ferentiatedwww.97yes.com
www.97yes.com 时间:2021-03-19 阅读:()
RESEARCHOpenAccessLymph-noderatioisanindependentprognosticfactorinpatientswithstageIIIcolorectalcancer:aretrospectivestudyfromtheMiddleEastEliasElias1,DeborahMukherji1,WalidFaraj2,MohammadKhalife2,HaniDimassi3,MohamadEloubeidi4,HasanHattoum5,GhassanKAbou-Alfa6,AhmadSaleh1andAliShamseddine1*AbstractBackground:Inthisretrospectivestudy,weevaluatedtheprognosticeffectofpositivelymph-noderatio(pLNR)onpatientswithstageIIIcolorectalcancer(CRC).
Ourpaperisthefirstanalysis,toourknowledge,todealwithsuchdatafromtheMiddleEast.
Methods:Weanalyzedtheclinicopathologicaldataof535patientsdiagnosedwithcolorectalcanceratourinstitutionbetween1983and2003.
The164patientsdiagnosedwithstageIIIdiseaseweredividedintotwocategoriesbasedonlymph-noderatio(LNR)beingtheratioofpositivelymphnodesovertotallymphnodesdissected:LNR≤0.
4andLNR>0.
4.
WeusedKaplan-MeierandCoxproportionalhazardmodelstoevaluatetheprognosticeffectofpLNR.
Results:The10-yearsurvivalrateforthepatientswithstageIIIA,IIIBandIIICcancerswere76%,56%and0%respectively(P=0.
014).
UsingpLNRof0.
4asthecutoffpointwasfoundtoyieldclinicallyandsignificantresults,withasignificantdifferenceintheoutcomesofpatientswithpLNR≤0.
4comparedtothosewithpLNR>0.
4(hazardratio=5.
25,95%confidenceinterval=1.
2to22.
1,P=0.
02).
Conclusion:Theratio-basedstaging(pLNR)ofCRCisamoreaccurateandclinicallyusefulprognosticmethodthanthenumberofpositiveLNsresectedorthetotalnumberofLNsretrievedforpredictingthecourseofpatientswithstageIIICRC.
Keywords:Colorectalcancer,StageIII,Lymphnoderatio,PrognosisBackgroundColorectalcancer(CRC)isthethirdmostcommoncan-cerinbothfemaleandmalepopulations[1].
Currently,itsprogressionisstagedusingtheTNM(tumor,node,metastasis)stagingsystemaccordingtotumorsize,lymph-nodeinvolvementanddistantmetastases,asrecommendedbytheAmericanJointCommitteeonCancer(AJCC)[2].
However,manyinvestigatorshavequestionedtheprognosticpoweroftheTNMsystembe-causeofthepossibilityofstagemigration,andhavepro-posedalternativeprognosticmethods.
Onenotablealternativebasesapatient'sprognosisuponthetotalnumberofLNsresected.
Thisconcepthaslongbeendebatedintheliterature.
ManystudieshaveshownthatahighernumberofLNsretrievedleadstomoreaccuratestagingandapparentlyimprovedsurvivaloutcomes[3-8].
Furthermore,astudyconductedbytheNationalCancerInstitute(NCI)involving60,000patientsillustratedarelationshipbetweenthenumberofresectedpositiveLNsandthesurvivalrateinstageIIIpatients[9].
ThisrelationshiphasdrivenstudiesthathaveattempedtosetrecommendationsforthenumberofLNsthatshouldberesected.
TheNCIandtheRoyalCollegeofPathologists(RCP)agreeontherecommenda-tionforaminimumof12LNstoberesected[10].
Someresearchershavealsoinvestigatedtheimport-anceofthenumberofnegativeLNsretrievedonthe*Correspondence:as04@aub.
edu.
lb1DivisionofHematologyandOncology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,LebanonFulllistofauthorinformationisavailableattheendofthearticle2012Eliasetal.
;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63WORLDJOURNALOFSURGICALONCOLOGYhttp://www.
wjso.
com/content/10/1/63survivaloutcome[11],butfurtherstudiesarerequiredinthisarea.
MethodssuchasusingthepositiveLNratio(pLNR;thenumberofpositiveLNsdividedbythetotalnumberofLNsresected)havebeenreportedassignificantprog-nosticfactorsinmalignanciesofthepancreas,stomach,bladder,breastandesophagus[12-15],buttheimport-anceofthepLNRasaprognosticfactorincoloncancerisstillbeingexplored.
Inthisretrospectivestudy,weaimedtoevaluatetheimportanceofpLNRasaprognosticparameteronthesurvivalofpatientsdiagnosedwithstageIIIcoloncancerinourpopulation,andtocompareitsprognosticpoweragainstothermethods,suchasthetotalnumberofLNsandthenumberofpositiveLNsresected.
Toourknow-ledge,itisthefirststudytodealwiththistopicintheMiddleEast,hencewereliedontheworldliteratureforpurposesofcomparisonandreferences.
MethodsThestudyenrolled535patientswhowerediagnosedwithCRCatourinstitutionbetween1983and2003.
Ofthe535patients,164werediagnosedwithstageIIIdis-ease,whichconstitutedthesampletobeanalyzed.
Theclinicopathologicalvariablesreviewedincludedageatpresentation,gender,personalandfamilymedicalhis-tory,socialhabits,symptoms,sitesofneoplasms,diag-nostictools,pathologyresults,grade,TNMstaging,typeofsurgeryundergone,adjuvanttherapy,andsurvivalrate.
Wedefinedsurvivalrateasoverallsurvivalfromthetimeofdiagnosistoeitherthetimeofdeathorthelastfollow-up.
Tumorgradewasclassifiedaslow-grade(wellormoderatelydifferentiated)andhigh-grade(poorlydif-ferentiated,anaplastic,orundifferentiated).
Curativere-sectionwasdefinedasclearpathologicalmarginsaftersurgery,andthefollow-upperiodwas10years.
StatisticalanalysisAbstracteddatafromthemedicalrecordsofthe535patientswerecodedandanalyzedusingSPSS(software,version18;SPSSInc.
,Chicago,IL,USA).
Summarysta-tisticswerecomputedforpatientswithstageIIIdisease.
Survivalratesat1,5and10yearswerecomputedusingtheKaplan-Meiermethod,andthelogranktestwasusedtocalculatetheP-valuesforthedifferentvariables.
AmultivariatemodelusingtheCoxproportionatehaz-ardtechniquewascreatedusingageandgenderoftheparticipantsascontrolvariables,andallsignificantvari-ablesatthebivariatelevel,aswellasimportantprognos-ticvariablessuchastreatmentandnumberofpositiveLNs.
Coefficientsandstandarderrorswereexponen-tiatedtocreatehazardratios(HR)and95%confidenceintervals.
P0.
4(41;25.
2%)(Figure1b).
Moreover,whenstratifyingourdataaccordingtopositiveLNandLNRwegottheresultsascitedinTable2.
UnivariateanalysisStratifyingstageIIIpatientsalone,survivalat1,5and10years,respectively,was91%,75.
8%and75.
8%forstageIIIA;94%,77.
1%and56%forstageIIIB,and84.
7%,22%and0%forstageIIICrespectively(Table3,Figure2).
SurvivalforpatientsgradedN1andN2was58.
4%and19.
2%at10yearsrespectively(Table3,Figure3).
ThetotalnumberofLNsresectedwasnotfoundtobeasignificantpredictorofsurvivalunderunivariateana-lysis(P=0.
45),buttherewasasignificantproportionalcorrelationbetweenthetotalnumberofLNsresectedandthenumberofpositiveLNsretrieved(P4,survivalat1,5and10yearswas(Table3,Figure4).
MultivariateanalysisTheCoxproportionatehazardmodelwasusedtoanalyzesurvivalrates,andcontrolledforage,gender,stageIIIstrata(AB,andC),adjuvanttherapy,numberofpositiveLNs,andpLNR.
LNR>0.
4,controlledforalltheothervariables,gaveHR=5.
25,95%CI=1.
2to22.
1.
P=0.
02(Table5).
DiscussionAccuratestagingofcolorectalcancerisessentialforap-propriatetherapeuticplanning.
TheTNMstagingsystemhastakenoverfromthepathologicalDuke'sstagingsys-tem,howeveritprovideslimitedprognosticinformationFigure1DistributionofthenumberofdissectedLNs(LNs).
(a)Onaverage,21lymphnodesweredissected(median18).
ThedistributionofdissectedLNsshowedthatmostofthecaseshadbetween2and40LNsremoved,withthedistributionskewedpositivelytotherightbysomescatteredcaseswithahighernumberofdissectedLNs.
(b)DistributionoftheratioofpositivetodissectedLNs(lymph-noderatio;LNR).
TheaverageratioofpositivetodissectedLNswas0.
29(median0.
17),with50%ofthecasesbeingbetween0.
01and0.
17,and75%ofthecasesbetween0.
01and0.
42.
Thereisaapositiveskewtotheright.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page3of7http://www.
wjso.
com/content/10/1/63regardingtheheterogeneousgroupofpatientswithstageIIIdisease.
Novelprognosticmethodsbasedonthreedif-ferentparametershadbeeninvestigated:thetotalnum-berofLNscollectedthenumberofpositiveLNsretrieved,andthepositiveLNR.
Theaimofourretrospectivestudywastocompareandre-evaluatedifferentapproachesforCRCprognosisinourpopulationofpatientswithstageIIIdisease.
AccordingtotheAJCC[2],stageIIICRCisdefinedbythedepthoftumorinvasionandtheextentofLNin-volvementinnon-metastaticcarcinomas.
Long-termsurvivalratesdependonandareinverselyproportionaltothenumberofLNsinvolved.
AlthoughtheTNMsys-temisareliabletherapeuticguide,stagemigration,are-sultofinaccurateTNMstaging,hasmadeestimationoffuturesurvivalrateinconsistent.
Furthermore,stageIIIcolorectalcancerissubdividedintoA,B,andCaccord-ingtothenumberofLNsinvolved,butthisnumbermayvarywiththetotalnumberofLNsextracted[7,16,17].
ThetotalnumberofLNsretrievedmaybeaffectedbyfactorssuchasages,gender,bodymassindex,surgicaltechniqueandthelocationofthetumor.
Right-sidedtumorstendtoyieldahighernumberofretrievableLNsthanleft-sidedtumors[18].
TheNCIandRCPbothrec-ommendaminimumof12nodesshouldberetrieved[10],butthereisnogeneralconsensusontheexactnumberofLNsthatmustberemoved,andsurgeonsshouldgenerallyremoveasmanyLNsaspossible[11,19].
TakingintoconsiderationallthevariablesabovethatcouldaffectthetotalnumberofLNsretrieved,ourinstitutionhasmaintainedahighresectionnumberoveraperiodof20years(mean20.
8,range2–88)(Table1).
Reviewingourdata,wedidnotfindbyunivariateana-lysisasignificantcorrelationbetweenthetotalnumberofLNsresectedandthesurvivalrateofthepatients(P=0.
46).
Thisislikelytoreflectthehighstandardsoflymphadenectomy,withfewpatientsinthispopulationbeingunderstaged.
Ourfindingsareconsistentwithan-otherstudyconductedusingSurveillance,EpidemiologyTable2CrosstabulationofthevariablesaccordingtoLNRandpositiveLNCharacteristicsLNRN(%)P-valuePositiveLNP-value0–0.
4>0.
41–34+Age38(69.
1)17(30.
9)0.
74331(55.
4)25(44.
6)0.
3271StageIIIIIIA12(100)0(0)713980.
5±7.
468.
5±10.
168.
5±10.
10.
25LNR0to0.
411694.
1±2.
377.
3±5.
860.
6±9.
9>0.
44186.
2±6.
640.
6±13.
4046389.
2±4.
751.
1±13.
119.
2±15.
53positiveLNs).
Figure3SurvivalcurveforpatientswithstageIIIcolorectalcancer,stratifiedasIIIA,IIIBandIIIC.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page5of7http://www.
wjso.
com/content/10/1/63removed)andthensubdividedeachgroupintotwocat-egories(N1andN2,respectively)(Table5).
OuranalysisconfirmedthatthenumberofpositiveLNsretrieveddir-ectlycorrelatedwiththetotalnumberofLNscollected.
However,whenweusedmultivariateanalysisonthenumberofpositiveLNscollected,alongwithpLNR,tumorstage,andotherfactorssuchasageandgender,thenumberofpositiveLNswasnotfoundtobesignifi-cant(P=0.
35).
OurresultsareconsistentwithananalysisbyMougetal.
[18],whocomparedthenumberofpositiveLNsandthepLNRinbothunivariateandmultivariateanalysis.
pLNRmaintaineditssignificanceasaprognosticfactorinbothmodels,whereasthenumberofpositiveLNswasnotfoundtobesignificantwhencomputedalongotherfactorsinthemultivariatemodel(Tables3,4).
ToovercomeanyfactorsthatcanaffecttheyieldofLNs,weevaluatedaratio-basedclassification,thepositiveLNratio(pLNR).
ThisratiotakesintoaccountboththetotalnumberofLNsretrievedandtheactualnumberofpositiveLNsfound.
Becauseitdoesnotrelyononevariable,thepLNRovercomesseverallimitationspertainingtototalLNcollection,includingsurgicalandpathologicaltechniques,tumorsites,andeventheminimumnumberofLNsthatshouldbedissected[18].
Thismethodhasalreadybeenusedasaprognostictoolforothertumorssuchasgastric,pancreatic,andbreast[12-15].
MultiplecutoffpointsforpLNRhavebeenhavebeenpresentedintheliterature.
Bergeretal.
used0.
4[4].
OurpLNRstratificationusing0.
4asthecutoffpointisconsistentwiththeworkofDeRidderetal.
[20],whousedthesamethreshold.
Asexpected,ourunivariateanalysisshowedthatpatientswithstageIIIAhadabetter10-yearsdisease-freesurvivalrate(75.
8%)thanthosewithstageIIIB(56%)orstageIIIC(nopatientssurvived)(P=0.
01)(Figure2).
ItalsoshowedthatpLNRhadathresholdvalueof0.
4,withpatientshavingbettersurvivalwhentheratiowas≤0.
4(10-yearsurvivalof60.
6%,comparedto0%survivalinpatientswithratio>0.
4)(P702.
4622.
98GenderFemale10.
499-2.
0080.
99810.
39to2.
250.
88Male1.
0010.
93LNR≤0.
411.
472to6.
2340.
00311.
25to22.
120.
02>0.
43.
035.
25StageIIIA10.
318to5.
9560.
66810.
24to5.
630.
86IIIB1.
3770.
836to17.
670.
0841.
150.
21to14.
640.
60IIIC3.
8421.
76PositiveLN1–310.
993to4.
1850.
05210.
12to2.
080.
35≥42.
0390.
51AdjchemoNo10.
279to1.
2350.
1610.
21to1.
270.
15Yes0.
5860.
52Adjchemo,adjuvantchemotherapy;LN,lymphnode;LNR,lymph-noderatio.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page6of7http://www.
wjso.
com/content/10/1/63adjuvantchemotherapy,andpLNR.
StageIII,althoughfoundtobesignificantintheunivariatemodel,lostitspowerwhencomputedalongsidepLNR.
Moreover,pLNR>0.
4provedtohavethemostsignificantprognos-ticfactor(HR=5.
25,CI=1.
2to22.
1,P<0.
05),showingthatpLNRisindeedanindependentprognosticfactorforsurvivalinpatientswithstageIIICRC.
Alimitationofouristhatitwasaretrospectivereviewandtherewassomelossoffollow-upforafewfewpatients.
Nonetheless,theresultsconfirmpreviousstud-iesregardingtheprognosticpoweroftheLNRinthecolorectaldisease.
WehavetonotethatourmanuscriptisthefirstsuchstudytobeconductedintheMiddleEast.
ConclusionOurstudyconfirmstheprognosticvalueoftheratio-basedpLNRmodeltopredicsurvivalofpatientswithstageIIICRCrelativetostage(AJCC),numberofposi-tiveLNs,andtotalLNsretrieved.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authordetails1DivisionofHematologyandOncology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
2DivisionofHepatobiliaryandGastricsurgery,DepartmentofGeneralSurgeryAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
3SchoolofPharmacy,LebaneseAmericanUniversity,Byblos,Lebanon.
4DivisionofGastroenterology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
5DepartmentofInternalMedicine,StatenIslandUniversityHospital,475SeaviewAve,StatenIsland,NY10305,USA.
6MemorialSloan-KetteringCancerCenter,NewYork,NYandWeillMedicalCollegeatCornellUniversity,NewYork,NY.
Authors'contributionsEE,SA,HHandKMdesignedthestudy;EEandHHcollectedthedata;EEdraftedthepaper;SAsupervisedthestudy;andFWandMDeditedandcorrectedthemanuscript.
DH(PhDstatistician)carriedthestatisticalanalysiswiththehelpofMOandCMwhoparticipatedalsoindoingsomepartsoftheanalysis.
Allauthorsreadandapprovedthefinalmanuscript.
Received:9December2011Accepted:25April2012Published:25April2012References1.
JemalA,SiegelR,WardE,etal:Cancerstatistics,2009.
CACancerJClin2009,59:225–249.
2.
EdgeSB,ComptonCC:TheAmericanJointCommitteeonCancer:the7theditionoftheAJCCcancerstagingmanualandthefutureofTNM.
AnnSurgOncol2010,17:1471–1474.
3.
CaplinS,CerottiniJP,BosmanFT,etal:ForpatientswithDukes'B(TNMStageII)colorectalcarcinoma,examinationofsixorfewerlymphnodesisrelatedtopoorprognosis.
Cancer1998,83:666–672.
4.
BergerAC,SigurdsonER,LeVoyerT,etal:Coloncancersurvivalisassociatedwithdecreasingratioofmetastatictoexaminedlymphnodes.
JClinOncol2005,23:8706–8712.
5.
LeVoyerTE,SigurdsonER,HanlonAL,etal:Coloncancersurvivalisassociatedwithincreasingnumberoflymphnodesanalyzed:asecondarysurveyofintergrouptrialINT-0089.
JClinOncol2003,21:2912–2919.
6.
EdlerD,OhrlingK,HallstromM,etal:Thenumberofanalyzedlymphnodes-aprognosticfactorincolorectalcancer.
ActaOncol2007,46:975–981.
7.
SwansonRS,ComptonCC,StewartAK,etal:TheprognosisofT3N0coloncancerisdependentonthenumberoflymphnodesexamined.
AnnSurgOncol2003,10:65–71.
8.
WongSL,JiH,HollenbeckBK,etal:Hospitallymphnodeexaminationratesandsurvivalafterresectionforcoloncancer.
JAMA2007,298:2149–2154.
9.
ChangGJ,Rodriguez-BigasMA,SkibberJM,etal:Lymphnodeevaluationandsurvivalaftercurativeresectionofcoloncancer:systematicreview.
JNatlCancerInst2007,99:433–441.
10.
RoyalCollegeofPathologists:StandardsandDatasetforReportingCancers:Datasetforcolorectalcancer(2ndedition).
Availableat:http://www.
rcpath.
org/resources/pdf/G049-ColorectalDataset-Sep07.
pdf.
Accessedon29,March,2011.
11.
JohnsonPM,PorterGA,RicciardiR,etal:Increasingnegativelymphnodecountisindependentlyassociatedwithimprovedlong-termsurvivalinstageIIIBandIIICcoloncancer.
JClinOncol2006,24:3570–3575.
12.
HatoumHA,JamaliFR,El-SaghirNS,etal:Ratiobetweenpositivelymphnodesandtotalexcisedaxillarylymphnodesasanindependentprognosticfactorforoverallsurvivalinpatientswithnonmetastaticlymphnode-positivebreastcancer.
AnnSurgOncol2009,16:3388–3395.
13.
PawlikTM,GleisnerAL,CameronJL,etal:Prognosticrelevanceoflymphnoderatiofollowingpancreaticoduodenectomyforpancreaticcancer.
Surgery2007,141:610–618.
14.
MarietteC,PiessenG,BriezN,etal:Thenumberofmetastaticlymphnodesandtheratiobetweenmetastaticandexaminedlymphnodesareindependentprognosticfactorsinesophagealcancerregardlessofneoadjuvantchemoradiationorlymphadenectomyextent.
AnnSurg2008,247:365–371.
15.
MarchetA,MocellinS,AmbrosiA,NittiD:ItalianResearchGroupforGastricCancer(IRGGC),etal:Theratiobetweenmetastaticandexaminedlymphnodes(Nratio)isanindependentprognosticfactoringastriccancerregardlessofthetypeoflymphadenectomy:resultsfromanItalianmulticentricstudyin1853patients.
AnnSurg2007,245:543–552.
16.
JosephNE,SigurdsonER,HanlonAL,etal:Accuracyofdeterminingnodalnegativityincolorectalcanceronthebasisofthenumberofnodesretrievedonresection.
AnnSurgOncol2003,10:213–218.
17.
GoldsteinNS,SanfordW,CoffeyM,etal:Lymphnoderecoveryfromcolorectalresectionspecimensremovedforadenocarcinoma.
Trendsovertimeandarecommendationforaminimumnumberoflymphnodestoberecovered.
AmJClinPathol1996,106:209–216.
18.
MougSJ,SaldanhaJD,McGregorJR,etal:Positivelymphnoderetrievalratiooptimisespatientstagingincolorectalcancer.
BrJCancer2009,100:1530–1533.
19.
VatherR,SammourT,KahokehrA,etal:Lymphnodeevaluationandlong-termsurvivalinStageIIandStageIIIcoloncancer:anationalstudy.
AnnSurgOncol2009,16:585–593.
20.
DeRidderM,Vinh-HungV,VanNieuwenhoveY,etal:Prognosticvalueofthelymphnoderatioinnodepositivecoloncancer.
Gut2006,55:1681.
doi:10.
1186/1477-7819-10-63Citethisarticleas:Eliasetal.
:Lymph-noderatioisanindependentprognosticfactorinpatientswithstageIIIcolorectalcancer:aretrospectivestudyfromtheMiddleEast.
WorldJournalofSurgicalOncology201210:63.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitEliasetal.
WorldJournalofSurgicalOncology2012,10:63Page7of7http://www.
wjso.
com/content/10/1/63
Ourpaperisthefirstanalysis,toourknowledge,todealwithsuchdatafromtheMiddleEast.
Methods:Weanalyzedtheclinicopathologicaldataof535patientsdiagnosedwithcolorectalcanceratourinstitutionbetween1983and2003.
The164patientsdiagnosedwithstageIIIdiseaseweredividedintotwocategoriesbasedonlymph-noderatio(LNR)beingtheratioofpositivelymphnodesovertotallymphnodesdissected:LNR≤0.
4andLNR>0.
4.
WeusedKaplan-MeierandCoxproportionalhazardmodelstoevaluatetheprognosticeffectofpLNR.
Results:The10-yearsurvivalrateforthepatientswithstageIIIA,IIIBandIIICcancerswere76%,56%and0%respectively(P=0.
014).
UsingpLNRof0.
4asthecutoffpointwasfoundtoyieldclinicallyandsignificantresults,withasignificantdifferenceintheoutcomesofpatientswithpLNR≤0.
4comparedtothosewithpLNR>0.
4(hazardratio=5.
25,95%confidenceinterval=1.
2to22.
1,P=0.
02).
Conclusion:Theratio-basedstaging(pLNR)ofCRCisamoreaccurateandclinicallyusefulprognosticmethodthanthenumberofpositiveLNsresectedorthetotalnumberofLNsretrievedforpredictingthecourseofpatientswithstageIIICRC.
Keywords:Colorectalcancer,StageIII,Lymphnoderatio,PrognosisBackgroundColorectalcancer(CRC)isthethirdmostcommoncan-cerinbothfemaleandmalepopulations[1].
Currently,itsprogressionisstagedusingtheTNM(tumor,node,metastasis)stagingsystemaccordingtotumorsize,lymph-nodeinvolvementanddistantmetastases,asrecommendedbytheAmericanJointCommitteeonCancer(AJCC)[2].
However,manyinvestigatorshavequestionedtheprognosticpoweroftheTNMsystembe-causeofthepossibilityofstagemigration,andhavepro-posedalternativeprognosticmethods.
Onenotablealternativebasesapatient'sprognosisuponthetotalnumberofLNsresected.
Thisconcepthaslongbeendebatedintheliterature.
ManystudieshaveshownthatahighernumberofLNsretrievedleadstomoreaccuratestagingandapparentlyimprovedsurvivaloutcomes[3-8].
Furthermore,astudyconductedbytheNationalCancerInstitute(NCI)involving60,000patientsillustratedarelationshipbetweenthenumberofresectedpositiveLNsandthesurvivalrateinstageIIIpatients[9].
ThisrelationshiphasdrivenstudiesthathaveattempedtosetrecommendationsforthenumberofLNsthatshouldberesected.
TheNCIandtheRoyalCollegeofPathologists(RCP)agreeontherecommenda-tionforaminimumof12LNstoberesected[10].
Someresearchershavealsoinvestigatedtheimport-anceofthenumberofnegativeLNsretrievedonthe*Correspondence:as04@aub.
edu.
lb1DivisionofHematologyandOncology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,LebanonFulllistofauthorinformationisavailableattheendofthearticle2012Eliasetal.
;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63WORLDJOURNALOFSURGICALONCOLOGYhttp://www.
wjso.
com/content/10/1/63survivaloutcome[11],butfurtherstudiesarerequiredinthisarea.
MethodssuchasusingthepositiveLNratio(pLNR;thenumberofpositiveLNsdividedbythetotalnumberofLNsresected)havebeenreportedassignificantprog-nosticfactorsinmalignanciesofthepancreas,stomach,bladder,breastandesophagus[12-15],buttheimport-anceofthepLNRasaprognosticfactorincoloncancerisstillbeingexplored.
Inthisretrospectivestudy,weaimedtoevaluatetheimportanceofpLNRasaprognosticparameteronthesurvivalofpatientsdiagnosedwithstageIIIcoloncancerinourpopulation,andtocompareitsprognosticpoweragainstothermethods,suchasthetotalnumberofLNsandthenumberofpositiveLNsresected.
Toourknow-ledge,itisthefirststudytodealwiththistopicintheMiddleEast,hencewereliedontheworldliteratureforpurposesofcomparisonandreferences.
MethodsThestudyenrolled535patientswhowerediagnosedwithCRCatourinstitutionbetween1983and2003.
Ofthe535patients,164werediagnosedwithstageIIIdis-ease,whichconstitutedthesampletobeanalyzed.
Theclinicopathologicalvariablesreviewedincludedageatpresentation,gender,personalandfamilymedicalhis-tory,socialhabits,symptoms,sitesofneoplasms,diag-nostictools,pathologyresults,grade,TNMstaging,typeofsurgeryundergone,adjuvanttherapy,andsurvivalrate.
Wedefinedsurvivalrateasoverallsurvivalfromthetimeofdiagnosistoeitherthetimeofdeathorthelastfollow-up.
Tumorgradewasclassifiedaslow-grade(wellormoderatelydifferentiated)andhigh-grade(poorlydif-ferentiated,anaplastic,orundifferentiated).
Curativere-sectionwasdefinedasclearpathologicalmarginsaftersurgery,andthefollow-upperiodwas10years.
StatisticalanalysisAbstracteddatafromthemedicalrecordsofthe535patientswerecodedandanalyzedusingSPSS(software,version18;SPSSInc.
,Chicago,IL,USA).
Summarysta-tisticswerecomputedforpatientswithstageIIIdisease.
Survivalratesat1,5and10yearswerecomputedusingtheKaplan-Meiermethod,andthelogranktestwasusedtocalculatetheP-valuesforthedifferentvariables.
AmultivariatemodelusingtheCoxproportionatehaz-ardtechniquewascreatedusingageandgenderoftheparticipantsascontrolvariables,andallsignificantvari-ablesatthebivariatelevel,aswellasimportantprognos-ticvariablessuchastreatmentandnumberofpositiveLNs.
Coefficientsandstandarderrorswereexponen-tiatedtocreatehazardratios(HR)and95%confidenceintervals.
P0.
4(41;25.
2%)(Figure1b).
Moreover,whenstratifyingourdataaccordingtopositiveLNandLNRwegottheresultsascitedinTable2.
UnivariateanalysisStratifyingstageIIIpatientsalone,survivalat1,5and10years,respectively,was91%,75.
8%and75.
8%forstageIIIA;94%,77.
1%and56%forstageIIIB,and84.
7%,22%and0%forstageIIICrespectively(Table3,Figure2).
SurvivalforpatientsgradedN1andN2was58.
4%and19.
2%at10yearsrespectively(Table3,Figure3).
ThetotalnumberofLNsresectedwasnotfoundtobeasignificantpredictorofsurvivalunderunivariateana-lysis(P=0.
45),buttherewasasignificantproportionalcorrelationbetweenthetotalnumberofLNsresectedandthenumberofpositiveLNsretrieved(P4,survivalat1,5and10yearswas(Table3,Figure4).
MultivariateanalysisTheCoxproportionatehazardmodelwasusedtoanalyzesurvivalrates,andcontrolledforage,gender,stageIIIstrata(AB,andC),adjuvanttherapy,numberofpositiveLNs,andpLNR.
LNR>0.
4,controlledforalltheothervariables,gaveHR=5.
25,95%CI=1.
2to22.
1.
P=0.
02(Table5).
DiscussionAccuratestagingofcolorectalcancerisessentialforap-propriatetherapeuticplanning.
TheTNMstagingsystemhastakenoverfromthepathologicalDuke'sstagingsys-tem,howeveritprovideslimitedprognosticinformationFigure1DistributionofthenumberofdissectedLNs(LNs).
(a)Onaverage,21lymphnodesweredissected(median18).
ThedistributionofdissectedLNsshowedthatmostofthecaseshadbetween2and40LNsremoved,withthedistributionskewedpositivelytotherightbysomescatteredcaseswithahighernumberofdissectedLNs.
(b)DistributionoftheratioofpositivetodissectedLNs(lymph-noderatio;LNR).
TheaverageratioofpositivetodissectedLNswas0.
29(median0.
17),with50%ofthecasesbeingbetween0.
01and0.
17,and75%ofthecasesbetween0.
01and0.
42.
Thereisaapositiveskewtotheright.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page3of7http://www.
wjso.
com/content/10/1/63regardingtheheterogeneousgroupofpatientswithstageIIIdisease.
Novelprognosticmethodsbasedonthreedif-ferentparametershadbeeninvestigated:thetotalnum-berofLNscollectedthenumberofpositiveLNsretrieved,andthepositiveLNR.
Theaimofourretrospectivestudywastocompareandre-evaluatedifferentapproachesforCRCprognosisinourpopulationofpatientswithstageIIIdisease.
AccordingtotheAJCC[2],stageIIICRCisdefinedbythedepthoftumorinvasionandtheextentofLNin-volvementinnon-metastaticcarcinomas.
Long-termsurvivalratesdependonandareinverselyproportionaltothenumberofLNsinvolved.
AlthoughtheTNMsys-temisareliabletherapeuticguide,stagemigration,are-sultofinaccurateTNMstaging,hasmadeestimationoffuturesurvivalrateinconsistent.
Furthermore,stageIIIcolorectalcancerissubdividedintoA,B,andCaccord-ingtothenumberofLNsinvolved,butthisnumbermayvarywiththetotalnumberofLNsextracted[7,16,17].
ThetotalnumberofLNsretrievedmaybeaffectedbyfactorssuchasages,gender,bodymassindex,surgicaltechniqueandthelocationofthetumor.
Right-sidedtumorstendtoyieldahighernumberofretrievableLNsthanleft-sidedtumors[18].
TheNCIandRCPbothrec-ommendaminimumof12nodesshouldberetrieved[10],butthereisnogeneralconsensusontheexactnumberofLNsthatmustberemoved,andsurgeonsshouldgenerallyremoveasmanyLNsaspossible[11,19].
TakingintoconsiderationallthevariablesabovethatcouldaffectthetotalnumberofLNsretrieved,ourinstitutionhasmaintainedahighresectionnumberoveraperiodof20years(mean20.
8,range2–88)(Table1).
Reviewingourdata,wedidnotfindbyunivariateana-lysisasignificantcorrelationbetweenthetotalnumberofLNsresectedandthesurvivalrateofthepatients(P=0.
46).
Thisislikelytoreflectthehighstandardsoflymphadenectomy,withfewpatientsinthispopulationbeingunderstaged.
Ourfindingsareconsistentwithan-otherstudyconductedusingSurveillance,EpidemiologyTable2CrosstabulationofthevariablesaccordingtoLNRandpositiveLNCharacteristicsLNRN(%)P-valuePositiveLNP-value0–0.
4>0.
41–34+Age38(69.
1)17(30.
9)0.
74331(55.
4)25(44.
6)0.
3271StageIIIIIIA12(100)0(0)713980.
5±7.
468.
5±10.
168.
5±10.
10.
25LNR0to0.
411694.
1±2.
377.
3±5.
860.
6±9.
9>0.
44186.
2±6.
640.
6±13.
4046389.
2±4.
751.
1±13.
119.
2±15.
53positiveLNs).
Figure3SurvivalcurveforpatientswithstageIIIcolorectalcancer,stratifiedasIIIA,IIIBandIIIC.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page5of7http://www.
wjso.
com/content/10/1/63removed)andthensubdividedeachgroupintotwocat-egories(N1andN2,respectively)(Table5).
OuranalysisconfirmedthatthenumberofpositiveLNsretrieveddir-ectlycorrelatedwiththetotalnumberofLNscollected.
However,whenweusedmultivariateanalysisonthenumberofpositiveLNscollected,alongwithpLNR,tumorstage,andotherfactorssuchasageandgender,thenumberofpositiveLNswasnotfoundtobesignifi-cant(P=0.
35).
OurresultsareconsistentwithananalysisbyMougetal.
[18],whocomparedthenumberofpositiveLNsandthepLNRinbothunivariateandmultivariateanalysis.
pLNRmaintaineditssignificanceasaprognosticfactorinbothmodels,whereasthenumberofpositiveLNswasnotfoundtobesignificantwhencomputedalongotherfactorsinthemultivariatemodel(Tables3,4).
ToovercomeanyfactorsthatcanaffecttheyieldofLNs,weevaluatedaratio-basedclassification,thepositiveLNratio(pLNR).
ThisratiotakesintoaccountboththetotalnumberofLNsretrievedandtheactualnumberofpositiveLNsfound.
Becauseitdoesnotrelyononevariable,thepLNRovercomesseverallimitationspertainingtototalLNcollection,includingsurgicalandpathologicaltechniques,tumorsites,andeventheminimumnumberofLNsthatshouldbedissected[18].
Thismethodhasalreadybeenusedasaprognostictoolforothertumorssuchasgastric,pancreatic,andbreast[12-15].
MultiplecutoffpointsforpLNRhavebeenhavebeenpresentedintheliterature.
Bergeretal.
used0.
4[4].
OurpLNRstratificationusing0.
4asthecutoffpointisconsistentwiththeworkofDeRidderetal.
[20],whousedthesamethreshold.
Asexpected,ourunivariateanalysisshowedthatpatientswithstageIIIAhadabetter10-yearsdisease-freesurvivalrate(75.
8%)thanthosewithstageIIIB(56%)orstageIIIC(nopatientssurvived)(P=0.
01)(Figure2).
ItalsoshowedthatpLNRhadathresholdvalueof0.
4,withpatientshavingbettersurvivalwhentheratiowas≤0.
4(10-yearsurvivalof60.
6%,comparedto0%survivalinpatientswithratio>0.
4)(P702.
4622.
98GenderFemale10.
499-2.
0080.
99810.
39to2.
250.
88Male1.
0010.
93LNR≤0.
411.
472to6.
2340.
00311.
25to22.
120.
02>0.
43.
035.
25StageIIIA10.
318to5.
9560.
66810.
24to5.
630.
86IIIB1.
3770.
836to17.
670.
0841.
150.
21to14.
640.
60IIIC3.
8421.
76PositiveLN1–310.
993to4.
1850.
05210.
12to2.
080.
35≥42.
0390.
51AdjchemoNo10.
279to1.
2350.
1610.
21to1.
270.
15Yes0.
5860.
52Adjchemo,adjuvantchemotherapy;LN,lymphnode;LNR,lymph-noderatio.
Eliasetal.
WorldJournalofSurgicalOncology2012,10:63Page6of7http://www.
wjso.
com/content/10/1/63adjuvantchemotherapy,andpLNR.
StageIII,althoughfoundtobesignificantintheunivariatemodel,lostitspowerwhencomputedalongsidepLNR.
Moreover,pLNR>0.
4provedtohavethemostsignificantprognos-ticfactor(HR=5.
25,CI=1.
2to22.
1,P<0.
05),showingthatpLNRisindeedanindependentprognosticfactorforsurvivalinpatientswithstageIIICRC.
Alimitationofouristhatitwasaretrospectivereviewandtherewassomelossoffollow-upforafewfewpatients.
Nonetheless,theresultsconfirmpreviousstud-iesregardingtheprognosticpoweroftheLNRinthecolorectaldisease.
WehavetonotethatourmanuscriptisthefirstsuchstudytobeconductedintheMiddleEast.
ConclusionOurstudyconfirmstheprognosticvalueoftheratio-basedpLNRmodeltopredicsurvivalofpatientswithstageIIICRCrelativetostage(AJCC),numberofposi-tiveLNs,andtotalLNsretrieved.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authordetails1DivisionofHematologyandOncology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
2DivisionofHepatobiliaryandGastricsurgery,DepartmentofGeneralSurgeryAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
3SchoolofPharmacy,LebaneseAmericanUniversity,Byblos,Lebanon.
4DivisionofGastroenterology,DepartmentofInternalMedicineAmericanUniversityofBeirut,RiadEl-Solh,Beirut11072020,Lebanon.
5DepartmentofInternalMedicine,StatenIslandUniversityHospital,475SeaviewAve,StatenIsland,NY10305,USA.
6MemorialSloan-KetteringCancerCenter,NewYork,NYandWeillMedicalCollegeatCornellUniversity,NewYork,NY.
Authors'contributionsEE,SA,HHandKMdesignedthestudy;EEandHHcollectedthedata;EEdraftedthepaper;SAsupervisedthestudy;andFWandMDeditedandcorrectedthemanuscript.
DH(PhDstatistician)carriedthestatisticalanalysiswiththehelpofMOandCMwhoparticipatedalsoindoingsomepartsoftheanalysis.
Allauthorsreadandapprovedthefinalmanuscript.
Received:9December2011Accepted:25April2012Published:25April2012References1.
JemalA,SiegelR,WardE,etal:Cancerstatistics,2009.
CACancerJClin2009,59:225–249.
2.
EdgeSB,ComptonCC:TheAmericanJointCommitteeonCancer:the7theditionoftheAJCCcancerstagingmanualandthefutureofTNM.
AnnSurgOncol2010,17:1471–1474.
3.
CaplinS,CerottiniJP,BosmanFT,etal:ForpatientswithDukes'B(TNMStageII)colorectalcarcinoma,examinationofsixorfewerlymphnodesisrelatedtopoorprognosis.
Cancer1998,83:666–672.
4.
BergerAC,SigurdsonER,LeVoyerT,etal:Coloncancersurvivalisassociatedwithdecreasingratioofmetastatictoexaminedlymphnodes.
JClinOncol2005,23:8706–8712.
5.
LeVoyerTE,SigurdsonER,HanlonAL,etal:Coloncancersurvivalisassociatedwithincreasingnumberoflymphnodesanalyzed:asecondarysurveyofintergrouptrialINT-0089.
JClinOncol2003,21:2912–2919.
6.
EdlerD,OhrlingK,HallstromM,etal:Thenumberofanalyzedlymphnodes-aprognosticfactorincolorectalcancer.
ActaOncol2007,46:975–981.
7.
SwansonRS,ComptonCC,StewartAK,etal:TheprognosisofT3N0coloncancerisdependentonthenumberoflymphnodesexamined.
AnnSurgOncol2003,10:65–71.
8.
WongSL,JiH,HollenbeckBK,etal:Hospitallymphnodeexaminationratesandsurvivalafterresectionforcoloncancer.
JAMA2007,298:2149–2154.
9.
ChangGJ,Rodriguez-BigasMA,SkibberJM,etal:Lymphnodeevaluationandsurvivalaftercurativeresectionofcoloncancer:systematicreview.
JNatlCancerInst2007,99:433–441.
10.
RoyalCollegeofPathologists:StandardsandDatasetforReportingCancers:Datasetforcolorectalcancer(2ndedition).
Availableat:http://www.
rcpath.
org/resources/pdf/G049-ColorectalDataset-Sep07.
pdf.
Accessedon29,March,2011.
11.
JohnsonPM,PorterGA,RicciardiR,etal:Increasingnegativelymphnodecountisindependentlyassociatedwithimprovedlong-termsurvivalinstageIIIBandIIICcoloncancer.
JClinOncol2006,24:3570–3575.
12.
HatoumHA,JamaliFR,El-SaghirNS,etal:Ratiobetweenpositivelymphnodesandtotalexcisedaxillarylymphnodesasanindependentprognosticfactorforoverallsurvivalinpatientswithnonmetastaticlymphnode-positivebreastcancer.
AnnSurgOncol2009,16:3388–3395.
13.
PawlikTM,GleisnerAL,CameronJL,etal:Prognosticrelevanceoflymphnoderatiofollowingpancreaticoduodenectomyforpancreaticcancer.
Surgery2007,141:610–618.
14.
MarietteC,PiessenG,BriezN,etal:Thenumberofmetastaticlymphnodesandtheratiobetweenmetastaticandexaminedlymphnodesareindependentprognosticfactorsinesophagealcancerregardlessofneoadjuvantchemoradiationorlymphadenectomyextent.
AnnSurg2008,247:365–371.
15.
MarchetA,MocellinS,AmbrosiA,NittiD:ItalianResearchGroupforGastricCancer(IRGGC),etal:Theratiobetweenmetastaticandexaminedlymphnodes(Nratio)isanindependentprognosticfactoringastriccancerregardlessofthetypeoflymphadenectomy:resultsfromanItalianmulticentricstudyin1853patients.
AnnSurg2007,245:543–552.
16.
JosephNE,SigurdsonER,HanlonAL,etal:Accuracyofdeterminingnodalnegativityincolorectalcanceronthebasisofthenumberofnodesretrievedonresection.
AnnSurgOncol2003,10:213–218.
17.
GoldsteinNS,SanfordW,CoffeyM,etal:Lymphnoderecoveryfromcolorectalresectionspecimensremovedforadenocarcinoma.
Trendsovertimeandarecommendationforaminimumnumberoflymphnodestoberecovered.
AmJClinPathol1996,106:209–216.
18.
MougSJ,SaldanhaJD,McGregorJR,etal:Positivelymphnoderetrievalratiooptimisespatientstagingincolorectalcancer.
BrJCancer2009,100:1530–1533.
19.
VatherR,SammourT,KahokehrA,etal:Lymphnodeevaluationandlong-termsurvivalinStageIIandStageIIIcoloncancer:anationalstudy.
AnnSurgOncol2009,16:585–593.
20.
DeRidderM,Vinh-HungV,VanNieuwenhoveY,etal:Prognosticvalueofthelymphnoderatioinnodepositivecoloncancer.
Gut2006,55:1681.
doi:10.
1186/1477-7819-10-63Citethisarticleas:Eliasetal.
:Lymph-noderatioisanindependentprognosticfactorinpatientswithstageIIIcolorectalcancer:aretrospectivestudyfromtheMiddleEast.
WorldJournalofSurgicalOncology201210:63.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitEliasetal.
WorldJournalofSurgicalOncology2012,10:63Page7of7http://www.
wjso.
com/content/10/1/63
- ferentiatedwww.97yes.com相关文档
- 19.9www.97yes.com
- enableswww.97yes.com
- 靛奖www.97yes.com
- tradewww.97yes.com
- 可编程www.97yes.com
- fieldwww.97yes.com
极光KVM美国美国洛杉矶元/极光kvmCN7月促销,美国CN2 GIA大带宽vps,洛杉矶联通CUVIP,14元/月起
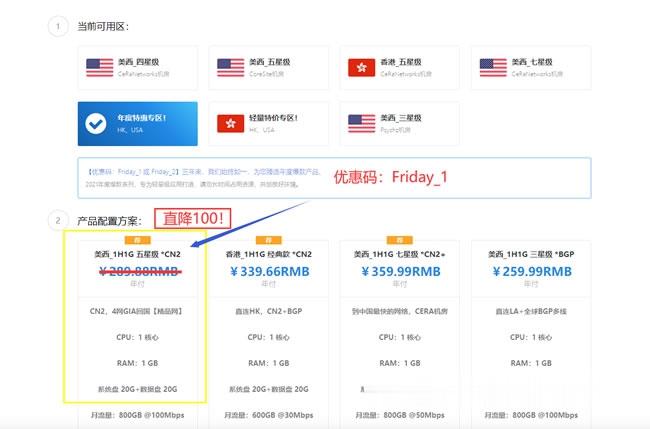
极光KVM怎么样?极光KVM本月主打产品:美西CN2双向,1H1G100M,189/年!在美西CN2资源“一兆难求”的大环境下,CN2+大带宽 是很多用户的福音,也是商家实力的象征。目前,极光KVM在7月份的促销,7月促销,美国CN2 GIA大带宽vps,洛杉矶联通cuvip,14元/月起;香港CN2+BGP仅19元/月起,这次补货,机会,不要错过了。点击进入:极光KVM官方网站地址极光KVM七月...
香港CN2云服务器 1核 2G 35元/月 妮妮云
妮妮云的来历妮妮云是 789 陈总 张总 三方共同投资建立的网站 本着“良心 便宜 稳定”的初衷 为小白用户避免被坑妮妮云的市场定位妮妮云主要代理市场稳定速度的云服务器产品,避免新手购买云服务器的时候众多商家不知道如何选择,妮妮云就帮你选择好了产品,无需承担购买风险,不用担心出现被跑路 被诈骗的情况。妮妮云的售后保证妮妮云退款 通过于合作商的友好协商,云服务器提供2天内全额退款到网站余额,超过2天...
bgpto:日本独立服务器6.5折($120起),新加坡独立服务器7.5折($93起)
bgp.to在对日本东京的独立服务器进行6.5折终身优惠促销,低至$120/月;对新加坡独立服务器进行7.5折终身优惠促销,低至$93/月。所有服务器都是直连国内,速度上面相比欧洲、美国有明显的优势,特别适合建站、远程办公等多种用途。官方网站:https://www.bgp.to/dedicated.html主打日本(东京、大阪)、新加坡、香港(CN)、洛杉矶(US)的服务器业务!日本服务器CPU...
www.97yes.com为你推荐
-
甲骨文不满赔偿未签合同被辞退的赔偿bbs.99nets.com怎么打造完美SFm.2828dy.comwww.dy6868.com这个电影网怎么样?广告法中国的广告法有哪些。www.idanmu.com新开奇迹SF|再创发布网|奇迹SF|奇迹mu|网通奇迹|电信奇迹|菊爆盘请问网上百度贴吧里有些下载地址,他们就直接说菊爆盘,然后后面有字母和数字,比如dk几几几的,www.zzzcn.com哪里有免费看书的网站蚕食嫩妻宠妻一加一老婆难做隐藏的文怎么看两朝太岁‘太岁出土’是什么意思?性间道男人的性癖好有哪四种?