineachstratum,withrespectivemor-talitiesof1.
39%(n=1),11.
11%(n=3),27.
78%(n=5),and55.
0%(n=11).
AsshowinFig.
4,eachstratumdif-feredsignificantlyfromtheothers(P=0.
002bythelog-ranktestwithinthedefinedstrata).
Thispredictionscorecorrespondedtodifferentgradesofdiseaseseverity,Table2PerformanceofvariablesinpredictingunfavorableoutcomeVariablesAUCROCPvalueCutoffvalueSensitivity(%)Specificity(%)APACHEIIscoreSOFAscore0.
813±0.
0550.
779±0.
075<0.
001**<0.
001**≥15.
00≥8.
5089.
680.
774.
872.
1suPAR0.
788±0.
058<0.
001**≥10.
8284.
977.
6PCT0.
651±0.
0810.
078≥24.
9757.
569.
2Abbreviations:AUCROCareaunderthereceiveroperatingcharacteristiccurve,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitoninSignificantdifferencesaremarkedby**(P<0.
01)Fig.
2Receiveroperatingcharacteristic(ROC)curvesofsuPAR,PCT,APACHEIIscore,andSOFAscoreonday1.
suPARhadastrongpowerforpredictingunfavorableoutcomeassuggestedbyareaunderthecurve(AUC)of0.
788±0.
058,P=0.
001.
suPAR,solubleurokinaseplasminogenactivatorreceptor;PCT,procalcitonin;APACHEII,AcutePhysiologyandChronicHealthEvaluationII;SOFA,SequentialOrganFailureAssessmentLiuetal.
BMCAnesthesiology(2016)16:46Page5of9thereforepatientswithseveresepsis/septicshocktendedtohavescorelevels(C)and(D)whenpatientswithsepsistendedtohavescorelevels(A)and(B).
DiscussionUndoubtedly,APACHEIIscorehasbeenadvocatedasthegoldstandardforriskevaluationincriticallyillpa-tients[19].
Nevertheless,agrowingbodyofevidencehassuggestedthatthescoremaysupplyinaccurateinforma-tioninthecertainpatients,suchasdisproportionatelyhighscoresinpatientswhoarelossofconsciousness[20].
Thistranslatesintoareal-worldcontextinwhichtheefficacyofAPACHEIIscoretopredictdeathisnotaspowerfulasclinicianswouldconsider.
Toourknowledge,previousstudyconductedbyGiamarellos-Bourboulisetal.
hasproposedanewprog-nosticationruleforpredictingtheoutcomeofsepsisbyAPACHEIIscoreandsuPAR[5].
Ourstudywastofur-therreaffirmtheriskstratificationsystemforChinesepatientswithsepsisbycombiningAPACHEIIscoreandplasmasuPARconcentrations.
Thereweresomediffer-encesbetweenourstudyandGiamarellos-Bourboulis'sstudy.
First,theenrolledpatientsofthetwostudieswerefromdifferentethnicgroups.
WeenrolledAsianpopula-tions(Chineseorigin),whileGiamarellos-Bourboulisetal.
mainlyenrolledtheEuropeanpopulations.
Second,thecutoffsofAPACHEIIandsuPARwhichwereusedtodeterminethestrataofdiseaseseveritywerenotuni-formlythesame.
Specifically,ourstudyindicatedthatFig.
3Receiveroperatingcharacteristic(ROC)curvesofsuPAR,APACHEIIscore,andtheircombinationonday1.
ThecombinationofsuPARandAPACHEIIscorehadastrongpowerforpredictingunfavorableoutcomeassuggestedbyareaunderthecurve(AUC)of0.
878±0.
042,P=0.
000.
suPAR,solubleurokinaseplasminogenactivatorreceptor;APACHEII,AcutePhysiologyandChronicHealthEvaluationIITable3PredictorsofunfavorableoutcomebyunivariateCoxregressionanalysisVariablesStandardβHazardratio95%CIPvalueAgeGenderLacticacidBUNScr0.
06830.
08150.
03680.
02400.
02171.
071.
341.
021.
011.
000.
84–1.
500.
91–1.
830.
82–1.
150.
57–1.
120.
53–1.
040.
6340.
7590.
3320.
4580.
465APACHEIIscoreSOFAscore0.
24570.
12433.
011.
682.
26–4.
691.
14–2.
39<0.
001**<0.
001**SuPARPCT0.
14820.
08912.
181.
671.
77–2.
951.
42–2.
08<0.
001**0.
024*Abbreviations:BUNbloodureanitrogen,Scrserumcreatinine,APACHEIIAcutePhysiologyandChronicHealthEvaluationII,SOFAsequentialorganfailureassessment,suPARsolubleurokinaseplasminogenactivatorreceptor,PCTprocalcitonin,CIconfidenceintervalThehazardratioindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby*(P<0.
05)or**(P<0.
01)Table4IndependentpredictorsofunfavorableoutcomebymultivariateCoxregressionanalysisVariablesStandardβHazardratio95%CIPvalueAPACHEIIscore0.
27433.
572.
38–4.
40<0.
001**SuPAR0.
15302.
261.
94–2.
87<0.
001**Abbreviations:APACHEIIAcutePhysiologyandChronicHealthEvaluationII,suPARsolubleurokinaseplasminogenactivatorreceptor,CIconfidenceintervalThehazardratioindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby**(P<0.
01)Liuetal.
BMCAnesthesiology(2016)16:46Page6of9APACHEII≥15andsuPAR≥10.
82ng/mLwereinde-pendentlyassociatedwithunfavorableoutcomewhileGiamarellos-Bourboulis'sstudyshowedthatAPACHEII≥17andsuPAR≥12ng/mlweretheoptimalcutoffs.
Third,weconstructedROCanalysisandcalculatedtheAUCtocomparetheperformanceofsuPAR,PCT,APA-CHEIIscore,andSOFAscoreaspredictorsofpoorout-come.
WefoundthatsuPARhadastrongpowerforpredictingunfavorableoutcomeassuggestedbyAUCof0.
788±0.
058,whichwaslessthanthatofAPACHEIIscore(0.
813±0.
055)butgreaterthanthatofSOFAscore(0.
779±0.
075)andPCT(0.
651±0.
081).
However,Giamarellos-Bourboulisetal.
justconductedROCana-lysiswithsuPARandAPACHEIIscoreasindependentvariablestopredictunfavorableoutcome.
Takento-gether,givenenrolledpatientswerefromdifferentethnicgroups,ourstudymayfurtherconfirmthepreliminaryconclusionthatapredictionrulewithfourlevelsofriskinsepsisbasedonAPACHEIIscoreandsuPARwasproposed.
Similartothefindingsofapreviousclinicaltrialcon-cerningplasmasuPARmeasurement[15],ourstudyclearlyshowedthatsuPARconcentrationswererelativelystableinthesystemiccirculationinbothsurvivorsandnon-survivorsduringthefirstweekofthediseasecourse.
Therefore,weinferthatthevalidityofthedevelopedprognosticationscoreremainsconstantevenifsuPARisnotmeasuredduringtheveryfirstdaysafterICUadmissionduetothestabilityofsuPARconcentra-tionsoverthediseasecourse.
Thesefindingswerecom-parabletootherdiseasesincludingchronicobstructivepulmonarydisease(COPD)[21]oracuterespiratorydis-tresssyndrome(ARDS)[22],inwhichsuPARwasregardedasanindependentpredictorforunfavorableoutcomes.
Severesepsishasareportedannualincidenceinadultsofupto300casesper100,000population[23,24].
Af-fectedpatientshavehighmortalities,complications,andresourceutilization.
Althoughfigureshaveimprovedintherecentyears[2,3],theriskfordeathremainshigh[25].
Consequently,improvingoutcomemaybeadaunt-ingwork.
Oneofpivotalmeasuresistoidentifythesep-ticpatientswithpoorprognosisrapidly[4].
OurstudysuggestedonecompositerulefordeterminingpatientswithsepsisathighriskonthebasisofAPACHEIIscoreandplasmasuPARconcentrations.
Actually,themeas-urementprocedureissosimplethatwecancompletethemeasurementforevery45patientsampleswithinabout4h.
Thepriceforthemeasurementisalsorela-tivelyreasonableandweonlyspend6,000CNY(about924USD)onevaluating45patientsamples,thatmeansweneedspendabout133CNY(20USD)onmeasuringTable5ValidationofthenovelstratificationruleAPACHEIIscoresuPARSurvivors,Number(%)Non-survivors,Number(%)PvalueOR(95%CI)<15<10.
8271(98.
61%)1(1.
39%)<0.
001**4.
72(3.
36–5.
81)≥10.
8224(88.
89%)3(11.
11%)≥15<10.
8213(72.
22%)5(27.
78%)<0.
001**2.
04(1.
85–3.
50)≥10.
829(45.
00%)11(55.
00%)Abbreviations:APACHEIIAcutePhysiologyandChronicHealthEvaluationII,suPARsolubleurokinaseplasminogenactivatorreceptor,ORoddsratio,CIconfidenceintervalTheORindicatestheriskofobtainingunfavorableoutcomeSignificantdifferencesaremarkedby**(P<0.
01)Fig.
4Kaplan-Meierestimatesofsurvivalofpatientsstratifiedintofourstrataofseverity.
Everystratumdifferedsignificantlyfromtheothers.
P=0.
002bythelog-ranktestwithinthefourdefinedstrata.
APACHEII,AcutePhysiologyandChronicHealthEvaluationII;suPAR,solubleurokinaseplasminogenactivatorreceptorLiuetal.
BMCAnesthesiology(2016)16:46Page7of9onepatientsample.
Undoubtedly,thesuPARmeasure-mentisrelativelycost-effective.
Therefore,giventhesimpleandinexpensivemeasurement,thecombinationofAPACHEIIscoreandplasmasuPARconcentrationsmaycontributetointensivecaremanagementinthesepticpatientsproperly.
Currently,evidencehassuggestedthatthevalueofsinglescoringsystemasastandardofclinicaldecision-makinginsepticpatientsisquestionable.
APACHEIIscoreislikelytorecognizeeitherlow-riskpatientsorvery-high-riskpatients,butnotthesepatientsbetweenthetwoextremes[20].
Theproposedriskstratificationrulefulfillsthisneedbecauseitdiscriminatesnotonlypatientslyingatoneofthetwoextremes-strata(A)and(D)-butalsopatientswithmoderatediseasesever-ity,namelypatientswithanAPACHEIIscoreoflessthan15andsuPARofatleast10.
82ng/mLorpatientswithanAPACHEIIscoreofatleast15andsuPARoflessthan10.
82ng/mL,whobelongtostrata(B)and(C),respectively.
ConclusionsInsummary,combinationofAPACHEIIscoreandsuPARmaysupplythepowerfulprognosticutilityforthemortalityofsepsis.
Ourfindingssuggestthatincorp-oratingsuPARintoAPACHEIIscoreasacompositeriskstratificationruleforsepsisisworthconsidering.
AbbreviationsAPACHEII,AcutePhysiologyandChronicHealthEvaluationII;ARDS,acuterespiratorydistresssyndrome;AUC,areaunderthecurve;CI,confidenceinterval;COPD,chronicobstructivepulmonarydisease;ICU,intensivecareunit;IQR,interquartileranges;OR,oddsratio;PCT,procalcitonin;ROC,receiveroperatingcharacteristic;SD,standarddeviation;SOFA,sequentialorganfailureassessment;suPAR,solubleurokinaseplasminogenactivatorreceptor;uPA,urokinaseplasminogenactivator;uPAR,urokinaseplasminogenactivatorreceptorAcknowledgementsNone.
FundingThisworkwasfinanciallysupportedbythegrantfromthe2013-2014Na-tionalClinicalKeySpecialtyConstructionProject.
AvailabilityofdataandmaterialsAlldatasetsarepresentedinthemainpaperoradditionalsupportingfiles.
Authors'contributionsXLandSPhavemadesubstantialcontributionstoconceptionanddesign,oracquisitionofdata,oranalysisandinterpretationofdata;XL,YS,andZLhavebeeninvolvedindraftingthemanuscriptorrevisingitcriticallyforimportantintellectualcontent;AFandHWhavegivenfinalapprovaloftheversiontobepublished;QGandSPhaveagreedtobeaccountableforallaspectsoftheworkinensuringthatquestionsrelatedtotheaccuracyorintegrityofanypartoftheworkareappropriatelyinvestigatedandresolved.
Allauthorsreadandapprovedthefinalmanuscript.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
ConsentforpublicationNotapplicable.
EthicsapprovalandconsenttoparticipateThestudywasapprovedbyShanghaiJiaotongUniversityXinhuaHospitalEthicsCommitteeandwascarriedoutinaccordancewiththeDeclarationofHelsinki.
Informedconsentswereobtainedfromallpatients.
Received:12January2016Accepted:15July2016References1.
ARISEInvestigators;ANZICSClinicalTrialsGroup,PeakeSL,DelaneyA,BaileyM,BellomoR,CameronPA,CooperDJ,HigginsAM,HoldgateA,HoweBD,etal.
Goal-directedresuscitationforpatientswithearlysepticshock.
NEnglJMed.
2014;371:1496–506.
2.
KaukonenKM,BaileyM,SuzukiS,PilcherD,BellomoR.
MortalityrelatedtoseveresepsisandsepticshockamongcriticallyillpatientsinAustraliaandNewZealand,2000–2012.
JAMA.
2014;311:1308–16.
3.
ReinhartK,DanielsR,KissoonN,O'BrienJ,MachadoFR,JimenezE,GSAExecutiveBoardandWSDExecutiveBoard.
Theburdenofsepsis-acalltoactioninsupportofWorldSepsisDay2013.
JCritCare.
2013;28:526–8.
4.
DellingerRP,LevyMM,RhodesA,AnnaneD,GerlachH,OpalSM,SevranskyJE,SprungCL,DouglasIS,JaeschkeR,etal.
SurvivingSepsisCampaign:internationalguidelinesformanagementofseveresepsisandsepticshock,2012.
IntensiveCareMed.
2013;39:165–228.
5.
Giamarellos-BourboulisEJ,Norrby-TeglundA,MylonaV,SavvaA,TsangarisI,DimopoulouI,MouktaroudiM,RaftogiannisM,GeorgitsiM,LinnérA,etal.
Riskassessmentinsepsis:anewprognosticationrulebyAPACHEIIscoreandserumsolubleurokinaseplasminogenactivatorreceptor.
CritCare.
2012;16:R149.
6.
VeraS,MartínezR,GormazJG,GajardoA,GalleguillosF,RodrigoR.
Novelrelationshipsbetweenoxidativestressandangiogenesis-relatedfactorsinsepsis:Newbiomarkersandtherapies.
AnnMed.
2015;47:289–300.
7.
HongDY,KimJW,PaikJH,JungHM,BaekKJ,ParkSO,LeeKR.
Valueofplasmaneutrophilgelatinase-associatedlipocalininpredictingthemortalityofpatientswithsepsisattheemergencydepartment.
ClinChimActa.
2015;452:177–81.
8.
LinderA,ArnoldR,BoydJH,ZindovicM,ZindovicI,LangeA,PaulssonM,NybergP,RussellJA,PritchardD,etal.
Heparin-BindingProteinMeasurementImprovesthePredictionofSevereInfectionWithOrganDysfunctionintheEmergencyDepartment.
CritCareMed.
2015;43:2378–86.
9.
HurM,KimH,KimHJ,YangHS,MagriniL,MarinoR,CardelliP,DiSommaS,GREATNetwork.
SolubleST2hasaprognosticroleinpatientswithsuspectedsepsis.
AnnLabMed.
2015;35:570–7.
10.
BackesY,vanderSluijsKF,MackieDP,TackeF,KochA,TenhunenJJ,SchultzMJ.
UsefulnessofsuPARasabiologicalmarkerinpatientswithsystemicinflammationorinfection:asystematicreview.
IntensiveCareMed.
2012;38:1418–28.
11.
MadsenCD,SideniusN.
Theinteractionbetweenurokinasereceptorandvitronectinincelladhesionandsignaling.
EurJCellBiol.
2008;87:617–29.
12.
MekonnenG,CorbanMT,HungOY,EshtehardiP,EapenDJ,Al-KassemH,Rasoul-ArzrumlyE,GogasBD,McDanielMC,PielakT,etal.
Plasmasolubleurokinase-typeplasminogenactivatorreceptorlevelisindependentlyassociatedwithcoronarymicrovascularfunctioninpatientswithnon-obstructivecoronaryarterydisease.
Atherosclerosis.
2015;239:55–60.
13.
TzanakakiG,PaparoupaM,KyprianouM,BarbouniA,Eugen-OlsenJ,Kourea-KremastinouJ.
ElevatedsolubleurokinasereceptorvaluesinCSF,ageandbacterialmeningitisinfectionareindependentandadditiveriskfactorsoffataloutcome.
EurJClinMicrobiolInfectDis.
2012;31:1157–62.
14.
HuttunenR,SyrjnenJ,VuentoR,HurmeM,HuhtalaH,LaineJ,PessiT,AittoniemiJ.
Plasmalevelofsolubleurokinase-typeplasminogenactivatorreceptorasapredictorofdiseaseseverityandcasefatalityinpatientswithbacteraemia:aprospectivecohortstudy.
JInternMed.
2011;270:32–40.
15.
KochA,VoigtS,KruschinskiC,SansonE,DückersH,HornA,YagmurE,ZimmermannH,TrautweinC,TackeF.
Circulatingsolubleurokinaseplasminogenactivatorreceptorisstablyelevatedduringthefirstweekoftreatmentintheintensivecareunitandpredictsmortalityincriticallyillpatients.
CritCare.
2011;15:R63.
16.
HoeniglM,RaggamRB,WagnerJ,ValentinT,LeitnerE,SeeberK,Zollner-SchwetzI,KrammerW,PrüllerF,GrisoldAJ,etal.
Diagnosticaccuracyofsolubleurokinaseplasminogenactivatorreceptor(suPAR)forpredictionofbacteremiainpatientswithsystemicinflammatoryresponsesyndrome.
ClinBiochem.
2013;46:225–9.
Liuetal.
BMCAnesthesiology(2016)16:46Page8of917.
OkuluE,ArsanS,AkinIM,AtesC,AlanS,KilicA,AtasayB.
SerumLevelsofSolubleUrokinasePlasminogenActivatorReceptorinInfantswithLate-onsetSepsis.
JClinLabAnal.
2015;29:347–52.
18.
LevyMM,FinkMP,MarshallJC,AbrahamE,AngusD,CookD,CohenJ,OpalSM,VincentJL,RamsayG,SCCM/ESICM/ACCP/ATS/SIS.
2001SCCM/ESICM/ACCP/ATS/SISinternationalsepsisdefinitionsconference.
CritCareMed.
2003;31:1250–6.
19.
CorrêaTD,SanchesPR,deMoraisLC,ScarinFC,SilvaE,BarbasCS.
Performanceofnoninvasiveventilationinacuterespiratoryfailureincriticallyillpatients:aprospective,observational,cohortstudy.
BMCPulmMed.
2015;15:144.
20.
VincentJL,OpalSM,MarshallJC.
TenreasonswhyweshouldNOTuseseverityscoresasentrycriteriaforclinicaltrialsorinourtreatmentdecisions.
CritCareMed.
2010;38:283–7.
21.
Can,GüzelantA,YerlikayaFH,Yosunkaya.
Theroleofserumsolubleurokinase-typeplasminogenactivatorreceptorinstablechronicobstructivepulmonarydisease.
JInvestigMed.
2014;62:938–43.
22.
GeboersDG,deBeerFM,Tuip-deBoerAM,vanderPollT,HornJ,CremerOL,BontenMJ,OngDS,SchultzMJ,BosLD.
PlasmasuPARasaprognosticbiologicalmarkerforICUmortalityinARDSpatients.
IntensiveCareMed.
2015;41:1281–90.
23.
JawadI,LukiI,RafnssonSB.
Assessingavailableinformationontheburdenofsepsis:globalestimatesofincidence,prevalenceandmortality.
JGlobHealth.
2012;2:010404.
24.
GaieskiDF,EdwardsJM,KallanMJ,CarrBG.
BenchmarkingtheincidenceandmortalityofseveresepsisintheUnitedStates.
CritCareMed.
2013;41:1167–74.
25.
HarrisonDA,WelchCA,EddlestonJM.
TheepidemiologyofseveresepsisinEngland,WalesandNorthernIreland,1996to2004:secondaryanalysisofahighqualityclinicaldatabase,theICNARCCaseMixProgrammeDatabase.
CritCare.
2006;10:R42.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Liuetal.
BMCAnesthesiology(2016)16:46Page9of9
- higherapche相关文档
- organismsapche
- highapche
- aminoapche
- 规则apche
- 第二军医大学学报AcadJS
- Figapche
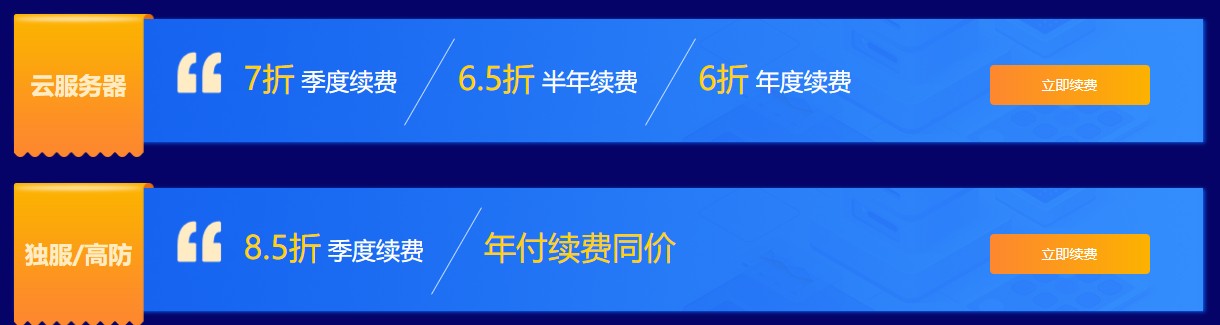
华纳云,3折低至优惠云服务器,独立服务器/高防御服务器低至6折,免备案香港云服务器CN2 GIA三网直连线路月付18元起,10Mbps带宽不限流量
近日华纳云发布了最新的618返场优惠活动,主要针对旗下的免备案香港云服务器、香港独立服务器、香港高防御服务器等产品,月付6折优惠起,高防御服务器可提供20G DDOS防御,采用E5处理器V4CPU性能,10Mbps独享CN2 GIA高速优质带宽,有需要免备案香港服务器、香港云服务器、香港独立服务器、香港高防御服务器、香港物理服务器的朋友可以尝试一下。华纳云好不好?华纳云怎么样?华纳云服务器怎么样?...
新加坡云服务器 1核2Gg 46元/月 香港云服务器 1核2G 74元/月 LightNode
LightNode是一家成立于2002年,总部位于香港的VPS服务商。提供基于KVM虚拟化技术.支持CentOS、Ubuntu或者Windows等操作系统。公司名:厦门靠谱云股份有限公司官方网站:https://www.lightnode.com拥有高质量香港CN2 GIA与东南亚节点(河内、曼谷、迪拜等)。最低月付7.71美金,按时付费,可随时取消。灵活满足开发建站、游戏应用、外贸电商等需求。首...

腾讯云CVM云服务器大硬盘方案400GB和800GB数据盘方案
最近看到群里的不少网友在搭建大数据内容网站,内容量有百万篇幅,包括图片可能有超过50GB,如果一台服务器有需要多个站点的话,那肯定默认的服务器50GB存储空间是不够用的。如果单独在购买数据盘会成本提高不少。这里我们看到腾讯云促销活动中有2款带大数据盘的套餐还是比较实惠的,一台是400GB数据盘,一台是800GB数据盘,适合他们的大数据网站。 直达链接 - 腾讯云 大数据盘套餐服务器这里我们看到当前...

apche为你推荐
-
主机空间如何租用主机或申请免费空间。海外虚拟主机空间有免费的性能好的国外虚拟主机空间吗?vps试用请问有什么网站可以提供免费vps试用的?想用它来刷一下外国pt站成都虚拟空间空间服务商那个好深圳网站空间深圳网站设计 哪家好一些?北京网站空间自己弄一个简单的网站,大概需要办理什么,大概需要多少钱?虚拟主机控制面板万网的虚拟主机控制面板指的是什么呢?上海虚拟主机帮忙推荐一下哪里的虚拟主机比较好?重庆虚拟主机万网M3型虚拟主机怎么样?速度如何?淘宝虚拟主机淘宝里卖虚拟主机、独立服务器、VPS的都是怎么进货的。