rulewww.163gg.com
www.163gg.com 时间:2021-03-18 阅读:()
REVIEWOpenAccessClinic,neuropathologyandmoleculargeneticsoffrontotemporaldementia:amini-reviewXiao-dongPan1,2,3andXiao-chunChen1,2,3*AbstractFrontotemporallobardegeneration(FTLD)representsagroupofclinically,neuropathologicallyandgeneticallyheterogeneousdisorderswithplentyofoverlapsbetweentheneurodegenerativemechanismandtheclinicalphenotype.
FTLDispathologicallycharacterizedbythefrontalandtemporallobaratrophy.
Frontotemporaldementia(FTD)clinicallypresentswithabnormalitiesofbehaviorandpersonalityandlanguageimpairmentsvariants.
TheclinicalspectrumofFTDencompassesdistinctcanonicalsyndromes:behaviouralvariantofFTD(bvFTD)andprimaryprogressiveaphasia.
Thelaterincludesnonfluent/agrammaticvariantPPA(nfvPPAorPNFA),semanticvariantPPA(svPPAorSD)andlogopenicvariantPPA(lvPPA).
Inaddition,thereisalsooverlapofFTDwithmotorneurondisease(FTD-MNDorFTD-ALS),aswellastheparkinsoniansyndromes,progressivesupranuclearpalsy(PSP)andcorticobasalsyndrome(CBS).
TheFTLDspectrumdisordersarebaseduponthepredominantneuropathologicalproteins(containinginclusionsofhyperphosphorylatedtauorubiquitinprotein,e.
gtransactiveresponse(TAR)DNA-bindingprotein43kDa(TDP-43)andfusedin-sarcomaproteininneuronsandglialcells)intothreemaincategories:(1)microtubule-associatedproteintau(FTLD-Tau);(2)TARDNA-bindingprotein-43(FTLD-TDP);and(3)fusedinsarcomaprotein(FTLD-FUS).
TherearefivemaingenesmutationsleadingclinicalandpathologicalvariantsinFTLDthatidentifiedbymoleculargeneticstudies,whicharechromosome9openreadingframe72(C9ORF72)gene,granulin(GRN)gene,microtubuleassociatedproteintaugene(MAPT),thegeneencodingvalosin-containingprotein(VCP)andthechargedmultivesicularbodyprotein2B(CHMP2B).
Inthisreview,recentadvancesonthedifferentclinicvariants,neuroimaging,genetics,pathologicalsubtypesandclinicopathologicalassociationsofFTDwillbediscussed.
Keywords:bvFTD,Nonfluent/agrammaticvariant,Semanticvariant,Logopenicvariant,Moleculargenetics,MAPT,GRN,C9ORF72IntroductionFrontotemporaldementia(FTD)representsagroupofclinically,neuropathologicallyandgeneticallyhetero-geneousdisorders.
Itisarangeofprogressivedementiasyndromesassociatedwithfocalatrophyoftheorbitomesialfrontalandanteriortemporallobes.
Andthetermfrontotemporallobardegeneration(FTLD)todescribethepathologicalsyndrome.
In1892,ArnoldPickdescribedapatientwithprogressiveaphasiaandlobaratrophy[1].
In1911,AloisAlzheimerdescribedthehistopathologicalstatusrelatedtothesepatients,pointingtheabsenceofsenileplaquesandneuro-fibrillarytangles,andthepresenceofargyrophilicneuronalinclusions(latercalled"Pickbodies")andswollencells(latercalled"Pickcells")atneuropathologicalexamination[2].
However,duringthe20thcentury,thesepatientswithfrontotemporallobardegenerationweregenericallyreferredtoaspatientswithdementia,beingoftendiagnosedwithAlzheimerdisease(AD)[2].
In1994,twomajorresearchgroupsfromLundandManchesterproposedclinicalandneuropathologicalcriteriaforthediagnosisofFTD[3].
In1998,Nearyetal[4]reportedaconsensusonclinicaldiagnosticcriteriaoffrontotemporallobardegenerationintheAmericanAcademyofNeurology(AAN).
FTDoftenbeginswhenthepatientisinthefifthtoseventhdecades.
Epidemiologicalstudiessuggestthat*Correspondence:chenxc998@163.
com1DepartmentofNeurology,UnionHospitalofFujianMedicalUniversity,29XinquanRoad,Fuzhou350001,China2KeyLaboratoryofBrainAgingandNeurodegenerativeDisease;FujianInstituteofGeriatrics,UnionHospitalofFujianMedicalUniversity,29Xinquan,Road,Fuzhou350001,ChinaFulllistofauthorinformationisavailableattheendofthearticleTranslationalNeurodegeneration2013PanandChen;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
PanandChenTranslationalNeurodegeneration2013,2:8http://www.
translationalneurodegeneration.
com/content/2/1/8FTDisthesecondmostcommoncauseofdementiainindividualsyoungerthan65andisjustlesscommonthanAlzheimer'sdisease(AD)withinthisagegroup[2,5].
Ofover65yearsolddementia,theincidenceofFTDranksfourth,thetopthreeisAlzheimer'sdisease,Lewybodydementiaandvasculardementia[5-7].
Theredonotappeartobeanycleargenderdifferencesinsus-ceptibility[8-11].
AmongtheFTDclinicalsyndromes,sexdistributionappearstovaryfromonesubtypetothenext.
SeveralstudiesreportamalepredominanceinbvFTDandSD,andafemalepredominanceinPNFA[5,12].
Thereisawiderangeindurationsofillness(2-20years)partlyreflectingdifferentunderlyingpathologies.
Inthepastfewyears,significantadvanceshavebeenseenintheetiology,pathogenesis,andgenetics,pathologyandclinicalphenotypeofFTD,andmanynewterminologyandclassificationofFTDhaveemerged.
Inthisreview,recentadvancesonthedifferentclinicalvariantphenotypes,neuroimaging,hereditaryforms,pathologicalsubtypesandclinicopathologicalassociationsofFTDwillbediscussed.
FTLDclinicalpresentation:classificationandcharacteristicsFrontotemporallobardegeneration(FTLD)includesagroupofprogressivedegenerativedisorderscharacterisedbyprogressivebehaviouralchange,executivedysfunctionandlanguagedifficulties[13].
UnlikeAD,behavioralsymptomspredominateintheearlystagesofFTLD.
TheclinicalheterogeneityinfamilialandsporadicformsofFTDisremarkable,withpatientsdemonstratingvariablemixturesofdisinhibition,dementia,PSP,CBD,andmotorneurondisease[13,14].
Earlysymptomsaredividedamongcognitive,behavioral,andsometimesmotorabnor-malities,reflectingdegenerationoftheanteriorfrontalandtemporalregions,basalganglia,andmotorneurons[13,14].
FTLDisapowerfulmodeltostudyemotion,socialcognitionandlanguageorganizationinthebrain.
Behavioralvariantfrontotemporaldementia(bvFTD)bvFTDhasthehighestprevalenceamongsttheFTDclinicalsyndromes,accountingforapproximately70%ofallFTDcases[2,5].
TheonsetofbvFTDistypicallybeforetheageof65years,withanaverageonsetageof58years[12,15].
Patientswiththisclinicalvariantpresentwithmarkedchangesinpersonalityandbehaviourandwithrelativepreservationofthecognitivefunctionspraxis,gnosiaandmemory[13,16].
Commonbehavioraldeficitsincludeapathy,disinhibition,weightgain,foodfetishes,compulsions,euphoria,andanabsenceofinsightintotheircondition.
Poorbusinessdecisionsanddifficultyorganizingworktasksarecommon.
Cognitivetestingtypicallyrevealssparedmemorybutimpairedexecutivefunctions[3,13,17].
bvFTDhasbeenassociatedwithsymmetricalventromedialfrontal,orbitalfrontal,andinsularatrophyandleftanteriorcingulateatrophy[18].
BehaviouralassessmentisatthecoreofassessmentinpatientswithpotentialbvFTDandseemstobemoresensitiveindistinguishingbvFTDfromADthanstandardcognitivetesting.
The'InternationalBehavioralVariantFTDCriteriaConsortium'developedinternationalconsensuscriteriaforbvFTD.
Subclassifi-cationsweremadeinpossiblebvFTDdefinedbyclinicalcriteria,probablebvFTDsupportedbyneuroimagingdata,anddefinitebvFTDconfirmationbyneuropathologicalevidenceorapathogenicmutation[17].
Primaryprogressiveaphasia(PPA)PPAisalanguagedisorderthatinvolveschangesintheabilitytospeak,read,writeandunderstandwhatothersaresaying.
Itisassociatedwithearlytemporallobeatrophyorbrainlesionsaroundthelateralfissure.
PPArepresentsaspectrumofselectivelanguagedisordersandthevariantofPPAmightprovidecluestotheunder-lyingpathology[19].
Currentlycerebrospinalfluid(CSF)biomarkershavelimitedabilitytoidentifyPPAreliably,whichmightbeexplainedbythepathologicalheterogeneity.
AnindicationoflowerAβ1-40levelsorthelowerT-tautoAβ1-42ratioinFTD,mightbeusefultodistinguishpatientsfromsubjectsADandcontrolsubjects[20,21].
In2011,criteriawereadoptedfortheclassificationofPPAintothreeclinicalsubtypes:nonfluent/agrammaticvariantPPA(nfvPPAorPNFA),semanticvariantPPA(svPPAorSD)andlogopenicvariantPPA(lvPPA)[22].
TheproposalisanimportantstepforwardinestablishingtheconsistencyofterminologyandclassificationofPPA.
Thediagnosticrecommendationsincludetwosteps.
First,thepatientshouldmeetthebasicstandardofPPA,whichisaninitialpresentationofsignificantdamagetolanguageandaccompaniedbylimiteddailylivingskillsandothercognitiveimpairment.
Second,weneedtoassessthemainlanguagedomains,includingverbalgeneration,repeat,andunderstandingofwordsandsyntax,naming,semanticknowledgeandreading/spellingcharacteristics.
Finally,clinicalvariantswillbedividedbasingonspecificspeechandlanguagefeaturescharacteristicofeachsubtype.
Classificationcanthenbefurtherspecifiedas"imaging-supported"iftheexpectedpatternofatrophyisfoundand"withdefinitepathology"ifpathologicorgeneticdataareavailable.
Therefore,thenewproposalhasaclearpracticalsignificance.
nfvPPAorPNFAisthesecondmostprevalentpres-entationofFTLD,accountingforalarge25%[12].
ThefeatureofnfvPPAincludesgrammaticalerrormakingagrammatismand/orlaboriousspeech,butrelativelypreservedlanguagecomprehension.
Apraxiaofspeech(AOS)ororofacialapraxiaisfrequentlyaccompanyingtheaphasia[15].
SemanticvariantPPA(svPPA)orSDpresentsin20–25%oftheFTLDpatients[12].
svPPAPanandChenTranslationalNeurodegeneration2013,2:8Page2of9http://www.
translationalneurodegeneration.
com/content/2/1/8presentsasignificantlyimpairednamingabilityandwordcomprehension,whilespeechproductionisspared[22,23].
LvPPAorlogopenicprogressiveaphasia[24]ismarkedbyimpairedwordfindinganddifficultrepetition.
lvPPAshowesanimpairedabilitytorepeatsentencesorphrases,spontaneousspeechandasinglewordextractingwhennaming.
UnlikeotherFTDsubtypes,lvPPAgenerallydoesnotproducechangesinbehaviororpersonalityuntillaterstagesofthedisease.
Mostpeoplewithprogressiveaphasiamaintaintheabilitytocareforthemselves,keepupoutsideinterestsand,insomeinstances,remainemployedforafewyearsafteronsetofthedisorder.
LPAismostlyassociatedwithaneuro-pathologicaldiagnosisofAD[25].
ClinicaldistinctionbetweenbvFTD,nfvPPAandsvPPAisoftencomplicatedforthatoverlapoftheclinicalsyndromesbetweenthemcanoccurinadvancedstagesofdisease.
FTLDoverlapswithotherclinicalsyndromeThesubcorticalnucleiandmotorsystemsareinvolvesinFTLDvariants.
Motorneurondysfunction(MND)hasbeendescribedin40%oftheFTLDpatients,referredtoasFTLD-MND.
ThecommoncomorbidityofAmyotrophiclateralsclerosis(ALS)withbehaviorabnormality,cognitiveimpairmentordementiahasbeennoticed[26,27].
FTLDmayprecede,followorcoincidewiththeonsetofmotorsymptoms[28].
OtherdisordersarecloselyrelatedtoFTLD,includingprogressivesupranuclearpalsy(PSP)syndromes,corticobasalsyndrome(CBS),FTDwithparkinsonism(FTDP)andargyrophilicgraindisease(AGD).
PSPandCBSaretwocommonatypicalparkinsoniansyndromesdemonstratingcognitiveandbehaviourdisordersthatoverlapwithFTD.
Ofthem,behavioralandcognitivedysfunctionpromotesthedevelopmentofdementia.
Andextrapyramidalsystemsymptomspresentasbradykinesia,abnormalposture,rigidity,buttremoruncommon.
Theco-occurrenceofAGDinALSisnotuncommon,andcomparablewiththatinanumberofdiseasesbelongingtothetauopathiesorα-synucleinopathies[29].
Motionsystemdamagepresentsasmuscleatrophy.
FTDP-17showinggeneticlinkagetochromosome17,presentswithaclinicalsyn-dromeofautosomaldominantdisinhibition,dementia,parkinsonism,andamyotrophy[30].
TheclinicalpictureresemblesbvFTD,whilecognitivedeficitsincludean-terogradememorydysfunctioninanearlystage,laterthedeteriorationofvisuospatialfunction,orientationandglobalmemoryaregraduallypresented.
Motorsignstypicallyincludethesymmetricalbradykinesiawithoutrestingtremor,incombinationwithaxialrigidityandposturalinstability.
TheearlyclinicalpresentationofAGDissimilartoADbutitislessaggressive,withpatientsmaintainmildcognitiveimpairment(MCI)formanyyears[31].
NeuroimaginginFTLDNeuroimagingplaysacriticalroleindiagnosisofFTD.
NeuroimaginginvestigationscanreliablydifferentiateFTLDsubtypesfromotherdementias,andcanhelpclinicaldiagnosticsbasedonneuropsychiatricsymptoms.
Differentclinicalvariatentshavedifferentformsofbrainatrophy,whichcanbeusedforsomeimportantcluesforearlyclinicaldifferentialdiagnosis.
DTIcandetectwhitematterdamage,differentsubtypesofwhitematterinjuryalsohelpclinicalearlydifferentialdiagnosisofclinicalsubtypesofFTLD[32].
Functionalneuroimagingtechniques,suchas[99mTc]-hexamethylpropyleneamineoximesingle-photonemissioncomputedtomography(SPECT)[33]or[18F]-fluorodeoxyglucose(FDG)-PETareincreasinglybeingusedtohelpwiththediagnosisofFTLD[34].
Arterialspinlabelingimaging(ASL)likeFDG-PETcanbeusedforshowingthehypometabolisminbrainregions.
HypometabolismonFDG-PETisdetectedconsistentlyandreliablyinfrontalbrainregionsinpatientswithbvFTDcomparedwiththosewithAD,whoshowposteriorcingulatehypometabolismearlyinthediseaseprocess[34].
However,inpatientsshowingclearbrainatrophyonstructuralMRI,littleadditionaldiagnosticbenefitisgainedbydoingaPETscan,becausefocalatrophyisapositivepredictivemarkerofFTD.
Theimagingpresen-tationofnfvPPAindicatesthatpredominantleftposteriorfronto-insularatrophyonMRIorpredominantleftposteriorfronto-insularhypoperfusionorhypometabolismonSPECTorPET.
Imaging-supportedsvPPAshowpredominantanteriortemporallobeatrophyand/orthesebrainregionshypoperfusionorhypometabolismonSPECTorPET.
TheimagingoflvPPAmustshowatleastoneofpredominantleftposteriorperisylvianorparietalatrophyonMRIand/orhypoperfusionorhypometabolismonSPECTorPET[22,25,35-37].
FutureinFTLDareverysimilartoimaginginAD–earlydetection,moleculardiagnosis,monitordiseaseprogressionandvalidateandimplementdiseasemodifyingtherapies.
SpecificanatomicpatternsinFTLD,andanamyloid-PETneuroimaging,whichusestheamyloid-β-detecting11C-PittsburghcompoundB,hasshownpromisingresultsindiscriminatingorrule-outatypicalADandFTDcases[38,39]particularlythosepresentingwithlanguagedeficitsratherthanbehaviouralchanges.
MicroPETwith18F-THK523inTautransgenicmicehavebeenreported[40].
Tauspecificimagingscannerthatusesthe18F-THK523maybeapromisingtechniquecomingsooninfuture[40].
FTLDNeuropathologyandcliniconeuropathologicalcorrelationsNeuropathologyThesubtypesofunderlyingpathologicalchangesinpatientswithFTDareclassifiedonthebasisofthePanandChenTranslationalNeurodegeneration2013,2:8Page3of9http://www.
translationalneurodegeneration.
com/content/2/1/8patternofproteindeposition,andarereferredtocollectivelyasfrontotemporallobardegeneration.
Underamicroscope,commonpathologicchangesofFTLDareatrophybrainregionpresentingneuronalloss,spongychangeandgliosisincorticesofatrophiedfrontalandtemporallobes[41,42].
FTDhaveidentifiednovelgeneticdefectsandachromosomallocusinhereditaryformsofFTLD,aswellasnovelclinicneuropathologicalassociations.
Immunohistochemistryallowssubcategorizationofthesedisordersintospecificproteinopathiesbasedonthemajorconstituentoftheinclusions.
(1)FTLD-tau:Onesubtypeispresentedasneuronsandglialcellscontaininginclusionsofhyperphosphorylatedtauprotein,referredtoasFTLD-tau[43].
TaupathologywasassociatedwithFTDwithparkinsonism,PSPsyndromes[44],CBS[45]andAGD[31].
(2)FTLD-UbiquitinorFTLD-U:Over50%oftheFTLDpatientspresentedwithtau-negativeubiquitinstaininginclusions,referredtoasFTLD-UbiquitinorFTLD-U[46].
In80–95%ofthisgroup,inclusionswerefoundtobecomposedoftransactiveresponse(TAR)DNA-bindingprotein43kDa(TDP-43)[47-49],referredtoasFTLD-TDP[50],orTDP-43-negativeFTLD-Ucaseshavinginclusionsoffusedin-sarcomaprotein(FUS),referredtoasFTLD-FUS[43,49,51,52].
However,inasmallnumberofFTLD-Upatients,theinclusionproteinremainsunclear.
ThisgroupisreferredtoasFTLD-ubiquitinproteasomesystem(FTLD-UPS)[46,53].
(3)Dementialackingdistinctivehistopathology(DLDH)[54,55].
(4)Otherraretypes:dementiawithbasophilicinclusionbody,neuronalintermediatefilamentinclusiondisease[52].
AssociationbetweenpathologyandclinicalphenotypeAssociationswerenotedbetweentheclinicalFTLDsubtypesandunderlyingproteinopathies,butastrictonetoonerelationshipislacking.
bvFTDismostlyassociatedwithFTLD-TDP43,somecasesarealsocorrelatedwithFTLD-tau(PiDsubtype).
AnFTLD-FUSproteinopathyisinvariantlyassociatedwithaclinicaldiagnosisofbvFTD,eitherwithorwithoutthesignsofMND.
MicroscopicassessmentofnfaPPAatautopsyoftenrevealsFTLDasso-ciatedwithatauopathy(FTLD-tau).
nfaPPAiscommonlyassociatedwithtaupathology,especiallywhenAOSororofacialapraxiaispresent.
Inmostcases,thepathologyunderlyingnfaPPAwasmixed,includingFTLD-tauandFTLD-TDP43,butwithapredominanceofFTLD-taupathology.
SvPPAis,inmostcases,linkedwithTDP-43-immunoreactivepathology,althoughtaupathologyissometimesobserved.
Somepatientswithpredominantlyrighttemporallobeatrophy(RTLA)areusuallydiagnosedclinicallywitheitherbvFTDorsvPPA[56].
IthasbeensuggestedthatpatientswithbvFTDandRTLAhaveFTLD-taupathology,whereaspatientswithsvPPAandRTLAhaveFTLD-TDP43pathology[56].
svPPApatientswhooftenpresentwithacalculiaisassociatedwithFTLD-tau[57].
LvPAispredominantlyassociatedwithADpathology.
ManypatientswithlvPPAoftenhaveunderlyingADpathology[58-60].
CSFtau:amyloid-βratio[37]andPiBPETimaging[25]studiescanbehelpfulintheidentificationofpatientswhoaremorelikelytohavelvPPAthannfaPPA.
Arecentstudyshowedthat93%ofpatientswithlvPPAonamyloidPETimagingwasfoundPiBpositive,butsvPPAonly9%,nfvPPAis13%,whichsuggeststhatthereissomecommonpathologicalfeaturesbetweenlvPPAandAD[59].
TaupathologywasalsoassociatedwithFTLDwithparkinsonism,PSP,CBD,AGDandPickbodies(PiD)[30,44,61].
Similarly,TDP-43andFUSproteinopathiesarealsocommonlyfoundinMNDwithorwithoutFTLD[52].
Althoughthesearerelativelystrongassociations,theyarenotabsolute,anditiscurrentlynotpossibletopredictwithcertaintytheunderlyingpathologyofspecificFTLDsyndromes.
ExtrapyramidalsystemsymptomsaccompaniedwithapraxiaindicatesthepresenceofCBS,whichmostlyattributestoTaudisease.
WhiledementiawithFTLD-MNDsyndromemostlyattributestoTDP-43pathology[15,45,57].
ThesesuggestthatitiscontributingtotherapeuticstrategyforFTLDthroughelucidatingtherelationshipbetweenpathologicalandclinicalpresentation.
MoleculargeneticsApproximately40%ofpatientswithFTDhaveafamilyhistory[8].
bvFTDisthemostprominentsubtypewithfamilyhistory,especiallywhenconcomitantsymptomsofMNDarepresent(60%),whileSvPPAappearedtobetheleasthereditaryFTLDsubtype(<20%)[62].
Moleculargen-eticstudieshaveidentifiedseveralcommon(MAPT,GRN)andrare(VCP,CHMP2B,TARDBP,FUS)geneticfactorsinhereditaryFTLDoverrecentyears.
In1998microtubuleassociatedproteintau(MAPT)genewasfound,whichlocatedonchromosome17q21.
32,inwhich13%ofthecasesisFTDP-17,thosewhohaveparkinson-likesymptoms[63].
In2004,thegeneencodingvalosin-containingprotein(VCP)genewasfound,locatedonchromosome9p13.
3,whichisassociatedwiththegenesthatcauseFTLDinasso-ciationwithinclusionbodymyopathyandPaget'sdisease[64,65].
In2005,thechargedmultivesicularbodyprotein2B(CHMP2B,alsoknownaschromatin-modifyingprotein2B)genemutations,locatedonchromosome3p11.
2,wasdiscoveredinalargeDanishcohortwithfamilialFTLD[66,67].
In2006,amutatedgenelocatedonchromosomePanandChenTranslationalNeurodegeneration2013,2:8Page4of9http://www.
translationalneurodegeneration.
com/content/2/1/8Table1Clinicalphenotypes,pathologicalandmoleculargeneticspectruminFTLD[13,19,22,35,72,77,78]CoreclinicalfeaturePraxiologicalobstacleLogopathyExtrapyramidalsymptoms+praxiologicalobstacleDyskinesia+praxiologicalobstacleClinicalsyndromeBehavioralvariantFrontotemporaldementia(bvFTD)Primaryprogressiveaphasia(PPA)Corticobasaldegeneration(CBD)progressivesupranuclearpalsy(PSP)FTD-MND/ALSnonfluent/agrammaticvariantPPA(nfvPPA)Semanticsvariation(svPPA)logopenicvariantPPA(lvPPA)BrainmorphologicallyaffectedpartsPrefrontallobeandtemporallobeLeftposteriorfrontallobe,insulaThefront/ventraltemporallobeleftposteriorsuperiortemporallobeandmedialparietallobeFrontalandtemporallobe,BasalgangliaBasalgangliaandbrainstemCortexandmotorneuronBiochemistryandNeuropathologyFTLD-Tau(Picktype,3R-tau)FTLD-TDP43FTLD-TaumorethanFTLD-TDP43,ADlikepathologicalvisibleMostbelongstoFTLD-TDP43;ADlikepathologicalrareAD-likepathologicalcommon;FTLD-TDP43visibleFTLD-Tau(CBDtype,4R-tau)commonFTLD-Tau(PSPtype,4R-tau)commonFTLD-TDP43,FTLD-FUSCausativeandAssociatedGenesC9ORF72PGRN,C9ORF72PGRNMAPTC9ORF72PGRNC9ORF72PGRNMAPTPGRNFUSMAPTMAPTMAPTPGRNC9ORF72C9ORF72VCPVCPVCPVCPVCPVCPCHMP2BCHMP2BCHMP2BCHMP2BCHMP2BNote:3Rtau:threemicrotubulebindingrepeats;4Rtau:fourmicrotubule-bindingrepeats.
PanandChenTranslationalNeurodegeneration2013,2:8Page5of9http://www.
translationalneurodegeneration.
com/content/2/1/817q21.
31areidentifiedasthegranuleproteinprecursor(PGRN),only1.
7MnucleotideawayfromtheMAPT[68,69].
Approximately10%ofpatientswithFTLDisassociatedwiththisgene.
In2011,chromosome9openreadingframe72(C9ORF72)genewasnewlyidentifiedinFTLD[70,71].
Overall,patientswithmutationsinGRN,MAPTandC9ORF72togetheraccountforatleast17%oftotalFTDcases[53,72].
SummedC9ORF72,GRNandMAPTmutationfrequencieswere32-40%[70,73].
MutationsinVCPandCHMP2Barerare,eachexplaininglessthan1%ofthefamilialFTLD.
TheMAPTgenemutationsoftenleadtoFTLD-Taupathologicalchanges.
TheBothPGRNandC9ORF72muta-tionscancauseFTLD-TDP-43.
ThesymmetryfrontallobeatrophyinbvFTDpatientsisassociatedwithC9ORF72andMAPTgenemutations,whereastheasymmetryoffrontallobeatrophyinbvFTDpatientsisassociatedwithPGRNgenemutations[74].
Thelargehexanucleotiderepeatexpansionlocatedwithinthenon-codingportionofC9ORF72isthecauseofchromosome9-linkedALSandFTLD[70].
Thesesuggestthatspecificgenemutationsmayaffectthepatternsofneuroanatomicinjuryinthedevelopmentoffrontallobaratrophy.
C9ORF72isexpressedasthreemajortranscriptsandtheexpandedG4C2repeatislocatedintheproximalregulatoryregionofC9ORF72[70,73],upstreamofoneandinthefirstintronofthetwoothertranscripts.
Repeatexpansionresultsinnearcompletelossofexpressionofthemajorgenetranscripts.
Thepathogenicexpansionwasnon-penetrantinindividualsyoungerthan35years,50%penetrantby58years,andalmostfullypenetrantby80years.
Innormalpopulation,thesizeoftheG4C2repeatrangesfrom3to25units,whichisexpandedtoatleast60unitsinFTLDpatients[70,71,73].
TheclinicalphenotypeofC9ORF72mutationoftenpresentsasbvFTDorALSorFTDco-morbiditiesALS.
InpatientswithbvFTD,C9ORF72mutationismorecommonthanMAPTorPGRN.
Anxietyoragitation,andmemorydysfunction(oftenepisodicmemory)isacommonclinicalfeature.
Thosecasesunderlinesthatthehexanucleotiderepeatexpansioninchromosome9couldbealsoassociatedwithearlyonsetpsychiatricpresentations[75].
Overexpressedp-62inclusionbodylesionsinthecere-bellumisoneofpathologicalfeatures[76].
Neuroimagingpresentsasthesymmetricalfrontaland/ortemporallobeatrophy,andparietal,occipitalandcerebellaratrophycanalsoappear.
Therefore,C9ORF72mutationisnotonlyas-sociatedwithcorticalanatomicsitebutalsowithsub-corticalstructures.
However,itisunclearfortheexactmechanismofactionofthis"repeatamplificationC9ORF72gene".
TheclinicalandpathologicalheterogeneityinFTLDcausesachallengefordiagnosisofFTLD.
AhelpfulTable2TheprofileofmaingenesmutationanditspossiblediseasemechanismsinFTLDGenesymbolMAPTC9ORF72PGRNVCPCHMP2BFullnameMicrotubule-associatedproteintauChromosome9openreadingframe72ProgranulinValosincontainingproteinChromatinmodifyingprotein2BChromosomallocalization17q21.
329p21.
217q21.
329p13.
33p11.
2.
MAPTgivesrisetosixisoforms:threeisoformscontainingthreeamino-acidrepeats(3R),andthreeisoformswithfourrepeats(4R)[79].
expressedasthreemajortranscripts,theexpandedG4C2repeatislocatedintheproximalregulatoryregionofC9ORF72[70,73].
encodesprogranulin,aubiquitouslyexpressedgrowthfactorprecursorconsistingof7.
5granulinpeptides.
EncodesaubiquitouslyexpressedmemberofafamilyofATPasesassociatedwithawiderangeofcellularfunctions[85].
EncodesacomponentoftheheteromericESCRT-IIIcomplexwithfunctionsintheendosomal-lysosomalandtheautophagicproteindegradationpathway.
FunctionsandpossibleroleinthediseasemechanismMutationsresultinachangeinratioof3Rto4Rtauisoforms.
Mutationsaffectthenormalfunctionofthetauproteintostabilisemicrotubules,increasethetendencyoftautoformneurotoxicaggregatesanddisturbneuronalplasticityandaxonaltransport[80].
Repeatexpansionresultsinnearcompletelossofthemajorgenetranscripts.
AndaccumulationoftranscriptsharboringtheexpandedG4C2repeatinnuclearRNAfoci[70].
awiderangeofbiologicalprocessessuchasinflammationandwoundrepair,orinpathologicalconditionsincludingtumorigenesis[82].
mutationsresideattheinterfacebetweentheD1ATPaseandtheN-domainoftheCDC48-likeprotein[85].
Expressedinneuronsofallmajorbrainregions.
Itiscriticalfordevelopment,sexualdifferentiation[88]andneuronalsurvival[89].
G4C2repeatleadstoneuronalcytoplasmicinclusionsthroughouttheentirecorticalthickness[81].
Neurotrophicfunctioninvolvedinneuronalsurvivalandneuriteoutgrowth[83,84].
mutationsdisturbubiquitin-proteasomemediatedproteindegradation,autophagy,orboth[86,87].
MutationsaffecttheC-terminalendoftheproteinduetoaberrantsplicing[78].
unidentifiedmechanismsexist.
Estimatedmutationfrequency[69,72,79,81,90]0-50%14-48%3–26%<1%<1%PanandChenTranslationalNeurodegeneration2013,2:8Page6of9http://www.
translationalneurodegeneration.
com/content/2/1/8supplementforclinicalevaluationusinggeneticsandbiologicalmarkerstestingcansignificantlyimprovetheforecastofpotentialhistopathologyinvivo.
Wesummarizeclinicalphenotypes,molecularpathologicalandgeneticspectruminFTLDinTable1.
Andtheprofileofmaingenesmutationsanditspossiblediseasemecha-nismsinFTLDisshowninTable2.
ConclusionInthisreview,wehavesystematicallyupdatedcurrentunderstandingonclinical,genetic,neuropathological,andneuroimagingperspectivesofFTD.
ThisreviewaimstoarouseawarenessofFTDamongclinicians,inpar-ticularwhentheoverlappingclinicalandneuroimagingcharacteristicfeaturesamongdementiaanddifferentsubtypesofFTDremaingreatchallengesforclinicians.
IdentificationofbiomarkersforclinicaldiagnosisanddifferentiationFTDfromotherdementiaiswarrantedforfuturestudies.
Genediagnosistestshouldbecon-sideredforfamilialcasessuspectedwithFTDinclinicpractice.
Longitudinalclinicopathologicalcorrelationstudieswillfurtherelucidatethenetworkfunctionsofhumanbraininthiscomplexdisorderwithbehaviour,speechandmotorabnormality.
Withfurtherunder-standingofthegenetics,clinicalandneuropathologicalbasisofFTD,wecanvisualisethatFTDwillbefurtherclinicallydefined.
Andnewconsensuswillbedevelopedforbetterguidanceinclinicalpractice.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authors'contributionsXdPcollectedthereferencematerialsanddraftedthemanuscript.
XcCrevisedthemanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
AcknowledgementsThisworkwassupportedbythegrantsfromtheNationalNaturalScienceFoundationofChina(81200991),OutstandingYoungPersons'ResearchProgramforHigherEducationofFujianProvince,China(JA10123),MajorProjectofFujianScienceandTechnologyBureau(2009D061).
Authordetails1DepartmentofNeurology,UnionHospitalofFujianMedicalUniversity,29XinquanRoad,Fuzhou350001,China.
2KeyLaboratoryofBrainAgingandNeurodegenerativeDisease;FujianInstituteofGeriatrics,UnionHospitalofFujianMedicalUniversity,29Xinquan,Road,Fuzhou350001,China.
3CentreofNeurobiology,FujianMedicalUniversity,88JiaotongRoad,Fuzhou350001,China.
Received:29December2012Accepted:8April2013Published:19April2013References1.
RossorMN:Pick'sdisease:aclinicaloverview.
Neurology2001,56:S3–S5.
2.
SnowdenJS,NearyD,MannDM:Frontotemporaldementia.
BrJPsychiatry2002,180:140–143.
3.
TheLundandManchesterGroups:Clinicalandneuropathologicalcriteriaforfrontotemporaldementia.
JNeurolNeurosurgPsychiatry1994,57:416–418.
4.
NearyD,SnowdenJS,GustafsonL,PassantU,StussD,BlackS,FreedmanM,KerteszA,RobertPH,AlbertM,etal:Frontotemporallobardegeneration:aconsensusonclinicaldiagnosticcriteria.
Neurology1998,51:1546–1554.
5.
RatnavalliE,BrayneC,DawsonK,HodgesJR:Theprevalenceoffrontotemporaldementia.
Neurology2002,58:1615–1621.
6.
ArvanitakisZ:Updateonfrontotemporaldementia.
Neurologist2010,16:16–22.
7.
BarkerWW,LuisCA,KashubaA,LuisM,HarwoodDG,LoewensteinD,WatersC,JimisonP,ShepherdE,SevushS,etal:RelativefrequenciesofAlzheimerdisease,Lewybody,vascularandfrontotemporaldementia,andhippocampalsclerosisintheStateofFloridaBrainBank.
AlzheimerDisAssocDisord2002,16:203–212.
8.
RossoSM,DonkerKaatL,BaksT,JoosseM,deKoningI,PijnenburgY,deJongD,DooijesD,KamphorstW,RavidR,etal:FrontotemporaldementiainTheNetherlands:patientcharacteristicsandprevalenceestimatesfromapopulation-basedstudy.
Brain2003,126:2016–2022.
9.
MercyL,HodgesJR,DawsonK,BarkerRA,BrayneC:Incidenceofearly-onsetdementiasinCambridgeshire,UnitedKingdom.
Neurology2008,71:1496–1499.
10.
IkedaM,IshikawaT,TanabeH:Epidemiologyoffrontotemporallobardegeneration.
DementGeriatrCognDisord2004,17:265–268.
11.
HouCE,YaffeK,Perez-StableEJ,MillerBL:Frequencyofdementiaetiologiesinfourethnicgroups.
DementGeriatrCognDisord2006,22:42–47.
12.
JohnsonJK,DiehlJ,MendezMF,NeuhausJ,ShapiraJS,FormanM,ChuteDJ,RobersonED,Pace-SavitskyC,NeumannM,etal:Frontotemporallobardegeneration:demographiccharacteristicsof353patients.
ArchNeurol2005,62:925–930.
13.
PiguetO,HornbergerM,MioshiE,HodgesJR:Behavioural-variantfrontotemporaldementia:diagnosis,clinicalstaging,andmanagement.
LancetNeurol2011,10:162–172.
14.
LilloP,GarcinB,HornbergerM,BakTH,HodgesJR:Neurobehavioralfeaturesinfrontotemporaldementiawithamyotrophiclateralsclerosis.
ArchNeurol2010,67:826–830.
15.
JosephsKA,HodgesJR,SnowdenJS,MackenzieIR,NeumannM,MannDM,DicksonDW:Neuropathologicalbackgroundofphenotypicalvariabilityinfrontotemporaldementia.
ActaNeuropathol2011,122:137–153.
16.
BathgateD,SnowdenJS,VarmaA,BlackshawA,NearyD:Behaviourinfrontotemporaldementia,Alzheimer'sdiseaseandvasculardementia.
ActaNeurolScand2001,103:367–378.
17.
RascovskyK,HodgesJR,KnopmanD,MendezMF,KramerJH,NeuhausJ,vanSwietenJC,SeelaarH,DopperEG,OnyikeCU,etal:Sensitivityofreviseddiagnosticcriteriaforthebehaviouralvariantoffrontotemporaldementia.
Brain2011,134:2456–2477.
18.
RohrerJD,LashleyT,SchottJM,WarrenJE,MeadS,IsaacsAM,BeckJ,HardyJ,deSilvaR,WarringtonE,etal:Clinicalandneuroanatomicalsignaturesoftissuepathologyinfrontotemporallobardegeneration.
Brain2011,134:2565–2581.
19.
GrossmanM:Primaryprogressiveaphasia:clinicopathologicalcorrelations.
NatRevNeurol2010,6:88–97.
20.
IrwinDJ,McMillanCT,ToledoJB,ArnoldSE,ShawLM,WangLS,VanDeerlinV,LeeVM,TrojanowskiJQ,GrossmanM:ComparisonofcerebrospinalfluidlevelsoftauandAbeta1-42inAlzheimerdiseaseandfrontotemporaldegenerationusing2analyticalplatforms.
ArchNeurol2012,69:1018–1025.
21.
VerweyNA,KesterMI,vanderFlierWM,VeerhuisR,BerkhofH,TwaalfhovenH,BlankensteinMA,ScheltensAP,PijnenburgYA:AdditionalvalueofCSFamyloid-beta40levelsinthedifferentiationbetweenFTLDandcontrolsubjects.
JAlzheimersDis2010,20:445–452.
22.
Gorno-TempiniML,HillisAE,WeintraubS,KerteszA,MendezM,CappaSF,OgarJM,RohrerJD,BlackS,BoeveBF,etal:Classificationofprimaryprogressiveaphasiaanditsvariants.
Neurology2011,76:1006–1014.
23.
SnowdenJS,ThompsonJC,StopfordCL,RichardsonAM,GerhardA,NearyD,MannDM:Theclinicaldiagnosisofearly-onsetdementias:diagnosticaccuracyandclinicopathologicalrelationships.
Brain2011,134:2478–2492.
24.
Gorno-TempiniML,BrambatiSM,GinexV,OgarJ,DronkersNF,MarconeA,PeraniD,GaribottoV,CappaSF,MillerBL:Thelogopenic/phonologicalvariantofprimaryprogressiveaphasia.
Neurology2008,71:1227–1234.
25.
RabinoviciGD,JagustWJ,FurstAJ,OgarJM,RacineCA,MorminoEC,O'NeilJP,LalRA,DronkersNF,MillerBL,etal:Abetaamyloidandglucosemetabolisminthreevariantsofprimaryprogressiveaphasia.
AnnNeurol2008,64:388–401.
26.
PhukanJ,PenderNP,HardimanO:Cognitiveimpairmentinamyotrophiclateralsclerosis.
LancetNeurol2007,6:994–1003.
27.
RingholzGM,AppelSH,BradshawM,CookeNA,MosnikDM,SchulzPE:PrevalenceandpatternsofcognitiveimpairmentinsporadicALS.
Neurology2005,65:586–590.
PanandChenTranslationalNeurodegeneration2013,2:8Page7of9http://www.
translationalneurodegeneration.
com/content/2/1/828.
vanLangenhoveT,vanderZeeJ,vanBroeckhovenC:Themolecularbasisofthefrontotemporallobardegeneration-amyotrophiclateralsclerosisspectrum.
AnnMed2012,44:817–828.
29.
SomaK,FuYJ,WakabayashiK,OnoderaO,KakitaA,TakahashiH:Co-occurrenceofargyrophilicgraindiseaseinsporadicamyotrophiclateralsclerosis.
NeuropatholApplNeurobiol2012,38:54–60.
30.
SpillantiniMG,BirdTD,GhettiB:FrontotemporaldementiaandParkinsonismlinkedtochromosome17:anewgroupoftauopathies.
BrainPathol1998,8:387–402.
31.
FerrerI,SantpereG,vanLeeuwenFW:Argyrophilicgraindisease.
Brain2008,131:1416–1432.
32.
ZhangY,SchuffN,DuAT,RosenHJ,KramerJH,Gorno-TempiniML,MillerBL,WeinerMW:WhitematterdamageinfrontotemporaldementiaandAlzheimer'sdiseasemeasuredbydiffusionMRI.
Brain2009,132:2579–2592.
33.
VarmaAR,AdamsW,LloydJJ,CarsonKJ,SnowdenJS,TestaHJ,JacksonA,NearyD:DiagnosticpatternsofregionalatrophyonMRIandregionalcerebralbloodflowchangeonSPECTinyoungonsetpatientswithAlzheimer'sdisease,frontotemporaldementiaandvasculardementia.
ActaNeurolScand2002,105:261–269.
34.
KandaT,IshiiK,UemuraT,MiyamotoN,YoshikawaT,KonoAK,MoriE:ComparisonofgreymatterandmetabolicreductionsinfrontotemporaldementiausingFDG-PETandvoxel-basedmorphometricMRstudies.
EurJNuclMedMolImaging2008,35:2227–2234.
35.
GrossmanM:Thenon-fluent/agrammaticvariantofprimaryprogressiveaphasia.
LancetNeurol2012,11:545–555.
36.
GrossmanM,PowersJ,AshS,McMillanC,BurkholderL,IrwinD,TrojanowskiJQ:Disruptionoflarge-scaleneuralnetworksinnon-fluent/agrammaticvariantprimaryprogressiveaphasiaassociatedwithfrontotemporaldegenerationpathology.
BrainLang2012.
inPress,doi:10.
1016/j.
bandl.
2012.
10.
005.
[Epubaheadofprint],PMID:23218686.
37.
HuWT,McMillanC,LibonD,LeightS,FormanM,LeeVM,TrojanowskiJQ,GrossmanM:MultimodalpredictorsforAlzheimerdiseaseinnonfluentprimaryprogressiveaphasia.
Neurology2010,75:595–602.
38.
EnglerH,SantilloAF,WangSX,LindauM,SavitchevaI,NordbergA,LannfeltL,LangstromB,KilanderL:InvivoamyloidimagingwithPETinfrontotemporaldementia.
EurJNuclMedMolImaging2008,35:100–106.
39.
RoweCC,NgS,AckermannU,GongSJ,PikeK,SavageG,CowieTF,DickinsonKL,MaruffP,DarbyD,etal:Imagingbeta-amyloidburdeninaginganddementia.
Neurology2007,68:1718–1725.
40.
Fodero-TavolettiMT,OkamuraN,FurumotoS,MulliganRS,ConnorAR,McLeanCA,CaoD,RigopoulosA,CartwrightGA,O'KeefeG,etal:18F-THK523:anovelinvivotauimagingligandforAlzheimer'sdisease.
Brain2011,134:1089–1100.
41.
BroeM,HodgesJR,SchofieldE,ShepherdCE,KrilJJ,HallidayGM:Stagingdiseaseseverityinpathologicallyconfirmedcasesoffrontotemporaldementia.
Neurology2003,60:1005–1011.
42.
KersaitisC,HallidayGM,KrilJJ:Regionalandcellularpathologyinfrontotemporaldementia:relationshiptostageofdiseaseincaseswithandwithoutPickbodies.
ActaNeuropathol2004,108:515–523.
43.
MackenzieIR,RademakersR,NeumannM:TDP-43andFUSinamyotrophiclateralsclerosisandfrontotemporaldementia.
LancetNeurol2010,9:995–1007.
44.
HoglingerGU,MelhemNM,DicksonDW,SleimanPM,WangLS,KleiL,RademakersR,deSilvaR,LitvanI,RileyDE,etal:Identificationofcommonvariantsinfluencingriskofthetauopathyprogressivesupranuclearpalsy.
NatGenet2011,43:699–705.
45.
BoeveBF:Themultiplephenotypesofcorticobasalsyndromeandcorticobasaldegeneration:implicationsforfurtherstudy.
JMolNeurosci2011,45:350–353.
46.
MackenzieIR,NeumannM,BigioEH,CairnsNJ,AlafuzoffI,KrilJ,KovacsGG,GhettiB,HallidayG,HolmIE,etal:Nomenclatureforneuropathologicsubtypesoffrontotemporallobardegeneration:consensusrecommendations.
ActaNeuropathol2009,117:15–18.
47.
BenajibaL,LeBerI,CamuzatA,LacosteM,Thomas-AnterionC,CouratierP,LegallicS,SalachasF,HannequinD,DecoususM,etal:TARDBPmutationsinmotoneurondiseasewithfrontotemporallobardegeneration.
AnnNeurol2009,65:470–473.
48.
NeumannM,SampathuDM,KwongLK,TruaxAC,MicsenyiMC,ChouTT,BruceJ,SchuckT,GrossmanM,ClarkCM,etal:UbiquitinatedTDP-43infrontotemporallobardegenerationandamyotrophiclateralsclerosis.
Science2006,314:130–133.
49.
MackenzieIR,FotiD,WoulfeJ,HurwitzTA:Atypicalfrontotemporallobardegenerationwithubiquitin-positive,TDP-43-negativeneuronalinclusions.
Brain2008,131:1282–1293.
50.
GrossmanM,WoodEM,MooreP,NeumannM,KwongL,FormanMS,ClarkCM,McCluskeyLF,MillerBL,LeeVM,etal:TDP-43pathologiclesionsandclinicalphenotypeinfrontotemporallobardegenerationwithubiquitin-positiveinclusions.
ArchNeurol2007,64:1449–1454.
51.
MackenzieIR,MunozDG,KusakaH,YokotaO,IshiharaK,RoeberS,KretzschmarHA,CairnsNJ,NeumannM:DistinctpathologicalsubtypesofFTLD-FUS.
ActaNeuropathol2011,121:207–218.
52.
RoeberS,MackenzieIR,KretzschmarHA,NeumannM:TDP-43-negativeFTLD-Uisasignificantnewclinico-pathologicalsubtypeofFTLD.
ActaNeuropathol2008,116:147–157.
53.
RohrerJD,GuerreiroR,VandrovcovaJ,UphillJ,ReimanD,BeckJ,IsaacsAM,AuthierA,FerrariR,FoxNC,etal:Theheritabilityandgeneticsoffrontotemporallobardegeneration.
Neurology2009,73:1451–1456.
54.
GiannakopoulosP,HofPR,BourasC:Dementialackingdistinctivehistopathology:clinicopathologicalevaluationof32cases.
ActaNeuropathol1995,89:346–355.
55.
JosephsKA,JonesAG,DicksonDW:Hippocampalsclerosisandubiquitin-positiveinclusionsindementialackingdistinctivehistopathology.
DementGeriatrCognDisord2004,17:342–345.
56.
GainottiG:Differentpatternsoffamouspeoplerecognitiondisordersinpatientswithrightandleftanteriortemporallesions:asystematicreview.
Neuropsychologia2007,45:1591–1607.
57.
RabinoviciGD,MillerBL:Frontotemporallobardegeneration:epidemiology,pathophysiology,diagnosisandmanagement.
CNSDrugs2010,24:375–398.
58.
JosephsKA,WhitwellJL,DuffyJR,VanvoorstWA,StrandEA,HuWT,BoeveBF,Graff-RadfordNR,ParisiJE,KnopmanDS,etal:ProgressiveaphasiasecondarytoAlzheimerdiseasevsFTLDpathology.
Neurology2008,70:25–34.
59.
MesulamM,WicklundA,JohnsonN,RogalskiE,LegerGC,RademakerA,WeintraubS,BigioEH:Alzheimerandfrontotemporalpathologyinsubsetsofprimaryprogressiveaphasia.
AnnNeurol2008,63:709–719.
60.
RohrerJD,RossorMN,WarrenJD:Alzheimer'spathologyinprimaryprogressiveaphasia.
NeurobiolAging2012,33:744–752.
61.
NearyD,SnowdenJ,MannD:Frontotemporaldementia.
LancetNeurol2005,4:771–780.
62.
GoldmanJS,FarmerJM,WoodEM,JohnsonJK,BoxerA,NeuhausJ,Lomen-HoerthC,WilhelmsenKC,LeeVM,GrossmanM,etal:ComparisonoffamilyhistoriesinFTLDsubtypesandrelatedtauopathies.
Neurology2005,65:1817–1819.
63.
HuttonM,LendonCL,RizzuP,BakerM,FroelichS,HouldenH,Pickering-BrownS,ChakravertyS,IsaacsA,GroverA,etal:Associationofmissenseand50-splice-sitemutationsintauwiththeinheriteddementiaFTDP-17.
Nature1998,393:702–705.
64.
WattsGD,WymerJ,KovachMJ,MehtaSG,MummS,DarvishD,PestronkA,WhyteMP,KimonisVE:InclusionbodymyopathyassociatedwithPagetdiseaseofboneandfrontotemporaldementiaiscausedbymutantvalosin-containingprotein.
NatGenet2004,36:377–381.
65.
DaiRM,LiCC:Valosin-containingproteinisamulti-ubiquitinchain-targetingfactorrequiredinubiquitin-proteasomedegradation.
NatCellBiol2001,3:740–744.
66.
HolmIE,IsaacsAM,MackenzieIR:AbsenceofFUS-immunoreactivepathologyinfrontotemporaldementialinkedtochromosome3(FTD-3)causedbymutationintheCHMP2Bgene.
ActaNeuropathol2009,118:719–720.
67.
SkibinskiG,ParkinsonNJ,BrownJM,ChakrabartiL,LloydSL,HummerichH,NielsenJE,HodgesJR,SpillantiniMG,ThusgaardT,etal:MutationsintheendosomalESCRTIII-complexsubunitCHMP2Binfrontotemporaldementia.
NatGenet2005,37:806–808.
68.
BakerM,MackenzieIR,Pickering-BrownSM,GassJ,RademakersR,LindholmC,SnowdenJ,AdamsonJ,SadovnickAD,RollinsonS,etal:Mutationsinprogranulincausetau-negativefrontotemporaldementialinkedtochromosome17.
Nature2006,442:916–919.
69.
GassJ,CannonA,MackenzieIR,BoeveB,BakerM,AdamsonJ,CrookR,MelquistS,KuntzK,PetersenR,etal:Mutationsinprogranulinareamajorcauseofubiquitin-positivefrontotemporallobardegeneration.
HumMolGenet2006,15:2988–3001.
70.
DeJesus-HernandezM,MackenzieIR,BoeveBF,BoxerAL,BakerM,RutherfordNJ,NicholsonAM,FinchNA,FlynnH,AdamsonJ,etal:ExpandedGGGGCChexanucleotiderepeatinnoncodingregionofC9ORF72causesPanandChenTranslationalNeurodegeneration2013,2:8Page8of9http://www.
translationalneurodegeneration.
com/content/2/1/8chromosome9p-linkedFTDandALS.
Neuron2011,72:245–256.
71.
RentonAE,MajounieE,WaiteA,Simon-SanchezJ,RollinsonS,GibbsJR,SchymickJC,LaaksovirtaH,vanSwietenJC,MyllykangasL,etal:AhexanucleotiderepeatexpansioninC9ORF72isthecauseofchromosome9p21-linkedALS-FTD.
Neuron2011,72:257–268.
72.
MajounieE,RentonAE,MokK,DopperEG,WaiteA,RollinsonS,ChioA,RestagnoG,NicolaouN,Simon-SanchezJ,etal:FrequencyoftheC9orf72hexanucleotiderepeatexpansioninpatientswithamyotrophiclateralsclerosisandfrontotemporaldementia:across-sectionalstudy.
LancetNeurol2012,11:323–330.
73.
GijselinckI,VanLangenhoveT,vanderZeeJ,SleegersK,PhiltjensS,KleinbergerG,JanssensJ,BettensK,VanCauwenbergheC,PeresonS,etal:AC9orf72promoterrepeatexpansioninaFlanders-Belgiancohortwithdisordersofthefrontotemporallobardegeneration-amyotrophiclateralsclerosisspectrum:ageneidentificationstudy.
LancetNeurol2012,11:54–65.
74.
WhitwellJL,XuJ,MandrekarJ,BoeveBF,KnopmanDS,ParisiJE,SenjemML,DicksonDW,PetersenRC,RademakersR,etal:Frontalasymmetryinbehavioralvariantfrontotemporaldementia:clinicoimagingandpathogeneticcorrelates.
NeurobiolAging2012,34:636–639.
75.
ArighiA,FumagalliGG,JaciniF,FenoglioC,GhezziL,PietroboniAM,DeRizM,SerpenteM,RidolfiE,BonsiR,etal:EarlyonsetbehavioralvariantfrontotemporaldementiaduetotheC9ORF72hexanucleotiderepeatexpansion:psychiatricclinicalpresentations.
JAlzheimersDis2012,31:447–452.
76.
Al-SarrajS,KingA,TroakesC,SmithB,MaekawaS,BodiI,RogeljB,Al-ChalabiA,HortobagyiT,ShawCE:p62positive,TDP-43negative,neuronalcytoplasmicandintranuclearinclusionsinthecerebellumandhippocampusdefinethepathologyofC9orf72-linkedFTLDandMND/ALS.
ActaNeuropathol2011,122:691–702.
77.
BoeveBF,BoylanKB,Graff-RadfordNR,DeJesus-HernandezM,KnopmanDS,PedrazaO,VemuriP,JonesD,LoweV,MurrayME,etal:Characterizationoffrontotemporaldementiaand/oramyotrophiclateralsclerosisassociatedwiththeGGGGCCrepeatexpansioninC9ORF72.
Brain2012,135:765–783.
78.
SiebenA,VanLangenhoveT,EngelborghsS,MartinJJ,BoonP,CrasP,DeDeynPP,SantensP,VanBroeckhovenC,CrutsM:Thegeneticsandneuropathologyoffrontotemporallobardegeneration.
ActaNeuropathol2012,124:353–372.
79.
EdwardsTL,ScottWK,AlmonteC,BurtA,PowellEH,BeechamGW,WangL,ZuchnerS,KonidariI,WangG,etal:Genome-wideassociationstudyconfirmsSNPsinSNCAandtheMAPTregionascommonriskfactorsforParkinsondisease.
AnnHumGenet2010,74:97–109.
80.
RademakersR,CrutsM,vanBroeckhovenC:Theroleoftau(MAPT)infrontotemporaldementiaandrelatedtauopathies.
HumMutat2004,24:277–295.
81.
MackenzieIR,NeumannM,BaborieA,SampathuDM,DuPlessisD,JarosE,PerryRH,TrojanowskiJQ,MannDM,LeeVM:AharmonizedclassificationsystemforFTLD-TDPpathology.
ActaNeuropathol2011,122:111–113.
82.
HeZ,BatemanA:Progranulin(granulin-epithelinprecursor,PC-cell-derivedgrowthfactor,acrogranin)mediatestissuerepairandtumorigenesis.
JMolMed(Berl)2003,81:600–612.
83.
VanDammeP,VanHoeckeA,LambrechtsD,VanackerP,BogaertE,vanSwietenJ,CarmelietP,VanDenBoschL,RobberechtW:Progranulinfunctionsasaneurotrophicfactortoregulateneuriteoutgrowthandenhanceneuronalsurvival.
JCellBiol2008,181:37–41.
84.
YinF,BanerjeeR,ThomasB,ZhouP,QianL,JiaT,MaX,MaY,IadecolaC,BealMF,etal:Exaggeratedinflammation,impairedhostdefense,andneuropathologyinprogranulin-deficientmice.
JExpMed2010,207:117–128.
85.
WeihlCC,PestronkA,KimonisVE:Valosin-containingproteindisease:inclusionbodymyopathywithPaget'sdiseaseoftheboneandfronto-temporaldementia.
NeuromusculDisord2009,19:308–315.
86.
JuJS,WeihlCC:p97/VCPattheintersectionoftheautophagyandtheubiquitinproteasomesystem.
Autophagy2010,6:283–285.
87.
JuJS,WeihlCC:Inclusionbodymyopathy,Paget'sdiseaseoftheboneandfronto-temporaldementia:adisorderofautophagy.
HumMolGenet2010,19:R38–R45.
88.
SuzukiM,LeeHC,KayasugaY,ChibaS,NedachiT,MatsuwakiT,YamanouchiK,NishiharaM:Rolesofprogranulininsexualdifferentiationofthedevelopingbrainandadultneurogenesis.
JReprodDev2009,55:351–355.
89.
AhmedZ,ShengH,XuYF,LinWL,InnesAE,GassJ,YuX,WuertzerCA,HouH,ChibaS,etal:Acceleratedlipofuscinosisandubiquitinationingranulinknockoutmicesuggestaroleforprogranulininsuccessfulaging.
AmJPathol2010,177:311–324.
90.
GijselinckI,VanBroeckhovenC,CrutsM:Granulinmutationsassociatedwithfrontotemporallobardegenerationandrelateddisorders:anupdate.
HumMutat2008,29:1373–1386.
doi:10.
1186/2047-9158-2-8Citethisarticleas:PanandChen:Clinic,neuropathologyandmoleculargeneticsoffrontotemporaldementia:amini-review.
TranslationalNeurodegeneration20132:8.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitPanandChenTranslationalNeurodegeneration2013,2:8Page9of9http://www.
translationalneurodegeneration.
com/content/2/1/8
FTLDispathologicallycharacterizedbythefrontalandtemporallobaratrophy.
Frontotemporaldementia(FTD)clinicallypresentswithabnormalitiesofbehaviorandpersonalityandlanguageimpairmentsvariants.
TheclinicalspectrumofFTDencompassesdistinctcanonicalsyndromes:behaviouralvariantofFTD(bvFTD)andprimaryprogressiveaphasia.
Thelaterincludesnonfluent/agrammaticvariantPPA(nfvPPAorPNFA),semanticvariantPPA(svPPAorSD)andlogopenicvariantPPA(lvPPA).
Inaddition,thereisalsooverlapofFTDwithmotorneurondisease(FTD-MNDorFTD-ALS),aswellastheparkinsoniansyndromes,progressivesupranuclearpalsy(PSP)andcorticobasalsyndrome(CBS).
TheFTLDspectrumdisordersarebaseduponthepredominantneuropathologicalproteins(containinginclusionsofhyperphosphorylatedtauorubiquitinprotein,e.
gtransactiveresponse(TAR)DNA-bindingprotein43kDa(TDP-43)andfusedin-sarcomaproteininneuronsandglialcells)intothreemaincategories:(1)microtubule-associatedproteintau(FTLD-Tau);(2)TARDNA-bindingprotein-43(FTLD-TDP);and(3)fusedinsarcomaprotein(FTLD-FUS).
TherearefivemaingenesmutationsleadingclinicalandpathologicalvariantsinFTLDthatidentifiedbymoleculargeneticstudies,whicharechromosome9openreadingframe72(C9ORF72)gene,granulin(GRN)gene,microtubuleassociatedproteintaugene(MAPT),thegeneencodingvalosin-containingprotein(VCP)andthechargedmultivesicularbodyprotein2B(CHMP2B).
Inthisreview,recentadvancesonthedifferentclinicvariants,neuroimaging,genetics,pathologicalsubtypesandclinicopathologicalassociationsofFTDwillbediscussed.
Keywords:bvFTD,Nonfluent/agrammaticvariant,Semanticvariant,Logopenicvariant,Moleculargenetics,MAPT,GRN,C9ORF72IntroductionFrontotemporaldementia(FTD)representsagroupofclinically,neuropathologicallyandgeneticallyhetero-geneousdisorders.
Itisarangeofprogressivedementiasyndromesassociatedwithfocalatrophyoftheorbitomesialfrontalandanteriortemporallobes.
Andthetermfrontotemporallobardegeneration(FTLD)todescribethepathologicalsyndrome.
In1892,ArnoldPickdescribedapatientwithprogressiveaphasiaandlobaratrophy[1].
In1911,AloisAlzheimerdescribedthehistopathologicalstatusrelatedtothesepatients,pointingtheabsenceofsenileplaquesandneuro-fibrillarytangles,andthepresenceofargyrophilicneuronalinclusions(latercalled"Pickbodies")andswollencells(latercalled"Pickcells")atneuropathologicalexamination[2].
However,duringthe20thcentury,thesepatientswithfrontotemporallobardegenerationweregenericallyreferredtoaspatientswithdementia,beingoftendiagnosedwithAlzheimerdisease(AD)[2].
In1994,twomajorresearchgroupsfromLundandManchesterproposedclinicalandneuropathologicalcriteriaforthediagnosisofFTD[3].
In1998,Nearyetal[4]reportedaconsensusonclinicaldiagnosticcriteriaoffrontotemporallobardegenerationintheAmericanAcademyofNeurology(AAN).
FTDoftenbeginswhenthepatientisinthefifthtoseventhdecades.
Epidemiologicalstudiessuggestthat*Correspondence:chenxc998@163.
com1DepartmentofNeurology,UnionHospitalofFujianMedicalUniversity,29XinquanRoad,Fuzhou350001,China2KeyLaboratoryofBrainAgingandNeurodegenerativeDisease;FujianInstituteofGeriatrics,UnionHospitalofFujianMedicalUniversity,29Xinquan,Road,Fuzhou350001,ChinaFulllistofauthorinformationisavailableattheendofthearticleTranslationalNeurodegeneration2013PanandChen;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
PanandChenTranslationalNeurodegeneration2013,2:8http://www.
translationalneurodegeneration.
com/content/2/1/8FTDisthesecondmostcommoncauseofdementiainindividualsyoungerthan65andisjustlesscommonthanAlzheimer'sdisease(AD)withinthisagegroup[2,5].
Ofover65yearsolddementia,theincidenceofFTDranksfourth,thetopthreeisAlzheimer'sdisease,Lewybodydementiaandvasculardementia[5-7].
Theredonotappeartobeanycleargenderdifferencesinsus-ceptibility[8-11].
AmongtheFTDclinicalsyndromes,sexdistributionappearstovaryfromonesubtypetothenext.
SeveralstudiesreportamalepredominanceinbvFTDandSD,andafemalepredominanceinPNFA[5,12].
Thereisawiderangeindurationsofillness(2-20years)partlyreflectingdifferentunderlyingpathologies.
Inthepastfewyears,significantadvanceshavebeenseenintheetiology,pathogenesis,andgenetics,pathologyandclinicalphenotypeofFTD,andmanynewterminologyandclassificationofFTDhaveemerged.
Inthisreview,recentadvancesonthedifferentclinicalvariantphenotypes,neuroimaging,hereditaryforms,pathologicalsubtypesandclinicopathologicalassociationsofFTDwillbediscussed.
FTLDclinicalpresentation:classificationandcharacteristicsFrontotemporallobardegeneration(FTLD)includesagroupofprogressivedegenerativedisorderscharacterisedbyprogressivebehaviouralchange,executivedysfunctionandlanguagedifficulties[13].
UnlikeAD,behavioralsymptomspredominateintheearlystagesofFTLD.
TheclinicalheterogeneityinfamilialandsporadicformsofFTDisremarkable,withpatientsdemonstratingvariablemixturesofdisinhibition,dementia,PSP,CBD,andmotorneurondisease[13,14].
Earlysymptomsaredividedamongcognitive,behavioral,andsometimesmotorabnor-malities,reflectingdegenerationoftheanteriorfrontalandtemporalregions,basalganglia,andmotorneurons[13,14].
FTLDisapowerfulmodeltostudyemotion,socialcognitionandlanguageorganizationinthebrain.
Behavioralvariantfrontotemporaldementia(bvFTD)bvFTDhasthehighestprevalenceamongsttheFTDclinicalsyndromes,accountingforapproximately70%ofallFTDcases[2,5].
TheonsetofbvFTDistypicallybeforetheageof65years,withanaverageonsetageof58years[12,15].
Patientswiththisclinicalvariantpresentwithmarkedchangesinpersonalityandbehaviourandwithrelativepreservationofthecognitivefunctionspraxis,gnosiaandmemory[13,16].
Commonbehavioraldeficitsincludeapathy,disinhibition,weightgain,foodfetishes,compulsions,euphoria,andanabsenceofinsightintotheircondition.
Poorbusinessdecisionsanddifficultyorganizingworktasksarecommon.
Cognitivetestingtypicallyrevealssparedmemorybutimpairedexecutivefunctions[3,13,17].
bvFTDhasbeenassociatedwithsymmetricalventromedialfrontal,orbitalfrontal,andinsularatrophyandleftanteriorcingulateatrophy[18].
BehaviouralassessmentisatthecoreofassessmentinpatientswithpotentialbvFTDandseemstobemoresensitiveindistinguishingbvFTDfromADthanstandardcognitivetesting.
The'InternationalBehavioralVariantFTDCriteriaConsortium'developedinternationalconsensuscriteriaforbvFTD.
Subclassifi-cationsweremadeinpossiblebvFTDdefinedbyclinicalcriteria,probablebvFTDsupportedbyneuroimagingdata,anddefinitebvFTDconfirmationbyneuropathologicalevidenceorapathogenicmutation[17].
Primaryprogressiveaphasia(PPA)PPAisalanguagedisorderthatinvolveschangesintheabilitytospeak,read,writeandunderstandwhatothersaresaying.
Itisassociatedwithearlytemporallobeatrophyorbrainlesionsaroundthelateralfissure.
PPArepresentsaspectrumofselectivelanguagedisordersandthevariantofPPAmightprovidecluestotheunder-lyingpathology[19].
Currentlycerebrospinalfluid(CSF)biomarkershavelimitedabilitytoidentifyPPAreliably,whichmightbeexplainedbythepathologicalheterogeneity.
AnindicationoflowerAβ1-40levelsorthelowerT-tautoAβ1-42ratioinFTD,mightbeusefultodistinguishpatientsfromsubjectsADandcontrolsubjects[20,21].
In2011,criteriawereadoptedfortheclassificationofPPAintothreeclinicalsubtypes:nonfluent/agrammaticvariantPPA(nfvPPAorPNFA),semanticvariantPPA(svPPAorSD)andlogopenicvariantPPA(lvPPA)[22].
TheproposalisanimportantstepforwardinestablishingtheconsistencyofterminologyandclassificationofPPA.
Thediagnosticrecommendationsincludetwosteps.
First,thepatientshouldmeetthebasicstandardofPPA,whichisaninitialpresentationofsignificantdamagetolanguageandaccompaniedbylimiteddailylivingskillsandothercognitiveimpairment.
Second,weneedtoassessthemainlanguagedomains,includingverbalgeneration,repeat,andunderstandingofwordsandsyntax,naming,semanticknowledgeandreading/spellingcharacteristics.
Finally,clinicalvariantswillbedividedbasingonspecificspeechandlanguagefeaturescharacteristicofeachsubtype.
Classificationcanthenbefurtherspecifiedas"imaging-supported"iftheexpectedpatternofatrophyisfoundand"withdefinitepathology"ifpathologicorgeneticdataareavailable.
Therefore,thenewproposalhasaclearpracticalsignificance.
nfvPPAorPNFAisthesecondmostprevalentpres-entationofFTLD,accountingforalarge25%[12].
ThefeatureofnfvPPAincludesgrammaticalerrormakingagrammatismand/orlaboriousspeech,butrelativelypreservedlanguagecomprehension.
Apraxiaofspeech(AOS)ororofacialapraxiaisfrequentlyaccompanyingtheaphasia[15].
SemanticvariantPPA(svPPA)orSDpresentsin20–25%oftheFTLDpatients[12].
svPPAPanandChenTranslationalNeurodegeneration2013,2:8Page2of9http://www.
translationalneurodegeneration.
com/content/2/1/8presentsasignificantlyimpairednamingabilityandwordcomprehension,whilespeechproductionisspared[22,23].
LvPPAorlogopenicprogressiveaphasia[24]ismarkedbyimpairedwordfindinganddifficultrepetition.
lvPPAshowesanimpairedabilitytorepeatsentencesorphrases,spontaneousspeechandasinglewordextractingwhennaming.
UnlikeotherFTDsubtypes,lvPPAgenerallydoesnotproducechangesinbehaviororpersonalityuntillaterstagesofthedisease.
Mostpeoplewithprogressiveaphasiamaintaintheabilitytocareforthemselves,keepupoutsideinterestsand,insomeinstances,remainemployedforafewyearsafteronsetofthedisorder.
LPAismostlyassociatedwithaneuro-pathologicaldiagnosisofAD[25].
ClinicaldistinctionbetweenbvFTD,nfvPPAandsvPPAisoftencomplicatedforthatoverlapoftheclinicalsyndromesbetweenthemcanoccurinadvancedstagesofdisease.
FTLDoverlapswithotherclinicalsyndromeThesubcorticalnucleiandmotorsystemsareinvolvesinFTLDvariants.
Motorneurondysfunction(MND)hasbeendescribedin40%oftheFTLDpatients,referredtoasFTLD-MND.
ThecommoncomorbidityofAmyotrophiclateralsclerosis(ALS)withbehaviorabnormality,cognitiveimpairmentordementiahasbeennoticed[26,27].
FTLDmayprecede,followorcoincidewiththeonsetofmotorsymptoms[28].
OtherdisordersarecloselyrelatedtoFTLD,includingprogressivesupranuclearpalsy(PSP)syndromes,corticobasalsyndrome(CBS),FTDwithparkinsonism(FTDP)andargyrophilicgraindisease(AGD).
PSPandCBSaretwocommonatypicalparkinsoniansyndromesdemonstratingcognitiveandbehaviourdisordersthatoverlapwithFTD.
Ofthem,behavioralandcognitivedysfunctionpromotesthedevelopmentofdementia.
Andextrapyramidalsystemsymptomspresentasbradykinesia,abnormalposture,rigidity,buttremoruncommon.
Theco-occurrenceofAGDinALSisnotuncommon,andcomparablewiththatinanumberofdiseasesbelongingtothetauopathiesorα-synucleinopathies[29].
Motionsystemdamagepresentsasmuscleatrophy.
FTDP-17showinggeneticlinkagetochromosome17,presentswithaclinicalsyn-dromeofautosomaldominantdisinhibition,dementia,parkinsonism,andamyotrophy[30].
TheclinicalpictureresemblesbvFTD,whilecognitivedeficitsincludean-terogradememorydysfunctioninanearlystage,laterthedeteriorationofvisuospatialfunction,orientationandglobalmemoryaregraduallypresented.
Motorsignstypicallyincludethesymmetricalbradykinesiawithoutrestingtremor,incombinationwithaxialrigidityandposturalinstability.
TheearlyclinicalpresentationofAGDissimilartoADbutitislessaggressive,withpatientsmaintainmildcognitiveimpairment(MCI)formanyyears[31].
NeuroimaginginFTLDNeuroimagingplaysacriticalroleindiagnosisofFTD.
NeuroimaginginvestigationscanreliablydifferentiateFTLDsubtypesfromotherdementias,andcanhelpclinicaldiagnosticsbasedonneuropsychiatricsymptoms.
Differentclinicalvariatentshavedifferentformsofbrainatrophy,whichcanbeusedforsomeimportantcluesforearlyclinicaldifferentialdiagnosis.
DTIcandetectwhitematterdamage,differentsubtypesofwhitematterinjuryalsohelpclinicalearlydifferentialdiagnosisofclinicalsubtypesofFTLD[32].
Functionalneuroimagingtechniques,suchas[99mTc]-hexamethylpropyleneamineoximesingle-photonemissioncomputedtomography(SPECT)[33]or[18F]-fluorodeoxyglucose(FDG)-PETareincreasinglybeingusedtohelpwiththediagnosisofFTLD[34].
Arterialspinlabelingimaging(ASL)likeFDG-PETcanbeusedforshowingthehypometabolisminbrainregions.
HypometabolismonFDG-PETisdetectedconsistentlyandreliablyinfrontalbrainregionsinpatientswithbvFTDcomparedwiththosewithAD,whoshowposteriorcingulatehypometabolismearlyinthediseaseprocess[34].
However,inpatientsshowingclearbrainatrophyonstructuralMRI,littleadditionaldiagnosticbenefitisgainedbydoingaPETscan,becausefocalatrophyisapositivepredictivemarkerofFTD.
Theimagingpresen-tationofnfvPPAindicatesthatpredominantleftposteriorfronto-insularatrophyonMRIorpredominantleftposteriorfronto-insularhypoperfusionorhypometabolismonSPECTorPET.
Imaging-supportedsvPPAshowpredominantanteriortemporallobeatrophyand/orthesebrainregionshypoperfusionorhypometabolismonSPECTorPET.
TheimagingoflvPPAmustshowatleastoneofpredominantleftposteriorperisylvianorparietalatrophyonMRIand/orhypoperfusionorhypometabolismonSPECTorPET[22,25,35-37].
FutureinFTLDareverysimilartoimaginginAD–earlydetection,moleculardiagnosis,monitordiseaseprogressionandvalidateandimplementdiseasemodifyingtherapies.
SpecificanatomicpatternsinFTLD,andanamyloid-PETneuroimaging,whichusestheamyloid-β-detecting11C-PittsburghcompoundB,hasshownpromisingresultsindiscriminatingorrule-outatypicalADandFTDcases[38,39]particularlythosepresentingwithlanguagedeficitsratherthanbehaviouralchanges.
MicroPETwith18F-THK523inTautransgenicmicehavebeenreported[40].
Tauspecificimagingscannerthatusesthe18F-THK523maybeapromisingtechniquecomingsooninfuture[40].
FTLDNeuropathologyandcliniconeuropathologicalcorrelationsNeuropathologyThesubtypesofunderlyingpathologicalchangesinpatientswithFTDareclassifiedonthebasisofthePanandChenTranslationalNeurodegeneration2013,2:8Page3of9http://www.
translationalneurodegeneration.
com/content/2/1/8patternofproteindeposition,andarereferredtocollectivelyasfrontotemporallobardegeneration.
Underamicroscope,commonpathologicchangesofFTLDareatrophybrainregionpresentingneuronalloss,spongychangeandgliosisincorticesofatrophiedfrontalandtemporallobes[41,42].
FTDhaveidentifiednovelgeneticdefectsandachromosomallocusinhereditaryformsofFTLD,aswellasnovelclinicneuropathologicalassociations.
Immunohistochemistryallowssubcategorizationofthesedisordersintospecificproteinopathiesbasedonthemajorconstituentoftheinclusions.
(1)FTLD-tau:Onesubtypeispresentedasneuronsandglialcellscontaininginclusionsofhyperphosphorylatedtauprotein,referredtoasFTLD-tau[43].
TaupathologywasassociatedwithFTDwithparkinsonism,PSPsyndromes[44],CBS[45]andAGD[31].
(2)FTLD-UbiquitinorFTLD-U:Over50%oftheFTLDpatientspresentedwithtau-negativeubiquitinstaininginclusions,referredtoasFTLD-UbiquitinorFTLD-U[46].
In80–95%ofthisgroup,inclusionswerefoundtobecomposedoftransactiveresponse(TAR)DNA-bindingprotein43kDa(TDP-43)[47-49],referredtoasFTLD-TDP[50],orTDP-43-negativeFTLD-Ucaseshavinginclusionsoffusedin-sarcomaprotein(FUS),referredtoasFTLD-FUS[43,49,51,52].
However,inasmallnumberofFTLD-Upatients,theinclusionproteinremainsunclear.
ThisgroupisreferredtoasFTLD-ubiquitinproteasomesystem(FTLD-UPS)[46,53].
(3)Dementialackingdistinctivehistopathology(DLDH)[54,55].
(4)Otherraretypes:dementiawithbasophilicinclusionbody,neuronalintermediatefilamentinclusiondisease[52].
AssociationbetweenpathologyandclinicalphenotypeAssociationswerenotedbetweentheclinicalFTLDsubtypesandunderlyingproteinopathies,butastrictonetoonerelationshipislacking.
bvFTDismostlyassociatedwithFTLD-TDP43,somecasesarealsocorrelatedwithFTLD-tau(PiDsubtype).
AnFTLD-FUSproteinopathyisinvariantlyassociatedwithaclinicaldiagnosisofbvFTD,eitherwithorwithoutthesignsofMND.
MicroscopicassessmentofnfaPPAatautopsyoftenrevealsFTLDasso-ciatedwithatauopathy(FTLD-tau).
nfaPPAiscommonlyassociatedwithtaupathology,especiallywhenAOSororofacialapraxiaispresent.
Inmostcases,thepathologyunderlyingnfaPPAwasmixed,includingFTLD-tauandFTLD-TDP43,butwithapredominanceofFTLD-taupathology.
SvPPAis,inmostcases,linkedwithTDP-43-immunoreactivepathology,althoughtaupathologyissometimesobserved.
Somepatientswithpredominantlyrighttemporallobeatrophy(RTLA)areusuallydiagnosedclinicallywitheitherbvFTDorsvPPA[56].
IthasbeensuggestedthatpatientswithbvFTDandRTLAhaveFTLD-taupathology,whereaspatientswithsvPPAandRTLAhaveFTLD-TDP43pathology[56].
svPPApatientswhooftenpresentwithacalculiaisassociatedwithFTLD-tau[57].
LvPAispredominantlyassociatedwithADpathology.
ManypatientswithlvPPAoftenhaveunderlyingADpathology[58-60].
CSFtau:amyloid-βratio[37]andPiBPETimaging[25]studiescanbehelpfulintheidentificationofpatientswhoaremorelikelytohavelvPPAthannfaPPA.
Arecentstudyshowedthat93%ofpatientswithlvPPAonamyloidPETimagingwasfoundPiBpositive,butsvPPAonly9%,nfvPPAis13%,whichsuggeststhatthereissomecommonpathologicalfeaturesbetweenlvPPAandAD[59].
TaupathologywasalsoassociatedwithFTLDwithparkinsonism,PSP,CBD,AGDandPickbodies(PiD)[30,44,61].
Similarly,TDP-43andFUSproteinopathiesarealsocommonlyfoundinMNDwithorwithoutFTLD[52].
Althoughthesearerelativelystrongassociations,theyarenotabsolute,anditiscurrentlynotpossibletopredictwithcertaintytheunderlyingpathologyofspecificFTLDsyndromes.
ExtrapyramidalsystemsymptomsaccompaniedwithapraxiaindicatesthepresenceofCBS,whichmostlyattributestoTaudisease.
WhiledementiawithFTLD-MNDsyndromemostlyattributestoTDP-43pathology[15,45,57].
ThesesuggestthatitiscontributingtotherapeuticstrategyforFTLDthroughelucidatingtherelationshipbetweenpathologicalandclinicalpresentation.
MoleculargeneticsApproximately40%ofpatientswithFTDhaveafamilyhistory[8].
bvFTDisthemostprominentsubtypewithfamilyhistory,especiallywhenconcomitantsymptomsofMNDarepresent(60%),whileSvPPAappearedtobetheleasthereditaryFTLDsubtype(<20%)[62].
Moleculargen-eticstudieshaveidentifiedseveralcommon(MAPT,GRN)andrare(VCP,CHMP2B,TARDBP,FUS)geneticfactorsinhereditaryFTLDoverrecentyears.
In1998microtubuleassociatedproteintau(MAPT)genewasfound,whichlocatedonchromosome17q21.
32,inwhich13%ofthecasesisFTDP-17,thosewhohaveparkinson-likesymptoms[63].
In2004,thegeneencodingvalosin-containingprotein(VCP)genewasfound,locatedonchromosome9p13.
3,whichisassociatedwiththegenesthatcauseFTLDinasso-ciationwithinclusionbodymyopathyandPaget'sdisease[64,65].
In2005,thechargedmultivesicularbodyprotein2B(CHMP2B,alsoknownaschromatin-modifyingprotein2B)genemutations,locatedonchromosome3p11.
2,wasdiscoveredinalargeDanishcohortwithfamilialFTLD[66,67].
In2006,amutatedgenelocatedonchromosomePanandChenTranslationalNeurodegeneration2013,2:8Page4of9http://www.
translationalneurodegeneration.
com/content/2/1/8Table1Clinicalphenotypes,pathologicalandmoleculargeneticspectruminFTLD[13,19,22,35,72,77,78]CoreclinicalfeaturePraxiologicalobstacleLogopathyExtrapyramidalsymptoms+praxiologicalobstacleDyskinesia+praxiologicalobstacleClinicalsyndromeBehavioralvariantFrontotemporaldementia(bvFTD)Primaryprogressiveaphasia(PPA)Corticobasaldegeneration(CBD)progressivesupranuclearpalsy(PSP)FTD-MND/ALSnonfluent/agrammaticvariantPPA(nfvPPA)Semanticsvariation(svPPA)logopenicvariantPPA(lvPPA)BrainmorphologicallyaffectedpartsPrefrontallobeandtemporallobeLeftposteriorfrontallobe,insulaThefront/ventraltemporallobeleftposteriorsuperiortemporallobeandmedialparietallobeFrontalandtemporallobe,BasalgangliaBasalgangliaandbrainstemCortexandmotorneuronBiochemistryandNeuropathologyFTLD-Tau(Picktype,3R-tau)FTLD-TDP43FTLD-TaumorethanFTLD-TDP43,ADlikepathologicalvisibleMostbelongstoFTLD-TDP43;ADlikepathologicalrareAD-likepathologicalcommon;FTLD-TDP43visibleFTLD-Tau(CBDtype,4R-tau)commonFTLD-Tau(PSPtype,4R-tau)commonFTLD-TDP43,FTLD-FUSCausativeandAssociatedGenesC9ORF72PGRN,C9ORF72PGRNMAPTC9ORF72PGRNC9ORF72PGRNMAPTPGRNFUSMAPTMAPTMAPTPGRNC9ORF72C9ORF72VCPVCPVCPVCPVCPVCPCHMP2BCHMP2BCHMP2BCHMP2BCHMP2BNote:3Rtau:threemicrotubulebindingrepeats;4Rtau:fourmicrotubule-bindingrepeats.
PanandChenTranslationalNeurodegeneration2013,2:8Page5of9http://www.
translationalneurodegeneration.
com/content/2/1/817q21.
31areidentifiedasthegranuleproteinprecursor(PGRN),only1.
7MnucleotideawayfromtheMAPT[68,69].
Approximately10%ofpatientswithFTLDisassociatedwiththisgene.
In2011,chromosome9openreadingframe72(C9ORF72)genewasnewlyidentifiedinFTLD[70,71].
Overall,patientswithmutationsinGRN,MAPTandC9ORF72togetheraccountforatleast17%oftotalFTDcases[53,72].
SummedC9ORF72,GRNandMAPTmutationfrequencieswere32-40%[70,73].
MutationsinVCPandCHMP2Barerare,eachexplaininglessthan1%ofthefamilialFTLD.
TheMAPTgenemutationsoftenleadtoFTLD-Taupathologicalchanges.
TheBothPGRNandC9ORF72muta-tionscancauseFTLD-TDP-43.
ThesymmetryfrontallobeatrophyinbvFTDpatientsisassociatedwithC9ORF72andMAPTgenemutations,whereastheasymmetryoffrontallobeatrophyinbvFTDpatientsisassociatedwithPGRNgenemutations[74].
Thelargehexanucleotiderepeatexpansionlocatedwithinthenon-codingportionofC9ORF72isthecauseofchromosome9-linkedALSandFTLD[70].
Thesesuggestthatspecificgenemutationsmayaffectthepatternsofneuroanatomicinjuryinthedevelopmentoffrontallobaratrophy.
C9ORF72isexpressedasthreemajortranscriptsandtheexpandedG4C2repeatislocatedintheproximalregulatoryregionofC9ORF72[70,73],upstreamofoneandinthefirstintronofthetwoothertranscripts.
Repeatexpansionresultsinnearcompletelossofexpressionofthemajorgenetranscripts.
Thepathogenicexpansionwasnon-penetrantinindividualsyoungerthan35years,50%penetrantby58years,andalmostfullypenetrantby80years.
Innormalpopulation,thesizeoftheG4C2repeatrangesfrom3to25units,whichisexpandedtoatleast60unitsinFTLDpatients[70,71,73].
TheclinicalphenotypeofC9ORF72mutationoftenpresentsasbvFTDorALSorFTDco-morbiditiesALS.
InpatientswithbvFTD,C9ORF72mutationismorecommonthanMAPTorPGRN.
Anxietyoragitation,andmemorydysfunction(oftenepisodicmemory)isacommonclinicalfeature.
Thosecasesunderlinesthatthehexanucleotiderepeatexpansioninchromosome9couldbealsoassociatedwithearlyonsetpsychiatricpresentations[75].
Overexpressedp-62inclusionbodylesionsinthecere-bellumisoneofpathologicalfeatures[76].
Neuroimagingpresentsasthesymmetricalfrontaland/ortemporallobeatrophy,andparietal,occipitalandcerebellaratrophycanalsoappear.
Therefore,C9ORF72mutationisnotonlyas-sociatedwithcorticalanatomicsitebutalsowithsub-corticalstructures.
However,itisunclearfortheexactmechanismofactionofthis"repeatamplificationC9ORF72gene".
TheclinicalandpathologicalheterogeneityinFTLDcausesachallengefordiagnosisofFTLD.
AhelpfulTable2TheprofileofmaingenesmutationanditspossiblediseasemechanismsinFTLDGenesymbolMAPTC9ORF72PGRNVCPCHMP2BFullnameMicrotubule-associatedproteintauChromosome9openreadingframe72ProgranulinValosincontainingproteinChromatinmodifyingprotein2BChromosomallocalization17q21.
329p21.
217q21.
329p13.
33p11.
2.
MAPTgivesrisetosixisoforms:threeisoformscontainingthreeamino-acidrepeats(3R),andthreeisoformswithfourrepeats(4R)[79].
expressedasthreemajortranscripts,theexpandedG4C2repeatislocatedintheproximalregulatoryregionofC9ORF72[70,73].
encodesprogranulin,aubiquitouslyexpressedgrowthfactorprecursorconsistingof7.
5granulinpeptides.
EncodesaubiquitouslyexpressedmemberofafamilyofATPasesassociatedwithawiderangeofcellularfunctions[85].
EncodesacomponentoftheheteromericESCRT-IIIcomplexwithfunctionsintheendosomal-lysosomalandtheautophagicproteindegradationpathway.
FunctionsandpossibleroleinthediseasemechanismMutationsresultinachangeinratioof3Rto4Rtauisoforms.
Mutationsaffectthenormalfunctionofthetauproteintostabilisemicrotubules,increasethetendencyoftautoformneurotoxicaggregatesanddisturbneuronalplasticityandaxonaltransport[80].
Repeatexpansionresultsinnearcompletelossofthemajorgenetranscripts.
AndaccumulationoftranscriptsharboringtheexpandedG4C2repeatinnuclearRNAfoci[70].
awiderangeofbiologicalprocessessuchasinflammationandwoundrepair,orinpathologicalconditionsincludingtumorigenesis[82].
mutationsresideattheinterfacebetweentheD1ATPaseandtheN-domainoftheCDC48-likeprotein[85].
Expressedinneuronsofallmajorbrainregions.
Itiscriticalfordevelopment,sexualdifferentiation[88]andneuronalsurvival[89].
G4C2repeatleadstoneuronalcytoplasmicinclusionsthroughouttheentirecorticalthickness[81].
Neurotrophicfunctioninvolvedinneuronalsurvivalandneuriteoutgrowth[83,84].
mutationsdisturbubiquitin-proteasomemediatedproteindegradation,autophagy,orboth[86,87].
MutationsaffecttheC-terminalendoftheproteinduetoaberrantsplicing[78].
unidentifiedmechanismsexist.
Estimatedmutationfrequency[69,72,79,81,90]0-50%14-48%3–26%<1%<1%PanandChenTranslationalNeurodegeneration2013,2:8Page6of9http://www.
translationalneurodegeneration.
com/content/2/1/8supplementforclinicalevaluationusinggeneticsandbiologicalmarkerstestingcansignificantlyimprovetheforecastofpotentialhistopathologyinvivo.
Wesummarizeclinicalphenotypes,molecularpathologicalandgeneticspectruminFTLDinTable1.
Andtheprofileofmaingenesmutationsanditspossiblediseasemecha-nismsinFTLDisshowninTable2.
ConclusionInthisreview,wehavesystematicallyupdatedcurrentunderstandingonclinical,genetic,neuropathological,andneuroimagingperspectivesofFTD.
ThisreviewaimstoarouseawarenessofFTDamongclinicians,inpar-ticularwhentheoverlappingclinicalandneuroimagingcharacteristicfeaturesamongdementiaanddifferentsubtypesofFTDremaingreatchallengesforclinicians.
IdentificationofbiomarkersforclinicaldiagnosisanddifferentiationFTDfromotherdementiaiswarrantedforfuturestudies.
Genediagnosistestshouldbecon-sideredforfamilialcasessuspectedwithFTDinclinicpractice.
Longitudinalclinicopathologicalcorrelationstudieswillfurtherelucidatethenetworkfunctionsofhumanbraininthiscomplexdisorderwithbehaviour,speechandmotorabnormality.
Withfurtherunder-standingofthegenetics,clinicalandneuropathologicalbasisofFTD,wecanvisualisethatFTDwillbefurtherclinicallydefined.
Andnewconsensuswillbedevelopedforbetterguidanceinclinicalpractice.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authors'contributionsXdPcollectedthereferencematerialsanddraftedthemanuscript.
XcCrevisedthemanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
AcknowledgementsThisworkwassupportedbythegrantsfromtheNationalNaturalScienceFoundationofChina(81200991),OutstandingYoungPersons'ResearchProgramforHigherEducationofFujianProvince,China(JA10123),MajorProjectofFujianScienceandTechnologyBureau(2009D061).
Authordetails1DepartmentofNeurology,UnionHospitalofFujianMedicalUniversity,29XinquanRoad,Fuzhou350001,China.
2KeyLaboratoryofBrainAgingandNeurodegenerativeDisease;FujianInstituteofGeriatrics,UnionHospitalofFujianMedicalUniversity,29Xinquan,Road,Fuzhou350001,China.
3CentreofNeurobiology,FujianMedicalUniversity,88JiaotongRoad,Fuzhou350001,China.
Received:29December2012Accepted:8April2013Published:19April2013References1.
RossorMN:Pick'sdisease:aclinicaloverview.
Neurology2001,56:S3–S5.
2.
SnowdenJS,NearyD,MannDM:Frontotemporaldementia.
BrJPsychiatry2002,180:140–143.
3.
TheLundandManchesterGroups:Clinicalandneuropathologicalcriteriaforfrontotemporaldementia.
JNeurolNeurosurgPsychiatry1994,57:416–418.
4.
NearyD,SnowdenJS,GustafsonL,PassantU,StussD,BlackS,FreedmanM,KerteszA,RobertPH,AlbertM,etal:Frontotemporallobardegeneration:aconsensusonclinicaldiagnosticcriteria.
Neurology1998,51:1546–1554.
5.
RatnavalliE,BrayneC,DawsonK,HodgesJR:Theprevalenceoffrontotemporaldementia.
Neurology2002,58:1615–1621.
6.
ArvanitakisZ:Updateonfrontotemporaldementia.
Neurologist2010,16:16–22.
7.
BarkerWW,LuisCA,KashubaA,LuisM,HarwoodDG,LoewensteinD,WatersC,JimisonP,ShepherdE,SevushS,etal:RelativefrequenciesofAlzheimerdisease,Lewybody,vascularandfrontotemporaldementia,andhippocampalsclerosisintheStateofFloridaBrainBank.
AlzheimerDisAssocDisord2002,16:203–212.
8.
RossoSM,DonkerKaatL,BaksT,JoosseM,deKoningI,PijnenburgY,deJongD,DooijesD,KamphorstW,RavidR,etal:FrontotemporaldementiainTheNetherlands:patientcharacteristicsandprevalenceestimatesfromapopulation-basedstudy.
Brain2003,126:2016–2022.
9.
MercyL,HodgesJR,DawsonK,BarkerRA,BrayneC:Incidenceofearly-onsetdementiasinCambridgeshire,UnitedKingdom.
Neurology2008,71:1496–1499.
10.
IkedaM,IshikawaT,TanabeH:Epidemiologyoffrontotemporallobardegeneration.
DementGeriatrCognDisord2004,17:265–268.
11.
HouCE,YaffeK,Perez-StableEJ,MillerBL:Frequencyofdementiaetiologiesinfourethnicgroups.
DementGeriatrCognDisord2006,22:42–47.
12.
JohnsonJK,DiehlJ,MendezMF,NeuhausJ,ShapiraJS,FormanM,ChuteDJ,RobersonED,Pace-SavitskyC,NeumannM,etal:Frontotemporallobardegeneration:demographiccharacteristicsof353patients.
ArchNeurol2005,62:925–930.
13.
PiguetO,HornbergerM,MioshiE,HodgesJR:Behavioural-variantfrontotemporaldementia:diagnosis,clinicalstaging,andmanagement.
LancetNeurol2011,10:162–172.
14.
LilloP,GarcinB,HornbergerM,BakTH,HodgesJR:Neurobehavioralfeaturesinfrontotemporaldementiawithamyotrophiclateralsclerosis.
ArchNeurol2010,67:826–830.
15.
JosephsKA,HodgesJR,SnowdenJS,MackenzieIR,NeumannM,MannDM,DicksonDW:Neuropathologicalbackgroundofphenotypicalvariabilityinfrontotemporaldementia.
ActaNeuropathol2011,122:137–153.
16.
BathgateD,SnowdenJS,VarmaA,BlackshawA,NearyD:Behaviourinfrontotemporaldementia,Alzheimer'sdiseaseandvasculardementia.
ActaNeurolScand2001,103:367–378.
17.
RascovskyK,HodgesJR,KnopmanD,MendezMF,KramerJH,NeuhausJ,vanSwietenJC,SeelaarH,DopperEG,OnyikeCU,etal:Sensitivityofreviseddiagnosticcriteriaforthebehaviouralvariantoffrontotemporaldementia.
Brain2011,134:2456–2477.
18.
RohrerJD,LashleyT,SchottJM,WarrenJE,MeadS,IsaacsAM,BeckJ,HardyJ,deSilvaR,WarringtonE,etal:Clinicalandneuroanatomicalsignaturesoftissuepathologyinfrontotemporallobardegeneration.
Brain2011,134:2565–2581.
19.
GrossmanM:Primaryprogressiveaphasia:clinicopathologicalcorrelations.
NatRevNeurol2010,6:88–97.
20.
IrwinDJ,McMillanCT,ToledoJB,ArnoldSE,ShawLM,WangLS,VanDeerlinV,LeeVM,TrojanowskiJQ,GrossmanM:ComparisonofcerebrospinalfluidlevelsoftauandAbeta1-42inAlzheimerdiseaseandfrontotemporaldegenerationusing2analyticalplatforms.
ArchNeurol2012,69:1018–1025.
21.
VerweyNA,KesterMI,vanderFlierWM,VeerhuisR,BerkhofH,TwaalfhovenH,BlankensteinMA,ScheltensAP,PijnenburgYA:AdditionalvalueofCSFamyloid-beta40levelsinthedifferentiationbetweenFTLDandcontrolsubjects.
JAlzheimersDis2010,20:445–452.
22.
Gorno-TempiniML,HillisAE,WeintraubS,KerteszA,MendezM,CappaSF,OgarJM,RohrerJD,BlackS,BoeveBF,etal:Classificationofprimaryprogressiveaphasiaanditsvariants.
Neurology2011,76:1006–1014.
23.
SnowdenJS,ThompsonJC,StopfordCL,RichardsonAM,GerhardA,NearyD,MannDM:Theclinicaldiagnosisofearly-onsetdementias:diagnosticaccuracyandclinicopathologicalrelationships.
Brain2011,134:2478–2492.
24.
Gorno-TempiniML,BrambatiSM,GinexV,OgarJ,DronkersNF,MarconeA,PeraniD,GaribottoV,CappaSF,MillerBL:Thelogopenic/phonologicalvariantofprimaryprogressiveaphasia.
Neurology2008,71:1227–1234.
25.
RabinoviciGD,JagustWJ,FurstAJ,OgarJM,RacineCA,MorminoEC,O'NeilJP,LalRA,DronkersNF,MillerBL,etal:Abetaamyloidandglucosemetabolisminthreevariantsofprimaryprogressiveaphasia.
AnnNeurol2008,64:388–401.
26.
PhukanJ,PenderNP,HardimanO:Cognitiveimpairmentinamyotrophiclateralsclerosis.
LancetNeurol2007,6:994–1003.
27.
RingholzGM,AppelSH,BradshawM,CookeNA,MosnikDM,SchulzPE:PrevalenceandpatternsofcognitiveimpairmentinsporadicALS.
Neurology2005,65:586–590.
PanandChenTranslationalNeurodegeneration2013,2:8Page7of9http://www.
translationalneurodegeneration.
com/content/2/1/828.
vanLangenhoveT,vanderZeeJ,vanBroeckhovenC:Themolecularbasisofthefrontotemporallobardegeneration-amyotrophiclateralsclerosisspectrum.
AnnMed2012,44:817–828.
29.
SomaK,FuYJ,WakabayashiK,OnoderaO,KakitaA,TakahashiH:Co-occurrenceofargyrophilicgraindiseaseinsporadicamyotrophiclateralsclerosis.
NeuropatholApplNeurobiol2012,38:54–60.
30.
SpillantiniMG,BirdTD,GhettiB:FrontotemporaldementiaandParkinsonismlinkedtochromosome17:anewgroupoftauopathies.
BrainPathol1998,8:387–402.
31.
FerrerI,SantpereG,vanLeeuwenFW:Argyrophilicgraindisease.
Brain2008,131:1416–1432.
32.
ZhangY,SchuffN,DuAT,RosenHJ,KramerJH,Gorno-TempiniML,MillerBL,WeinerMW:WhitematterdamageinfrontotemporaldementiaandAlzheimer'sdiseasemeasuredbydiffusionMRI.
Brain2009,132:2579–2592.
33.
VarmaAR,AdamsW,LloydJJ,CarsonKJ,SnowdenJS,TestaHJ,JacksonA,NearyD:DiagnosticpatternsofregionalatrophyonMRIandregionalcerebralbloodflowchangeonSPECTinyoungonsetpatientswithAlzheimer'sdisease,frontotemporaldementiaandvasculardementia.
ActaNeurolScand2002,105:261–269.
34.
KandaT,IshiiK,UemuraT,MiyamotoN,YoshikawaT,KonoAK,MoriE:ComparisonofgreymatterandmetabolicreductionsinfrontotemporaldementiausingFDG-PETandvoxel-basedmorphometricMRstudies.
EurJNuclMedMolImaging2008,35:2227–2234.
35.
GrossmanM:Thenon-fluent/agrammaticvariantofprimaryprogressiveaphasia.
LancetNeurol2012,11:545–555.
36.
GrossmanM,PowersJ,AshS,McMillanC,BurkholderL,IrwinD,TrojanowskiJQ:Disruptionoflarge-scaleneuralnetworksinnon-fluent/agrammaticvariantprimaryprogressiveaphasiaassociatedwithfrontotemporaldegenerationpathology.
BrainLang2012.
inPress,doi:10.
1016/j.
bandl.
2012.
10.
005.
[Epubaheadofprint],PMID:23218686.
37.
HuWT,McMillanC,LibonD,LeightS,FormanM,LeeVM,TrojanowskiJQ,GrossmanM:MultimodalpredictorsforAlzheimerdiseaseinnonfluentprimaryprogressiveaphasia.
Neurology2010,75:595–602.
38.
EnglerH,SantilloAF,WangSX,LindauM,SavitchevaI,NordbergA,LannfeltL,LangstromB,KilanderL:InvivoamyloidimagingwithPETinfrontotemporaldementia.
EurJNuclMedMolImaging2008,35:100–106.
39.
RoweCC,NgS,AckermannU,GongSJ,PikeK,SavageG,CowieTF,DickinsonKL,MaruffP,DarbyD,etal:Imagingbeta-amyloidburdeninaginganddementia.
Neurology2007,68:1718–1725.
40.
Fodero-TavolettiMT,OkamuraN,FurumotoS,MulliganRS,ConnorAR,McLeanCA,CaoD,RigopoulosA,CartwrightGA,O'KeefeG,etal:18F-THK523:anovelinvivotauimagingligandforAlzheimer'sdisease.
Brain2011,134:1089–1100.
41.
BroeM,HodgesJR,SchofieldE,ShepherdCE,KrilJJ,HallidayGM:Stagingdiseaseseverityinpathologicallyconfirmedcasesoffrontotemporaldementia.
Neurology2003,60:1005–1011.
42.
KersaitisC,HallidayGM,KrilJJ:Regionalandcellularpathologyinfrontotemporaldementia:relationshiptostageofdiseaseincaseswithandwithoutPickbodies.
ActaNeuropathol2004,108:515–523.
43.
MackenzieIR,RademakersR,NeumannM:TDP-43andFUSinamyotrophiclateralsclerosisandfrontotemporaldementia.
LancetNeurol2010,9:995–1007.
44.
HoglingerGU,MelhemNM,DicksonDW,SleimanPM,WangLS,KleiL,RademakersR,deSilvaR,LitvanI,RileyDE,etal:Identificationofcommonvariantsinfluencingriskofthetauopathyprogressivesupranuclearpalsy.
NatGenet2011,43:699–705.
45.
BoeveBF:Themultiplephenotypesofcorticobasalsyndromeandcorticobasaldegeneration:implicationsforfurtherstudy.
JMolNeurosci2011,45:350–353.
46.
MackenzieIR,NeumannM,BigioEH,CairnsNJ,AlafuzoffI,KrilJ,KovacsGG,GhettiB,HallidayG,HolmIE,etal:Nomenclatureforneuropathologicsubtypesoffrontotemporallobardegeneration:consensusrecommendations.
ActaNeuropathol2009,117:15–18.
47.
BenajibaL,LeBerI,CamuzatA,LacosteM,Thomas-AnterionC,CouratierP,LegallicS,SalachasF,HannequinD,DecoususM,etal:TARDBPmutationsinmotoneurondiseasewithfrontotemporallobardegeneration.
AnnNeurol2009,65:470–473.
48.
NeumannM,SampathuDM,KwongLK,TruaxAC,MicsenyiMC,ChouTT,BruceJ,SchuckT,GrossmanM,ClarkCM,etal:UbiquitinatedTDP-43infrontotemporallobardegenerationandamyotrophiclateralsclerosis.
Science2006,314:130–133.
49.
MackenzieIR,FotiD,WoulfeJ,HurwitzTA:Atypicalfrontotemporallobardegenerationwithubiquitin-positive,TDP-43-negativeneuronalinclusions.
Brain2008,131:1282–1293.
50.
GrossmanM,WoodEM,MooreP,NeumannM,KwongL,FormanMS,ClarkCM,McCluskeyLF,MillerBL,LeeVM,etal:TDP-43pathologiclesionsandclinicalphenotypeinfrontotemporallobardegenerationwithubiquitin-positiveinclusions.
ArchNeurol2007,64:1449–1454.
51.
MackenzieIR,MunozDG,KusakaH,YokotaO,IshiharaK,RoeberS,KretzschmarHA,CairnsNJ,NeumannM:DistinctpathologicalsubtypesofFTLD-FUS.
ActaNeuropathol2011,121:207–218.
52.
RoeberS,MackenzieIR,KretzschmarHA,NeumannM:TDP-43-negativeFTLD-Uisasignificantnewclinico-pathologicalsubtypeofFTLD.
ActaNeuropathol2008,116:147–157.
53.
RohrerJD,GuerreiroR,VandrovcovaJ,UphillJ,ReimanD,BeckJ,IsaacsAM,AuthierA,FerrariR,FoxNC,etal:Theheritabilityandgeneticsoffrontotemporallobardegeneration.
Neurology2009,73:1451–1456.
54.
GiannakopoulosP,HofPR,BourasC:Dementialackingdistinctivehistopathology:clinicopathologicalevaluationof32cases.
ActaNeuropathol1995,89:346–355.
55.
JosephsKA,JonesAG,DicksonDW:Hippocampalsclerosisandubiquitin-positiveinclusionsindementialackingdistinctivehistopathology.
DementGeriatrCognDisord2004,17:342–345.
56.
GainottiG:Differentpatternsoffamouspeoplerecognitiondisordersinpatientswithrightandleftanteriortemporallesions:asystematicreview.
Neuropsychologia2007,45:1591–1607.
57.
RabinoviciGD,MillerBL:Frontotemporallobardegeneration:epidemiology,pathophysiology,diagnosisandmanagement.
CNSDrugs2010,24:375–398.
58.
JosephsKA,WhitwellJL,DuffyJR,VanvoorstWA,StrandEA,HuWT,BoeveBF,Graff-RadfordNR,ParisiJE,KnopmanDS,etal:ProgressiveaphasiasecondarytoAlzheimerdiseasevsFTLDpathology.
Neurology2008,70:25–34.
59.
MesulamM,WicklundA,JohnsonN,RogalskiE,LegerGC,RademakerA,WeintraubS,BigioEH:Alzheimerandfrontotemporalpathologyinsubsetsofprimaryprogressiveaphasia.
AnnNeurol2008,63:709–719.
60.
RohrerJD,RossorMN,WarrenJD:Alzheimer'spathologyinprimaryprogressiveaphasia.
NeurobiolAging2012,33:744–752.
61.
NearyD,SnowdenJ,MannD:Frontotemporaldementia.
LancetNeurol2005,4:771–780.
62.
GoldmanJS,FarmerJM,WoodEM,JohnsonJK,BoxerA,NeuhausJ,Lomen-HoerthC,WilhelmsenKC,LeeVM,GrossmanM,etal:ComparisonoffamilyhistoriesinFTLDsubtypesandrelatedtauopathies.
Neurology2005,65:1817–1819.
63.
HuttonM,LendonCL,RizzuP,BakerM,FroelichS,HouldenH,Pickering-BrownS,ChakravertyS,IsaacsA,GroverA,etal:Associationofmissenseand50-splice-sitemutationsintauwiththeinheriteddementiaFTDP-17.
Nature1998,393:702–705.
64.
WattsGD,WymerJ,KovachMJ,MehtaSG,MummS,DarvishD,PestronkA,WhyteMP,KimonisVE:InclusionbodymyopathyassociatedwithPagetdiseaseofboneandfrontotemporaldementiaiscausedbymutantvalosin-containingprotein.
NatGenet2004,36:377–381.
65.
DaiRM,LiCC:Valosin-containingproteinisamulti-ubiquitinchain-targetingfactorrequiredinubiquitin-proteasomedegradation.
NatCellBiol2001,3:740–744.
66.
HolmIE,IsaacsAM,MackenzieIR:AbsenceofFUS-immunoreactivepathologyinfrontotemporaldementialinkedtochromosome3(FTD-3)causedbymutationintheCHMP2Bgene.
ActaNeuropathol2009,118:719–720.
67.
SkibinskiG,ParkinsonNJ,BrownJM,ChakrabartiL,LloydSL,HummerichH,NielsenJE,HodgesJR,SpillantiniMG,ThusgaardT,etal:MutationsintheendosomalESCRTIII-complexsubunitCHMP2Binfrontotemporaldementia.
NatGenet2005,37:806–808.
68.
BakerM,MackenzieIR,Pickering-BrownSM,GassJ,RademakersR,LindholmC,SnowdenJ,AdamsonJ,SadovnickAD,RollinsonS,etal:Mutationsinprogranulincausetau-negativefrontotemporaldementialinkedtochromosome17.
Nature2006,442:916–919.
69.
GassJ,CannonA,MackenzieIR,BoeveB,BakerM,AdamsonJ,CrookR,MelquistS,KuntzK,PetersenR,etal:Mutationsinprogranulinareamajorcauseofubiquitin-positivefrontotemporallobardegeneration.
HumMolGenet2006,15:2988–3001.
70.
DeJesus-HernandezM,MackenzieIR,BoeveBF,BoxerAL,BakerM,RutherfordNJ,NicholsonAM,FinchNA,FlynnH,AdamsonJ,etal:ExpandedGGGGCChexanucleotiderepeatinnoncodingregionofC9ORF72causesPanandChenTranslationalNeurodegeneration2013,2:8Page8of9http://www.
translationalneurodegeneration.
com/content/2/1/8chromosome9p-linkedFTDandALS.
Neuron2011,72:245–256.
71.
RentonAE,MajounieE,WaiteA,Simon-SanchezJ,RollinsonS,GibbsJR,SchymickJC,LaaksovirtaH,vanSwietenJC,MyllykangasL,etal:AhexanucleotiderepeatexpansioninC9ORF72isthecauseofchromosome9p21-linkedALS-FTD.
Neuron2011,72:257–268.
72.
MajounieE,RentonAE,MokK,DopperEG,WaiteA,RollinsonS,ChioA,RestagnoG,NicolaouN,Simon-SanchezJ,etal:FrequencyoftheC9orf72hexanucleotiderepeatexpansioninpatientswithamyotrophiclateralsclerosisandfrontotemporaldementia:across-sectionalstudy.
LancetNeurol2012,11:323–330.
73.
GijselinckI,VanLangenhoveT,vanderZeeJ,SleegersK,PhiltjensS,KleinbergerG,JanssensJ,BettensK,VanCauwenbergheC,PeresonS,etal:AC9orf72promoterrepeatexpansioninaFlanders-Belgiancohortwithdisordersofthefrontotemporallobardegeneration-amyotrophiclateralsclerosisspectrum:ageneidentificationstudy.
LancetNeurol2012,11:54–65.
74.
WhitwellJL,XuJ,MandrekarJ,BoeveBF,KnopmanDS,ParisiJE,SenjemML,DicksonDW,PetersenRC,RademakersR,etal:Frontalasymmetryinbehavioralvariantfrontotemporaldementia:clinicoimagingandpathogeneticcorrelates.
NeurobiolAging2012,34:636–639.
75.
ArighiA,FumagalliGG,JaciniF,FenoglioC,GhezziL,PietroboniAM,DeRizM,SerpenteM,RidolfiE,BonsiR,etal:EarlyonsetbehavioralvariantfrontotemporaldementiaduetotheC9ORF72hexanucleotiderepeatexpansion:psychiatricclinicalpresentations.
JAlzheimersDis2012,31:447–452.
76.
Al-SarrajS,KingA,TroakesC,SmithB,MaekawaS,BodiI,RogeljB,Al-ChalabiA,HortobagyiT,ShawCE:p62positive,TDP-43negative,neuronalcytoplasmicandintranuclearinclusionsinthecerebellumandhippocampusdefinethepathologyofC9orf72-linkedFTLDandMND/ALS.
ActaNeuropathol2011,122:691–702.
77.
BoeveBF,BoylanKB,Graff-RadfordNR,DeJesus-HernandezM,KnopmanDS,PedrazaO,VemuriP,JonesD,LoweV,MurrayME,etal:Characterizationoffrontotemporaldementiaand/oramyotrophiclateralsclerosisassociatedwiththeGGGGCCrepeatexpansioninC9ORF72.
Brain2012,135:765–783.
78.
SiebenA,VanLangenhoveT,EngelborghsS,MartinJJ,BoonP,CrasP,DeDeynPP,SantensP,VanBroeckhovenC,CrutsM:Thegeneticsandneuropathologyoffrontotemporallobardegeneration.
ActaNeuropathol2012,124:353–372.
79.
EdwardsTL,ScottWK,AlmonteC,BurtA,PowellEH,BeechamGW,WangL,ZuchnerS,KonidariI,WangG,etal:Genome-wideassociationstudyconfirmsSNPsinSNCAandtheMAPTregionascommonriskfactorsforParkinsondisease.
AnnHumGenet2010,74:97–109.
80.
RademakersR,CrutsM,vanBroeckhovenC:Theroleoftau(MAPT)infrontotemporaldementiaandrelatedtauopathies.
HumMutat2004,24:277–295.
81.
MackenzieIR,NeumannM,BaborieA,SampathuDM,DuPlessisD,JarosE,PerryRH,TrojanowskiJQ,MannDM,LeeVM:AharmonizedclassificationsystemforFTLD-TDPpathology.
ActaNeuropathol2011,122:111–113.
82.
HeZ,BatemanA:Progranulin(granulin-epithelinprecursor,PC-cell-derivedgrowthfactor,acrogranin)mediatestissuerepairandtumorigenesis.
JMolMed(Berl)2003,81:600–612.
83.
VanDammeP,VanHoeckeA,LambrechtsD,VanackerP,BogaertE,vanSwietenJ,CarmelietP,VanDenBoschL,RobberechtW:Progranulinfunctionsasaneurotrophicfactortoregulateneuriteoutgrowthandenhanceneuronalsurvival.
JCellBiol2008,181:37–41.
84.
YinF,BanerjeeR,ThomasB,ZhouP,QianL,JiaT,MaX,MaY,IadecolaC,BealMF,etal:Exaggeratedinflammation,impairedhostdefense,andneuropathologyinprogranulin-deficientmice.
JExpMed2010,207:117–128.
85.
WeihlCC,PestronkA,KimonisVE:Valosin-containingproteindisease:inclusionbodymyopathywithPaget'sdiseaseoftheboneandfronto-temporaldementia.
NeuromusculDisord2009,19:308–315.
86.
JuJS,WeihlCC:p97/VCPattheintersectionoftheautophagyandtheubiquitinproteasomesystem.
Autophagy2010,6:283–285.
87.
JuJS,WeihlCC:Inclusionbodymyopathy,Paget'sdiseaseoftheboneandfronto-temporaldementia:adisorderofautophagy.
HumMolGenet2010,19:R38–R45.
88.
SuzukiM,LeeHC,KayasugaY,ChibaS,NedachiT,MatsuwakiT,YamanouchiK,NishiharaM:Rolesofprogranulininsexualdifferentiationofthedevelopingbrainandadultneurogenesis.
JReprodDev2009,55:351–355.
89.
AhmedZ,ShengH,XuYF,LinWL,InnesAE,GassJ,YuX,WuertzerCA,HouH,ChibaS,etal:Acceleratedlipofuscinosisandubiquitinationingranulinknockoutmicesuggestaroleforprogranulininsuccessfulaging.
AmJPathol2010,177:311–324.
90.
GijselinckI,VanBroeckhovenC,CrutsM:Granulinmutationsassociatedwithfrontotemporallobardegenerationandrelateddisorders:anupdate.
HumMutat2008,29:1373–1386.
doi:10.
1186/2047-9158-2-8Citethisarticleas:PanandChen:Clinic,neuropathologyandmoleculargeneticsoffrontotemporaldementia:amini-review.
TranslationalNeurodegeneration20132:8.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitPanandChenTranslationalNeurodegeneration2013,2:8Page9of9http://www.
translationalneurodegeneration.
com/content/2/1/8
- rulewww.163gg.com相关文档
- 交易www.163gg.com
- protocolswww.163gg.com
- 抽样www.163gg.com
- circulationwww.163gg.com
- 邮箱www.163gg.com
- 10.1www.163gg.com
随风云-内蒙古三线BGP 2-2 5M 25/月 ,香港CN2 25/月 ,美国CERA 25/月 所有云服务器均支持5天无理由退款
公司成立于2021年,专注为用户提供低价高性能云计算产品,致力于云计算应用的易用性开发,面向全球客户提供基于云计算的IT解决方案与客户服务,拥有丰富的国内BGP、三线高防、香港等优质的IDC资源。公司一直秉承”以人为本、客户为尊、永续创新”的价值观,坚持”以微笑收获友善, 以尊重收获理解,以责任收获支持,以谦卑收获成长”的行为观向客户提供全面优质的互...

哪里购买香港云服务器便宜?易探云2核2G低至18元/月起;BGP线路年付低至6.8折
哪里购买香港云服务器便宜?众所周知,国内购买云服务器大多数用户会选择阿里云或腾讯云,但是阿里云香港云服务器不仅平时没有优惠,就连双十一、618、开年采购节这些活动也很少给出优惠。那么,腾讯云虽然海外云有优惠活动,但仅限新用户,购买过腾讯云服务器的用户就不会有优惠了。那么,我们如果想买香港云服务器,怎么样购买香港云服务器便宜和优惠呢?下面,云服务器网(yuntue.com)小编就介绍一下!我们都知道...
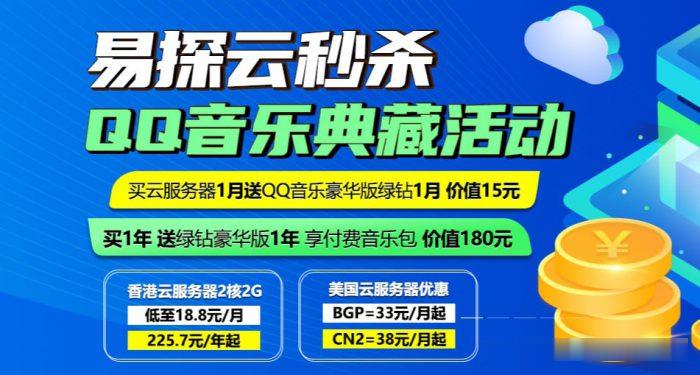
HostYun(月18元),CN2直连香港大带宽VPS 50M带宽起
对于如今的云服务商的竞争着实很激烈,我们可以看到国内国外服务商的各种内卷,使得我们很多个人服务商压力还是比较大的。我们看到这几年的服务商变动还是比较大的,很多新服务商坚持不超过三个月,有的是多个品牌同步进行然后分别的跑路赚一波走人。对于我们用户来说,便宜的服务商固然可以试试,但是如果是不确定的,建议月付或者主力业务尽量的还是注意备份。HostYun 最近几个月还是比较活跃的,在前面也有多次介绍到商...

www.163gg.com为你推荐
-
淘宝门户中国有哪些行业门户网站嘉兴商标注册怎么查商标注册日期甲骨文不满赔偿如果合同期不满被单位辞退,用人单位是否需要赔偿同ip网站同IP的两个网站,做单向链接,会不会被K掉??haokandianyingwang谁给个好看的电影网站看看。www.119mm.comwww.kb119.com 这个网站你们能打开不?www.niuav.com在那能找到免费高清电影网站呢 ?抓站工具大家在家用什么工具练站?怎么固定?面壁思过?在医院是站站立架kb123.netwww.zhmmjyw.net百度收录慢?hao.rising.cn我一打开网页就是瑞星安全网站导航,怎么修改?