www.elsevier.com/locate/breast
168post 时间:2021-04-09 阅读:()
THEBREASTREVIEWObesityandbreastcancer:areviewoftheliteratureA.
R.
Carmichaela,*,T.
BatesbaThePrincessRoyalHospital,HaywardsHeath,Sussex,UKbTheBreastUnit,WilliamHarveyHospital,Ashford,Kent,UKReceived24October2002;receivedinrevisedform10March2003;accepted20March2003SummaryAwoman'sbuild,theriskofbreastcanceranditssubsequentprognosisseemtoberelated.
Inmostbutnotallcase–controlandprospectivecohortstudies,aninverserelationshiphasbeenfoundbetweenweightandbreastcanceramongpremenopausalwomen.
However,mostlargeepidemiologicalstudieshavefoundthatoverweightorobesewomenareatincreasedriskofdevelopingpostmenopausalbreastcancer.
Itissuggestedthathigherbodymassindexisassociatedwithamoreadvancedstageofbreastcanceratdiagnosisintermsoftumoursizebutdataonlymphnodestatusisnotsoconsistent.
Alltreatmentmodalitiesforbreastcancersuchassurgery,radiotherapy,chemotherapyandhormonaltreatmentmaybeadverselyaffectedbythepresenceofobesity.
Theoverallanddisease-freesurvivalisworseinmostbutnotallstudiesofprognosisofobesepre-andpostmenopausalwomenwithbreastcancer.
&2003ElsevierLtd.
Allrightsreserved.
IntroductionObesitywhichmightbeconsideredasthemalnu-tritionofthedevelopedworld,hasreachedendemicproportionsanditsprevalencecontinuestoincrease,particularlyintheafuentcountriesofEuropeandtheUnitedStates.
1InEurope,itisestimatedthat10–20%ofallmenand15–25%ofallwomenareobese.
EpidemiologicalsurveysofEnglandindicatethattheprevalenceofobesityhasalmosttripledbetween1980and1998,from6%to17%inmenandfrom8%to21%inwomenbetween16and64yearsofage(Fig.
1).
2Thisincreaseinobesityisseeninallagegroupsandhasoccurredsorapidlythatenvironmentalfactorsarethoughttoberesponsibleratherthanageneticcause.
Paradoxically,therehasbeena20%decreaseintheconsumptionofcaloriessince1970,whichmaybepartlyexplainedbyadecreaseinexpendi-tureofcaloriesduetodeclineinphysicalactivity.
3DenitionObesitycanbemeasuredasbodyweight,bodyweightrelativetoheightormaybeassessedbythedistributionoffatinthebody.
Bodymassindex(BMI)(weightinkg/heightinm2)orthetypeofobesitybythecentralorperipheraldistributionoffataretwomostwidelyusedandclinicallyARTICLEINPRESSKEYWORDSBreastneoplasms;Incidence;Bodymassindex;Diagnosis;Female;Human;Incidence;Middleage;Mortality;Postmenopausal;Premenopausal*Correspondingauthor.
RussellsHallHospital,Dudley,WestMidlandsDYI2HQ,UK.
E-mailaddress:homepac@doctors.
org.
uk(A.
R.
Carmichael).
0960-9776/$-seefrontmatter&2003ElsevierLtd.
Allrightsreserved.
doi:10.
1016/j.
breast.
2003.
03.
001TheBreast(2004)13,85–92relevantclassicationstoassessthedegreeofobesity(Table1).
4TypesofobesityCentralobesityisdenedasawaisthipratio(WHR)equaltoorgreaterthan0.
95inmenand0.
80inwomen.
Thedistributionoffatisindependentlyrelatedtothehealthrisksassociatedwithobesityi.
e.
coronaryheartdiseaseismorecommoninpatientswithcentralobesity.
5Skin-foldthicknessonthetrunkandextremities,computedtomogra-phyandmagneticresonanceimaginghaveallbeenusedtomeasurethedegreeandtypeofobesity.
ObesityandtheincidenceofbreastcancerTherelationshipbetweenbreastcancerandobesityisnotstraightforward.
PremenopausalwomenInmostbutnotallcase–controlandprospectivecohortstudies,aninverserelationshiphasbeenfoundbetweenweightandbreastcanceramongpremenopausalwomen6–11(Table2).
Ameta-analysisofsomeofthesestudiesreachedtheconclusionthatinpremenopausalwomenthereisasignicanttrendforadecreasedrelativerisk(RR)forbreastcancerinassociationwithincreasingBMI.
12Thisincreasedincidenceofbreastcancerinleanyoungwomenisfoundtobestrongestamongsttheyoungestagegroup(p35years)andisconsistentregardlessofbreastcancerratesinthecountryofresidence,weightatthetimeofdiagnosis,adolescenceorchildhood.
13Insomeepidemiologicalstudiestheexcessincidenceofbreastcanceramongleanwomeninthisagegroupislimitedtotumoursthatarelessthan2.
0cmindiameter,arenotassociatedwithmetastasestolymphnodes,andarewelldifferentiated.
14Thesendingssuggestthattheapparentexcessriskofbreastcanceramongleanpremenopausalwomenmayresultatleastinpartfromeasier,andthusearlier,diagnosisoflessaggressivetumours.
However,ahighBMIissignicantlyassociatedwithanincreasedriskofinammatorybreastcancer(IBC),whichisthemostlethalformofbreastcancerinbothpremenopausalandpost-menopausalwomen.
15Inastudyof68womenwithIBCtreatedattheM.
D.
Anderson,womeninthehighestBMItertile(BMI426.
65kg/m2)relativetothelowesttertile(BMIo22.
27)hadasignicantlyincreasedriskofIBC(IBCvs.
non-IBC,oddsratio[OR]:2.
45,95%condenceinterval[CI]:1.
05–5.
73;IBCvs.
non-breastcancer,OR:4.
52,95%CI:1.
85–11.
04).
Thisassociationwasnotsignicantlymodiedbymenopausalstatus.
15Apopulation-basedcase–controlstudyconductedinNewMexicoofHispanic(n694)andnon-Hispanic(n813)whitewomenfoundthatweightchangefromageARTICLEINPRESSFigure1Obesity(BMI30–39.
9)rateinEnglandamongmenandwomenbetween16to64yearsofage1980–1998(HealthSurveyforEngland1998).
2Table1Degreeofoverweightandobesity.
GradeBMIDescriptionUngradedBMIo20UnderweightGrade0BMI20–24.
9DesirableweightGrade1BMI25–29.
9OverweightGrade2BMI30–39.
9ObeseGrade3BMIX40MorbidlyobeseAdaptedfromWHOTechnicalReportSeriesno.
854.
486A.
R.
Carmichael,T.
Bates18tousualadultweightwasassociatedwithincreasedriskofbreastcanceramongHispanics(4thquartilevs.
baseline,OR:2.
41;95%CI:1.
45–4.
03)withnosubstantialvariationbymenopausalstatus.
Increasedriskfromweightgainwaslargelyrestrictedtowomenwhowereleanatage18andthosehormonereceptorpositivetumours.
16Somedatasuggestthatadultweightgainandcentralobesityincreasetheriskofpremenopausalbreastcancer.
13,14,17,18Astudyof216pre-andpostmenopausalwomenwithinvasivebreastcarci-nomashowedthattheRRofbreastcancerincreaseswithincreasingWHR(lessthan0.
731.
00;0.
73–761.
90;0.
77–0.
802.
83;greaterthan0.
806.
46).
18PostmenopausalwomenMostlargeepidemiologicalstudieshavefoundthatoverweightorobesewomenareatincreasedriskofdevelopingpostmenopausalbreastcancer(Table3).
6,19–25TheRRofdevelopingpostmeno-pausalbreastcancerwasfoundtobe1.
26(95%CI:1.
09,1.
46)inwomenwithBMIof28kg/m2oraboveonanalysisofpooleddatafromsevenprospectivecohortstudiesincluding337819womenand4385incidentinvasivebreastcancercases.
10Adultweightgainisanestablishedriskfactorforbreastcancerinpostmenopausalwomen.
6,26,27Inapopulation-basedcase–controlstudyinallofSwe-den,whichincluded3345(84%ofalleligible)womenaged50–74yearswithinvasivebreastcancer,and3454(82%ofallselected)controlsofsimilarage,womenwhohadgained30kgormoresinceage18hadanoddsratioof2.
04(95%CI:1.
20–3.
48)ofbreastcancercomparedwiththosewhohadmaintainedtheirweightunchanged.
Theeffectofweightgainwasunequivocalamongnon-usersbutnotamongusersofhormonereplacementtherapy.
Theexactmechanismforthisincreasedriskofbreastcancerinobesewomenisnotfullyunder-stoodbutitisthoughtthatthisisafunctionoflifetimeexposuretooestrogen,sincetheoestrogenmilieuisimportantintheinitiationandprogressionofbreastcancerlesions.
Oestrogenandperhaps,progesteroneaffecttherateofcelldivisionwhichcausesproliferationofbreastepithelialcells.
ProliferatingcellsaresusceptibletogeneticerrorsduringDNAreplicationwhich,ifuncorrected,canultimatelyleadtomalignantphenotype.
28Inpostmenopausalwomen,themainsourceofoestrogenisfromtheconversionofandrogenprecursorandrostenedioneintheperiph-eraladipocytestooestrogen;thegreatertheamountofadiposetissue,thegreatertheconver-sionandhencethegreatertheexposureofbreastcellstooestrogen.
29Thiscouldexplainthelowerincidenceofbreastcancerinpre-menopausalobesewomen,asfrequentanovulatorycyclesinthesewomenmayreducetheiroverallexposuretooestrogen.
Obesityisassociatedwithlowerlevelsofsexhormonebindingglobulins(SHBG),whichincreasethebioavailabilityofoestrogeninpostmenopausalobesewomen.
20,30Insulinresistanceiscommoninobesewomenandisassociatedwithhyper-insulinaemia.
Insulincanstimulatemammaryepitheliuminvitroviatheeffectsofinsulinlikegrowthfactor1(IGF1)whichhasasynergisticeffectwithoestrogeninpromotingmammarycarcinogenesis.
29,31–36Analternativehypothesissuggeststhatobesityisassociatedwithearlyageofmenarche,lateageofmenopauseandinfertility,whichmaximisethenumberofovulatorycycles,thisincreasesthelifetimecumulativeexposureofmammaryepitheliumtooestrogenwhichincreasestheriskofbreastcancer.
37–40However,inlargerstudiestheassociationbetweenobesityandbreastcancerpersistsevenafteradjustmentforthesefactorsarguingagainsttheprepositionthatthesereproductivepathwaysareinthecausalpathway.
39ARTICLEINPRESSTable2RelativeriskestimatesforpremenopausalbreastcancerbyBMI.
Author(year)AgeCases/controlsBMIRR(CI)London8(1989)30–55658/115534o211.
04290.
6(0.
4,0.
8)Vatten11(1992)20–49164/25336o221.
04270.
6(0.
5,0.
8)Huang6(1997)30–552517/95256o201.
04310.
62(0.
45,0.
86)Obesityandbreastcancer:areviewoftheliterature87ObesityandthediagnosisofbreastcancerItissuggestedthathigherBMIisassociatedwithamoreadvancedstageofbreastcanceratdiagno-sis.
41Astudyofnewlydiagnosedbreastcancercases(n966)inBaltimorefrom1991to1997foundthatwomenwhowereobese(BMIX27.
3)weremorelikelytobeatanadvancedstage(morethan2cmindiameter)atdiagnosiscomparedwithwomenwithaBMIofo27.
3(OR:1.
57,95%CI:1.
15–2.
14).
TheassociationbetweenBMIandstageatdiagnosiswasstrongeramongwomenyoungerthan50years(OR:2.
34,95%CI:1.
34–4.
08)comparedwithwomen50yearsorolder(OR:1.
30,95%CI:0.
89–1.
91).
42Astudyof1361newlydiagnosedbreastcancerrevealedthatoddsoflate-stagedisease(denedasmorethan2cmindiameterandnodepositive)wereincreasedwithhigherBMI(ORforhighesttolowesttertile1.
46,95%CI:1.
10–1.
93)andlargerbracupsize(ORforcupDvs.
cupA1.
61,95%CI:1.
04–2.
48).
Theserelationshipswerenotmodiedbythemethodofdiagnosiswhetherbyclinicalexaminationorscreendetection.
43However,presenceofconfoundingfactorsmightcontributetothedelayinpresenta-tionofbreastcancerinobesepatients,suchaswomenfromlowersocio-economicstatusaremorelikelytobeobeseandalsomorelikelytopresentlate.
1,44–47Moststudieshavefoundapositiveassociationbetweentumoursizeandobesitybutdataonlymphnodestatusisnotsoconsistent.
Astudyof176node-positivebreastcancerpatientsdemonstratedanindependentassociationbetweenmetastasisandprimaryratio(M/P)andobesity(P0.
0002)suggestingthatobesityisassociatedwithearlyaxillary37metastasesfromprimarytumourandARTICLEINPRESSTable3RelativeriskestimatesforpostmenopausalbreastcancerbyBMI.
Author(year)AgeCases/controlsBMIRR(CI)London8(1989)30–55420/115534o211.
04291.
0(0.
8,1.
5)Tretli24(1989)7000/5700001g/cm1.
1(0.
7,0.
9)Folsom20(1990)55–69229/1839o24.
41.
0428.
351.
1(0.
8,1.
5)Sellers25(1992)55–69493/37105Nofamilyhistoryo22.
91.
027.
5–30.
71.
3(1.
0,1.
8)430.
71.
5(1.
1,2.
1)Positivefamilyhistoryo22.
91.
027.
5–30.
71.
7(0.
9,2.
9)430.
72.
2(1.
4,3.
6)Tornberg22(1994)4551466/47003o221X281.
13(1.
01,1.
10)Huang6(1997)30–552517/95256o201.
028.
1–311.
24(0.
97,1.
59)4311.
13(0.
87,1.
46)Li21(1999)50–64479/435p21.
51X27.
61.
5(1.
1,2.
3)VandenBrandt10(2000)X504385/337819o211X281.
26(1.
09,1.
46)Morimoto23(2002)50–791030/85917p22.
61431.
12.
52(1.
6–3.
9)88A.
R.
Carmichael,T.
Batesmorerapidgrowthofmetastases.
Thishypothesisissupportedbyastudyof248womenwithbreastcancerswhichdemonstratedthatobesepostmeno-pausalwomentendtohavemoreaxillarynodeinvolvementthantheirleanercounterparts(P0.
001).
17Obesityisreportedtobeassociatedwithanincreasedincidenceofhormonereceptorpositivetumoursinsomestudieswhileotherssuggestanincreaseofhormonereceptornegativetumours.
48–50Thisdiscrepancymaybeexplainedbydifferencesinlaboratorytechniquesorcriteriaforhormoneresponsiveness.
Itisalsoreportedthatobesityisastatisticallysignicantdeterminantofpatient-relateddelayinthediagnosisofbreastcancer.
Obesewomenaretwiceaslikelytopresenttoahealth-careprofes-sionalmorethan3monthsafterrstnoticingthesymptoms.
51Itispostulatedthatobesewomenaremorelikelytohavebigbreastsandabreastlumpmaybelessobviouswhichwouldleadtoadelayinseekingmedicalattention.
Alternatively,presenceofconfoundingfactorssuchasincreasedprepon-deranceofobesityinthelowersocio-economicclasses,bothofwhichisassociatedwithdelayindiagnosisofbreastcancer.
1,44–47ObesityandthetreatmentofbreastcancerThetreatmentofbreastcancercomprisessurgery,radiotherapy,chemotherapyandhormonaltreat-ment.
Allthesetreatmentmodalitiesmaybeadverselyaffectedbythepresenceofobesity.
Obesityandloco-regionalsurgeryABMIof30ormoreisanindependentprognosticfactorfortheriskofsurgicalinfectioninpatientswithbreastcancer.
52,53Axillarysurgeryistechni-callymorechallenginginobesewomenandisshowntobeassociatedwithanincreasedincidenceofaxillarydrainageandlymphoedema,especiallyifaxillarysurgeryisfollowedbyinfection.
54,55Ax-illarysurgeryinobesepatientsisassociatedwithanincreasedincidenceofradiotherapy-relatedlong-termcomplications,whichincludelymphoedema,reductioninshouldermobilityandbrachialplexo-pathy.
56EarlyresultsfromtheAxillaryLymphaticMappingAndNodalAxillaryClearance(ALMANAC)studyandothersentinelnodebiopsystudiessuggestthatobesityisanindependentpredictoroffailureoflessinvasiveaxillaryproceduressuchassentinelnodebiopsy.
57ObesityandradiotherapyThereisclearevidencethatthelargebreastwhichiscommoninobesewomenisassociatedwithtechnicaldifcultiesinprovidinganadequatedosetowholeofthebreast.
Someauthorshavesuggestedtheuseofmoreaggressivesurgicaltechniquessuchasreductionmammoplastyinobesewomentoachieveadequateoncologicaltreatment.
58Theincidenceofradiotherapy-relatedcomplicationsishigherinobesepatients.
ObesityandchemotherapyChemotherapyisassociatedwithadecreasedincidenceofamenorrhoeainobesewomencom-paredtotheirleancounterparts(71%vs.
80%).
59Itissuggestedthatoestrogenproductioncontinuesinobesepostmenopausalwomenduetoaromatisationintheperipheraladiposetissuewhichwouldcompromiseanyindirectadvantageofchemother-apyduetochemicallyinducedmenopauseparticu-larlyinpatientswithoestrogenreceptorpositivetumours.
Whenthebloodleukocytenadirisusedasasurrogatemarkerforthedrugeffect,obesepatientswhoreceiveintravenouscyclophospha-midemethotrexateand5-uorouracilhavelesssevereleukocytenadirsthantheleanpatientswhichsuggeststhatwhentheobesearetreatedaccordingtostandardschedulestheymaybesignicantlyunder-dosed.
60Furthermore,obesepatientsmaybegivenalowerdoseofchemother-apyinordertoavoidtoxicity,whichwouldcontributetowardsapoorerprognosis.
61ObesityandtheprognosisofbreastcancerTheoverallanddisease-freesurvivalisworseinmostbutnotallstudiesofprognosisofobesepre-andpostmenopausalwomenwithbreastcancer.
Thiseffectisapparentafteradjustmentforstageatdiagnosisandtheadequacytreatmentandmaybepartlyduetodelayeddetectionandmorerapidgrowthofmetastatictissueduetoimpairedcellularimmunityandhigheroestrogenlevels.
62–66TheAmericanCancerSociety'sCancerPreven-tionStudyII(CPS-II),aprospectivemortalitystudywhichincluded424168postmenopausalwomenand2852breastcancerdeathsfoundatfollow-upof14yearsthatbreastcancermortalityratesincreasedcontinuallyandsubstantiallywithin-creasingBMI(RR:3.
08,95%CI:2.
09–4.
51forBMI440.
0comparedtoBMI18.
5–20.
49).
Ifcausal,ARTICLEINPRESSObesityandbreastcancer:areviewoftheliterature89themultivariate-adjustedRRestimatesinthisstudycorrespondtoapproximately30–50%ofbreastcancerdeathsamongpostmenopausalwo-menintheUSpopulationbeingattributabletooverweight.
67Astudyof735node-positivepatientsfoundatamedianfollow-upof10.
7years,the10-year,disease-freeratefornon-obesepatientswas54%(95%CI:50–58%)comparedwith40%(CI:33–47%)forpatientsclassiedasobese.
Althoughobesepatientstendedtohavesomewhatlessfavourableoutcomebasedonstandardprognosticcriteria,aproportional-hazardsregressionmodeladjustingforotherfactorsindicatedthatriskfordiseaserecurrenceamongobesepatientswas1.
33timesthatofthenon-obesepopulation(CI:1.
05–1.
68).
68Thenegativeeffectofobesityonbreastcancersurvivalhasalsobeendemonstratedinseveralsmall-scalestudies.
Astudyof213womenwithbreastcancerfoundthattheestimatedsurvivalprobabilityforwomenwithBMIof20wasabout12%higherthanthosewithBMIof24,overa10-yearfollow-up.
69Theprognosisofbreastcancerwaspoorinbothpremenopausalandpostmeno-pausalobesewomen.
70Premenopausalobesewo-menhadupto70%decreasedsurvivalandrecurrence-freeintervalofbreastcancerafteradjustmentforstageatdiagnosisandtreat-ment.
65,71Ameta-analysisof8029womenfoundthatBMIhadaprognosticsignicanceinbreastcancer,hazardratio1.
56(95%CI:1.
22–2.
00).
However,thiseffectwasfoundtobeheteroge-neousandsomestudieshavereportednoadversesurvivaleffectofhighBMI.
7,72–77ThesedifferencesinreportedsurvivalinbreastcancerpatientswithhighBMIcanpartlybeexplainedbytheuseofdifferingdenitionsofobesitybyvariousstudiesandthefactthatsomestudieshaveanalysedthedataforoverweightandobesepatientstogether.
However,thepossibilityofpublicationbiasagainstnegativestudiesshouldnotbedismissed.
Thereisindirectevidencethatpoorsurvivalinwomenwithbreastcancerinlowersocio-economicclassesmaybepartlyexplainedbythegreaterincidenceofobesityinlowersocialclasses.
30,45,47,78,79Thehostfactorssuchascellularimmunityandnutritionthatmaydeterminemetas-tasesandrecurrenceofbreastcancermaybeunfavourableindeprivedobesepatientsoflowersocio-economicstatus.
45,80Itisalsosuggestedthatwomenfromlowersocio-economicclassestendtohavepooraccessandutilisationofthediagnosticandtherapeuticsupportforbreastcancer.
81Insummary,consistent,independentandpositiveassociationhasbeenfoundbetweenobesityandbreastcancerinpostmenopausalwomen,andinthemajorityoftheliteraturebetweenobesityandpoorprognosisofbreastcancerinbothpre-andpostmenopausalwomen.
Theattributable-riskes-timatesduetoobesityarecomparabletothoseduetoapositivefamilyhistory(6–19%).
70,82Itissuggestedthatreductionofobesitycandecreasethecasesofbreastcancerbyone-tenthinEuropewithaconsequentreductioninmortality.
83Despiteadecreaseinmortalityfrombreastcancerinrecentyears,breastcancerkills12000womenayearintheUnitedKingdomalone,andtensofthousandsinEurope.
Itisfearedthatincreasingobesityinwomenwillmanifestitseffectofincreasedincidenceofbreastcancerinpostmeno-pausalwomeninthecomingyears.
Sinceobesityisoneofthefewriskfactorsforbreastcancerwhichcanbemodiedthroughoutlife,84apublichealthpolicy,planningandhealtheducationcampaignareurgentlyrequiredtoaddresstherisingproblemsofobesityandbreastcancer.
AcknowledgementsIamgratefulforthehelpofthestaffoftheRosewellLibrary,ConquestHospital,St.
Leonard-on-Sea.
References1.
SeidellJC.
Timetrendsinobesity:anepidemiologicalperspective.
HormMetabRes1997;29(4):155–8.
2.
HMSO.
HealthSurveysofEngland:cardiovasculardisease.
London.
HMSO,1998.
3.
PrenticeA,JebbSA.
ObesityinBritain:gluttonyorsloth.
BMJ1995;311(7002):4379.
4.
WorldHealthOrganisation.
MeasuringobesityFclassica-tionanddescriptionofanthropometricdata.
Copenhagen;WHO:1989.
5.
HanTS,vanLeerEM,SeidellJC,LeanME.
Waistcircumfer-enceactionlevelsintheidenticationofcardiovascularriskfactors:prevalencestudyinarandomsample.
BMJ1995;311(7017):14015.
6.
HuangZ,HankinsonSE,ColditzGA,etal.
Dualeffectsofweightandweightgainonbreastcancerrisk.
JAMA1997;278(17):140711.
7.
KatohA,WatzlafVJ,D'AmicoF.
Anexaminationofobesityandbreastcancersurvivalinpost-menopausalwomen.
BrJCancer1994;70(5):92833.
8.
LondonSJ,ColditzGA,StampferMJ,etal.
Prospectivestudyofrelativeweight,height,andriskofbreastcancer.
JAMA1989;262(20):28538.
9.
PathakDR,WhittemoreAS.
Combinedeffectsofbodysize,parity,andmenstrualeventsonbreastcancerincidenceinsevencountries.
AmJEpidemiol1992;135(2):15368.
10.
vandenBrandtPA,SpiegelmanD,YaunSS,etal.
Pooledanalysisofprospectivecohortstudiesonheight,weight,andbreastcancerrisk.
AmJEpidemiol2000;152(6):51427.
11.
VattenLJ,KvinnslandS.
Prospectivestudyofheight,bodymassindexandriskofbreastcancer.
ActaOncol1992;31(2):195200.
ARTICLEINPRESS90A.
R.
Carmichael,T.
Bates12.
UrsinG,LongneckerMP,HaileRW,GreenlandS.
Ameta-analysisofbodymassindexandriskofpremenopausalbreastcancer.
Epidemiology1995;6(2):13741.
13.
PeacockSL,WhiteE,DalingJR,VoigtLF,MaloneKE.
Relationbetweenobesityandbreastcancerinyoungwomen.
AmJEpidemiol1999;149(4):33946.
14.
WillettWC,BrowneML,BainC,etal.
Relativeweightandriskofbreastcanceramongpremenopausalwomen.
AmJEpidemiol1985;122(5):73140.
15.
ChangS,BuzdarAU,HurstingSD.
Inammatorybreastcancerandbodymassindex.
JClinOncol1998;16(12):37315.
16.
WentenM,GillilandFD,BaumgartnerK,SametJM.
Associa-tionsofweight,weightchange,andbodymasswithbreastcancerriskinHispanicandnon-Hispanicwhitewomen.
AnnEpidemiol2002;12(6):4354417.
SchapiraDV,KumarNB,LymanGH,CoxCE.
Obesityandbodyfatdistributionandbreastcancerprognosis.
Cancer1991;67(2):5238.
18.
SchapiraDV,KumarNB,LymanGH,CoxCE.
Abdominalobesityandbreastcancerrisk.
AnnInternMed1990;112(3):1826.
19.
Ballard-BarbashR.
Anthropometryandbreastcancer.
BodysizeFamovingtarget.
Cancer1994;74(3Suppl):1090100.
20.
FolsomAR,KayeSA,PrineasRJ,etal.
Increasedincidenceofcarcinomaofthebreastassociatedwithabdominaladiposityinpostmenopausalwomen.
AmJEpidemiol1990;131(5):794803.
21.
LiCl,StanfordJL,DalingJR.
Anthropometricvariablesinrelationtoriskofbreastcancerinmiddle-agedwomen.
IntJEpidemiol2000;29(2):20813.
22.
TornbergSA,CarstensenJM.
RelationshipbetweenQuete-let'sindexandcancerofbreastandfemalegenitaltractin47,000womenfollowedfor25years.
BrJCancer1994;69(2):35861.
23.
MorimotoLM,WhiteE,ChenZ,etal.
Obesity,bodysize,andriskofpostmenopausalbreastcancer:theWomen'sHealthInitiative(UnitedStates).
CancerCausesControl2002;13:74151.
24.
TretliS.
Heightandweightinrelationtobreastcancermortalityandmorbidity:aprospectivestudyof570,000womeninNorway.
IntJCancer1989;44:2330.
25.
SellersTA,KushiLH,PotterJD,etal.
Effectoffamilyhistory,body-fatdistribution,andreproductivefactorsontheriskofpostmenopausalbreastcancer.
NEnglJMed1992;326(20):13239.
26.
WillettWC.
Whoissusceptibletocancerofthebreast,colonandprostateAnnNYAcadSci1995;768:111.
27.
MagnussonC,BaronJ,PerssonI,etal.
Bodysizeindifferentperiodsoflifeandbreastcancerriskinpost-menopausalwomen.
IntJCancer1998;76(1):2934.
28.
LaGuardiaM,GiammancoM.
Breastcancerandobesity.
PanminervaMed2001;43(2):12333.
29.
StollBA.
Adiposityasariskdeterminantforpostmenopausalbreastcancer.
IntJObesRelatMetabDisord2000;24(5):52733.
30.
StollBA.
Obesityandbreastcancer.
IntJObesRelatMetabDisord1996;20(5):38992.
31.
KalekoM,RutterWJ,MillerAD.
OverexpressionofthehumaninsulinlikegrowthfactorIreceptorpromotesligand-dependentneoplastictransformation.
MolCellBiol1990;10(2):46473.
32.
MacaulayVM.
Insulin-likegrowthfactorsandcancer.
BrJCancer1992;65(3):31120.
33.
PollakMN,PolychronakosC,YouseS,RichardM.
Char-acterizationofinsulin-likegrowthfactorI(IGF-I)receptorsofhumanbreastcancercells.
BiochemBiophysResCommun1988;154(1):32631.
34.
ReavenGM.
SyndromeX.
BloodPressSuppl1992;4:136.
35.
StollBA.
Breastcancer:theobesityconnection.
BrJCancer1994;69(5):799801.
36.
StollBA.
Nutritionandbreastcancerrisk:cananeffectviainsulinresistancebedemonstratedBreastCancerResTreat1996;38(3):23946.
37.
DaniellHW,TamE,FiliceA.
LargeraxillarymetastasesinobesewomenandsmokerswithbreastcancerFaninuencebyhostfactorsonearlytumorbehavior.
BreastCancerResTreat1993;25(3):193201.
38.
FriedenreichCM,RohanTE.
Physicalactivityandriskofbreastcancer.
EurJCancerPrev1995;4(2):14551.
39.
KorzeniowskiS,DybaT.
Reproductivehistoryandprognosisinpatientswithoperablebreastcancer.
Cancer1994;74(5):15914.
40.
MerzenichH,BoeingH,WahrendorfJ.
Dietaryfatandsportsactivityasdeterminantsforageatmenarche.
AmJEpidemiol1993;138(4):21724.
41.
MaehleBO,TretliS,SkjaervenR,ThorsenT.
Premorbidbodyweightanditsrelationstoprimarytumourdiameterinbreastcancerpatients;itsdependenceonestrogenandprogesteronreceptorstatus.
BreastCancerResTreat2001;68(2):15969.
42.
CuiY,WhitemanMK,FlawsJA,etal.
Bodymassandstageofbreastcanceratdiagnosis.
IntJCancer2002;98(2):27983.
43.
HallHI,CoatesRJ,UhlerRJ,etal.
Stageofbreastcancerinrelationtobodymassindexandbracupsize.
IntJCancer1999;82(1):237.
44.
RichardsonJL,LangholzB,BernsteinL,etal.
Stageanddelayinbreastcancerdiagnosisbyrace,socioeconomicstatus,ageandyear.
BrJCancer1992;65(6):9226.
45.
SchrijversCT,MackenbachJP,LutzJM,QuinnMJ,ColemanMP.
Deprivationandsurvivalfrombreastcancer.
BrJCancer1995;72(3):73843.
46.
StollBA.
Obesity,socialclassandWesterndiet:alinktobreastcancerprognosis.
EurJCancer1996;32A(8):12935.
47.
TorgersonD.
Riskfactorsforbreastcancer.
Socioeconomicdifferencesmightbeexplainedbybodymass.
BMJ1994;309(6969):1662.
48.
ClearyMP,MaihleNJ.
Theroleofbodymassindexintherelativeriskofdevelopingpremenopausalversuspostmeno-pausalbreastcancer.
ProcSocExpBiolMed1997;216(1):2843.
49.
GiuffridaD,LupoL,LaPortaGA,etal.
Relationbetweensteroidreceptorstatusandbodyweightinbreastcancerpatients.
EurJCancer1992;28(1):1125.
50.
MaehleBO,TretliS.
Pre-morbidbody-mass-indexinbreastcancer:reversedeffectonsurvivalinhormonereceptornegativepatients.
BreastCancerResTreat1996;41(2):12330.
51.
ArndtV,SturmerT,StegmaierC,etal.
PatientdelayandstageofdiagnosisamongbreastcancerpatientsinGerma-nyFapopulationbasedstudy.
BrJCancer2002;86(7):103440.
52.
BertinML,CroweJ,GordonSM.
Determinantsofsurgicalsiteinfectionafterbreastsurgery.
AmJInfectControl1998;26(1):615.
53.
VintonAL,TraversoLW,JollyPC.
Woundcomplicationsaftermodiedradicalmastectomycomparedwithtylectomywithaxillarylymphnodedissection.
AmJSurg1991;161(5):5848.
54.
BanerjeeD,WilliamsEV,IlottJ,MonypennyIJ,WebsterDJ.
ObesitypredisposestoincreaseddrainagefollowingaxillaryARTICLEINPRESSObesityandbreastcancer:areviewoftheliterature91nodeclearance:aprospectiveaudit.
AnnRCollSurgEngl2001;83(4):26871.
55.
WernerRS,McCormickB,PetrekJ,etal.
Armedemainconservativelymanagedbreastcancer:obesityisamajorpredictivefactor.
Radiology1991;180(1):17784.
56.
BentzenSM,DischeS.
Morbidityrelatedtoaxillaryirradia-tioninthetreatmentofbreastcancer.
ActaOncol2000;39(3):33747.
57.
AhrendtGM,LaudP,TjoeJ,etal.
DoesbreasttumorlocationinuencesuccessofsentinellymphnodebiopsyJAmCollSurg2002;194(3):27884.
58.
NewmanLA,KuererHM,McNeeseMD,etal.
Reductionmammoplastyimprovesbreastconservationtherapyinpatientswithmacromastia.
AmJSurg2001;181(3):21520.
59.
MehtaRR,BeattieCW,GuptaTK.
Endocrineproleinbreastcancerpatientsreceivingchemotherapy.
BreastCancerResTreat1991;20:12532.
60.
PoikonenP,BlomqvistC,JoensuuH.
Effectofobesityontheleukocytenadirinwomentreatedwithadjuvantcyclopho-sphamide,methotrexate,anduorouracildosedaccordingtobodysurfacearea.
ActaOncol2001;40(1):6771.
61.
RosnerGL,HargisJB,HollisDR,etal.
Relationshipbetweentoxicityandobesityinwomenreceivingadjuvantchemo-therapyforbreastcancer:resultsfromcancerandleukemiagroupBstudy8541.
JClinOncol1996;14(11):30008.
62.
NewmanSC,MillerAB,HoweGR.
Astudyoftheeffectofweightanddietaryfatonbreastcancersurvivaltime.
AmJEpidemiol1986;123(5):76774.
63.
SenieRT,RosenPP,RhodesP,LesserML,KinneDW.
Obesityatdiagnosisofbreastcarcinomainuencesdurationofdisease-freesurvival.
AnnInternMed1992;116(1):2632.
64.
TornbergS,CarstensenJ.
Serumbeta-lipoprotein,serumcholesterolandQuetelet'sindexaspredictorsforsurvivalofbreastcancerpatients.
EurJCancer1993;29A(14):202530.
65.
TretliS,HaldorsenT,OttestadL.
Theeffectofpre-morbidheightandweightonthesurvivalofbreastcancerpatients.
BrJCancer1990;62(2):299303.
66.
ZhangS,FolsomAR,SellersTA,KushiLH,PotterJD.
Betterbreastcancersurvivalforpostmenopausalwomenwhoarelessoverweightandeatlessfat.
TheIowaWomen'sHealthStudy.
Cancer1995;76(2):27583.
67.
PetrelliJM,CalleEE,RodriguezC,ThunMJ.
Bodymassindex,height,andpostmenopausalbreastcancermortalityinaprospectivecohortofUSwomen.
CancerCausesControl2002;13(4):32532.
68.
BastarracheaJ,HortobagyiGN,SmithTL,KauSW,BuzdarAU.
Obesityasanadverseprognosticfactorforpatientsreceivingadjuvantchemotherapyforbreastcancer.
AnnInternMed1994;120(1):1825.
69.
KyogokuS,HirohataT,TakeshitaS,etal.
Survivalofbreast-cancerpatientsandbodysizeindicators.
IntJCancer1990;46(5):82431.
70.
Ballard-BarbashR,SwansonCA.
Bodyweight:estimationofriskforbreastandendometrialcancers.
AmJClinNutr1996;63(3Suppl):437S41S.
71.
Demark-WahnefriedW,WinerEP,RimerBK.
Whywomengainweightwithadjuvantchemotherapyforbreastcancer.
JClinOncol1993;11(7):141829.
72.
GreenbergER,VesseyMP,McPhersonK,DollR,YeatesD.
Bodysizeandsurvivalinpremenopausalbreastcancer.
BrJCancer1985;51(5):6917.
73.
JainM,MillerAB.
Pre-morbidbodysizeandtheprognosisofwomenwithbreastcancer.
IntJCancer1994;59(3):3638.
74.
MarretH,PerrotinF,BougnouxP,etal.
Lowbodymassindexisanindependentpredictivefactoroflocalrecurrenceafterconservativetreatmentforbreastcancer.
BreastCancerResTreat2001;66(1):1723.
75.
MenonKV,HodgeA,HoughtonJ,BatesT.
Bodymassindex,heightandcumulativemenstrualcycleatthetimeofdiagnosisarenotriskfactorsforpooroutcomeinbreastcancer.
Breast1999;8:32833.
76.
ObermairA,KurzC,HanzalE,etal.
Theinuenceofobesityonthedisease-freesurvivalinprimarybreastcancer.
AnticancerRes1995;15(5B):22659.
77.
SohrabiA,SandozJ,SprattJS,PolkJr,HC.
Recurrenceofbreastcancer.
Obesity,tumorsize,andaxillarylymphnodemetastases.
JAMA1980;244(3):2645.
78.
HaybittleJ,HoughtonJ,BaumM.
Socialclassandweightasprognosticfactorsinearlybreastcancer.
BrJCancer1997;75(5):72933.
79.
KarjalainenS,PukkalaE.
Socialclassasaprognosticfactorinbreastcancersurvival.
Cancer1990;66(4):81926.
80.
CarnonAG,SsemwogerereA,LamontDW,etal.
Relationbetweensocioeconomicdeprivationandpathologicalprog-nosticfactorsinwomenwithbreastcancer.
BMJ1994;309(6961):10547.
81.
AntmanK,Abraido-LanzaAF,BlumD,etal.
Reducingdisparitiesinbreastcancersurvival:aColumbiaUniversityandAvonBreastCancerResearchandCareNetworkSymposium.
BreastCancerResTreat2002;75:26980.
82.
HunterDJ,WillettWC.
Diet,bodysize,andbreastcancer.
EpidemiolRev1993;15(1):11032.
83.
LaVecchiaC.
Nutritionalfactorsandcancersofthebreast,endometriumandovary.
EurJCancerClinOncol1989;25(12):194551.
84.
KelseyJL,BernsteinL.
Epidemiologyandpreventionofbreastcancer.
AnnuRevPublicHealth1996;17:4767.
ARTICLEINPRESS92A.
R.
Carmichael,T.
Bates
R.
Carmichaela,*,T.
BatesbaThePrincessRoyalHospital,HaywardsHeath,Sussex,UKbTheBreastUnit,WilliamHarveyHospital,Ashford,Kent,UKReceived24October2002;receivedinrevisedform10March2003;accepted20March2003SummaryAwoman'sbuild,theriskofbreastcanceranditssubsequentprognosisseemtoberelated.
Inmostbutnotallcase–controlandprospectivecohortstudies,aninverserelationshiphasbeenfoundbetweenweightandbreastcanceramongpremenopausalwomen.
However,mostlargeepidemiologicalstudieshavefoundthatoverweightorobesewomenareatincreasedriskofdevelopingpostmenopausalbreastcancer.
Itissuggestedthathigherbodymassindexisassociatedwithamoreadvancedstageofbreastcanceratdiagnosisintermsoftumoursizebutdataonlymphnodestatusisnotsoconsistent.
Alltreatmentmodalitiesforbreastcancersuchassurgery,radiotherapy,chemotherapyandhormonaltreatmentmaybeadverselyaffectedbythepresenceofobesity.
Theoverallanddisease-freesurvivalisworseinmostbutnotallstudiesofprognosisofobesepre-andpostmenopausalwomenwithbreastcancer.
&2003ElsevierLtd.
Allrightsreserved.
IntroductionObesitywhichmightbeconsideredasthemalnu-tritionofthedevelopedworld,hasreachedendemicproportionsanditsprevalencecontinuestoincrease,particularlyintheafuentcountriesofEuropeandtheUnitedStates.
1InEurope,itisestimatedthat10–20%ofallmenand15–25%ofallwomenareobese.
EpidemiologicalsurveysofEnglandindicatethattheprevalenceofobesityhasalmosttripledbetween1980and1998,from6%to17%inmenandfrom8%to21%inwomenbetween16and64yearsofage(Fig.
1).
2Thisincreaseinobesityisseeninallagegroupsandhasoccurredsorapidlythatenvironmentalfactorsarethoughttoberesponsibleratherthanageneticcause.
Paradoxically,therehasbeena20%decreaseintheconsumptionofcaloriessince1970,whichmaybepartlyexplainedbyadecreaseinexpendi-tureofcaloriesduetodeclineinphysicalactivity.
3DenitionObesitycanbemeasuredasbodyweight,bodyweightrelativetoheightormaybeassessedbythedistributionoffatinthebody.
Bodymassindex(BMI)(weightinkg/heightinm2)orthetypeofobesitybythecentralorperipheraldistributionoffataretwomostwidelyusedandclinicallyARTICLEINPRESSKEYWORDSBreastneoplasms;Incidence;Bodymassindex;Diagnosis;Female;Human;Incidence;Middleage;Mortality;Postmenopausal;Premenopausal*Correspondingauthor.
RussellsHallHospital,Dudley,WestMidlandsDYI2HQ,UK.
E-mailaddress:homepac@doctors.
org.
uk(A.
R.
Carmichael).
0960-9776/$-seefrontmatter&2003ElsevierLtd.
Allrightsreserved.
doi:10.
1016/j.
breast.
2003.
03.
001TheBreast(2004)13,85–92relevantclassicationstoassessthedegreeofobesity(Table1).
4TypesofobesityCentralobesityisdenedasawaisthipratio(WHR)equaltoorgreaterthan0.
95inmenand0.
80inwomen.
Thedistributionoffatisindependentlyrelatedtothehealthrisksassociatedwithobesityi.
e.
coronaryheartdiseaseismorecommoninpatientswithcentralobesity.
5Skin-foldthicknessonthetrunkandextremities,computedtomogra-phyandmagneticresonanceimaginghaveallbeenusedtomeasurethedegreeandtypeofobesity.
ObesityandtheincidenceofbreastcancerTherelationshipbetweenbreastcancerandobesityisnotstraightforward.
PremenopausalwomenInmostbutnotallcase–controlandprospectivecohortstudies,aninverserelationshiphasbeenfoundbetweenweightandbreastcanceramongpremenopausalwomen6–11(Table2).
Ameta-analysisofsomeofthesestudiesreachedtheconclusionthatinpremenopausalwomenthereisasignicanttrendforadecreasedrelativerisk(RR)forbreastcancerinassociationwithincreasingBMI.
12Thisincreasedincidenceofbreastcancerinleanyoungwomenisfoundtobestrongestamongsttheyoungestagegroup(p35years)andisconsistentregardlessofbreastcancerratesinthecountryofresidence,weightatthetimeofdiagnosis,adolescenceorchildhood.
13Insomeepidemiologicalstudiestheexcessincidenceofbreastcanceramongleanwomeninthisagegroupislimitedtotumoursthatarelessthan2.
0cmindiameter,arenotassociatedwithmetastasestolymphnodes,andarewelldifferentiated.
14Thesendingssuggestthattheapparentexcessriskofbreastcanceramongleanpremenopausalwomenmayresultatleastinpartfromeasier,andthusearlier,diagnosisoflessaggressivetumours.
However,ahighBMIissignicantlyassociatedwithanincreasedriskofinammatorybreastcancer(IBC),whichisthemostlethalformofbreastcancerinbothpremenopausalandpost-menopausalwomen.
15Inastudyof68womenwithIBCtreatedattheM.
D.
Anderson,womeninthehighestBMItertile(BMI426.
65kg/m2)relativetothelowesttertile(BMIo22.
27)hadasignicantlyincreasedriskofIBC(IBCvs.
non-IBC,oddsratio[OR]:2.
45,95%condenceinterval[CI]:1.
05–5.
73;IBCvs.
non-breastcancer,OR:4.
52,95%CI:1.
85–11.
04).
Thisassociationwasnotsignicantlymodiedbymenopausalstatus.
15Apopulation-basedcase–controlstudyconductedinNewMexicoofHispanic(n694)andnon-Hispanic(n813)whitewomenfoundthatweightchangefromageARTICLEINPRESSFigure1Obesity(BMI30–39.
9)rateinEnglandamongmenandwomenbetween16to64yearsofage1980–1998(HealthSurveyforEngland1998).
2Table1Degreeofoverweightandobesity.
GradeBMIDescriptionUngradedBMIo20UnderweightGrade0BMI20–24.
9DesirableweightGrade1BMI25–29.
9OverweightGrade2BMI30–39.
9ObeseGrade3BMIX40MorbidlyobeseAdaptedfromWHOTechnicalReportSeriesno.
854.
486A.
R.
Carmichael,T.
Bates18tousualadultweightwasassociatedwithincreasedriskofbreastcanceramongHispanics(4thquartilevs.
baseline,OR:2.
41;95%CI:1.
45–4.
03)withnosubstantialvariationbymenopausalstatus.
Increasedriskfromweightgainwaslargelyrestrictedtowomenwhowereleanatage18andthosehormonereceptorpositivetumours.
16Somedatasuggestthatadultweightgainandcentralobesityincreasetheriskofpremenopausalbreastcancer.
13,14,17,18Astudyof216pre-andpostmenopausalwomenwithinvasivebreastcarci-nomashowedthattheRRofbreastcancerincreaseswithincreasingWHR(lessthan0.
731.
00;0.
73–761.
90;0.
77–0.
802.
83;greaterthan0.
806.
46).
18PostmenopausalwomenMostlargeepidemiologicalstudieshavefoundthatoverweightorobesewomenareatincreasedriskofdevelopingpostmenopausalbreastcancer(Table3).
6,19–25TheRRofdevelopingpostmeno-pausalbreastcancerwasfoundtobe1.
26(95%CI:1.
09,1.
46)inwomenwithBMIof28kg/m2oraboveonanalysisofpooleddatafromsevenprospectivecohortstudiesincluding337819womenand4385incidentinvasivebreastcancercases.
10Adultweightgainisanestablishedriskfactorforbreastcancerinpostmenopausalwomen.
6,26,27Inapopulation-basedcase–controlstudyinallofSwe-den,whichincluded3345(84%ofalleligible)womenaged50–74yearswithinvasivebreastcancer,and3454(82%ofallselected)controlsofsimilarage,womenwhohadgained30kgormoresinceage18hadanoddsratioof2.
04(95%CI:1.
20–3.
48)ofbreastcancercomparedwiththosewhohadmaintainedtheirweightunchanged.
Theeffectofweightgainwasunequivocalamongnon-usersbutnotamongusersofhormonereplacementtherapy.
Theexactmechanismforthisincreasedriskofbreastcancerinobesewomenisnotfullyunder-stoodbutitisthoughtthatthisisafunctionoflifetimeexposuretooestrogen,sincetheoestrogenmilieuisimportantintheinitiationandprogressionofbreastcancerlesions.
Oestrogenandperhaps,progesteroneaffecttherateofcelldivisionwhichcausesproliferationofbreastepithelialcells.
ProliferatingcellsaresusceptibletogeneticerrorsduringDNAreplicationwhich,ifuncorrected,canultimatelyleadtomalignantphenotype.
28Inpostmenopausalwomen,themainsourceofoestrogenisfromtheconversionofandrogenprecursorandrostenedioneintheperiph-eraladipocytestooestrogen;thegreatertheamountofadiposetissue,thegreatertheconver-sionandhencethegreatertheexposureofbreastcellstooestrogen.
29Thiscouldexplainthelowerincidenceofbreastcancerinpre-menopausalobesewomen,asfrequentanovulatorycyclesinthesewomenmayreducetheiroverallexposuretooestrogen.
Obesityisassociatedwithlowerlevelsofsexhormonebindingglobulins(SHBG),whichincreasethebioavailabilityofoestrogeninpostmenopausalobesewomen.
20,30Insulinresistanceiscommoninobesewomenandisassociatedwithhyper-insulinaemia.
Insulincanstimulatemammaryepitheliuminvitroviatheeffectsofinsulinlikegrowthfactor1(IGF1)whichhasasynergisticeffectwithoestrogeninpromotingmammarycarcinogenesis.
29,31–36Analternativehypothesissuggeststhatobesityisassociatedwithearlyageofmenarche,lateageofmenopauseandinfertility,whichmaximisethenumberofovulatorycycles,thisincreasesthelifetimecumulativeexposureofmammaryepitheliumtooestrogenwhichincreasestheriskofbreastcancer.
37–40However,inlargerstudiestheassociationbetweenobesityandbreastcancerpersistsevenafteradjustmentforthesefactorsarguingagainsttheprepositionthatthesereproductivepathwaysareinthecausalpathway.
39ARTICLEINPRESSTable2RelativeriskestimatesforpremenopausalbreastcancerbyBMI.
Author(year)AgeCases/controlsBMIRR(CI)London8(1989)30–55658/115534o211.
04290.
6(0.
4,0.
8)Vatten11(1992)20–49164/25336o221.
04270.
6(0.
5,0.
8)Huang6(1997)30–552517/95256o201.
04310.
62(0.
45,0.
86)Obesityandbreastcancer:areviewoftheliterature87ObesityandthediagnosisofbreastcancerItissuggestedthathigherBMIisassociatedwithamoreadvancedstageofbreastcanceratdiagno-sis.
41Astudyofnewlydiagnosedbreastcancercases(n966)inBaltimorefrom1991to1997foundthatwomenwhowereobese(BMIX27.
3)weremorelikelytobeatanadvancedstage(morethan2cmindiameter)atdiagnosiscomparedwithwomenwithaBMIofo27.
3(OR:1.
57,95%CI:1.
15–2.
14).
TheassociationbetweenBMIandstageatdiagnosiswasstrongeramongwomenyoungerthan50years(OR:2.
34,95%CI:1.
34–4.
08)comparedwithwomen50yearsorolder(OR:1.
30,95%CI:0.
89–1.
91).
42Astudyof1361newlydiagnosedbreastcancerrevealedthatoddsoflate-stagedisease(denedasmorethan2cmindiameterandnodepositive)wereincreasedwithhigherBMI(ORforhighesttolowesttertile1.
46,95%CI:1.
10–1.
93)andlargerbracupsize(ORforcupDvs.
cupA1.
61,95%CI:1.
04–2.
48).
Theserelationshipswerenotmodiedbythemethodofdiagnosiswhetherbyclinicalexaminationorscreendetection.
43However,presenceofconfoundingfactorsmightcontributetothedelayinpresenta-tionofbreastcancerinobesepatients,suchaswomenfromlowersocio-economicstatusaremorelikelytobeobeseandalsomorelikelytopresentlate.
1,44–47Moststudieshavefoundapositiveassociationbetweentumoursizeandobesitybutdataonlymphnodestatusisnotsoconsistent.
Astudyof176node-positivebreastcancerpatientsdemonstratedanindependentassociationbetweenmetastasisandprimaryratio(M/P)andobesity(P0.
0002)suggestingthatobesityisassociatedwithearlyaxillary37metastasesfromprimarytumourandARTICLEINPRESSTable3RelativeriskestimatesforpostmenopausalbreastcancerbyBMI.
Author(year)AgeCases/controlsBMIRR(CI)London8(1989)30–55420/115534o211.
04291.
0(0.
8,1.
5)Tretli24(1989)7000/5700001g/cm1.
1(0.
7,0.
9)Folsom20(1990)55–69229/1839o24.
41.
0428.
351.
1(0.
8,1.
5)Sellers25(1992)55–69493/37105Nofamilyhistoryo22.
91.
027.
5–30.
71.
3(1.
0,1.
8)430.
71.
5(1.
1,2.
1)Positivefamilyhistoryo22.
91.
027.
5–30.
71.
7(0.
9,2.
9)430.
72.
2(1.
4,3.
6)Tornberg22(1994)4551466/47003o221X281.
13(1.
01,1.
10)Huang6(1997)30–552517/95256o201.
028.
1–311.
24(0.
97,1.
59)4311.
13(0.
87,1.
46)Li21(1999)50–64479/435p21.
51X27.
61.
5(1.
1,2.
3)VandenBrandt10(2000)X504385/337819o211X281.
26(1.
09,1.
46)Morimoto23(2002)50–791030/85917p22.
61431.
12.
52(1.
6–3.
9)88A.
R.
Carmichael,T.
Batesmorerapidgrowthofmetastases.
Thishypothesisissupportedbyastudyof248womenwithbreastcancerswhichdemonstratedthatobesepostmeno-pausalwomentendtohavemoreaxillarynodeinvolvementthantheirleanercounterparts(P0.
001).
17Obesityisreportedtobeassociatedwithanincreasedincidenceofhormonereceptorpositivetumoursinsomestudieswhileotherssuggestanincreaseofhormonereceptornegativetumours.
48–50Thisdiscrepancymaybeexplainedbydifferencesinlaboratorytechniquesorcriteriaforhormoneresponsiveness.
Itisalsoreportedthatobesityisastatisticallysignicantdeterminantofpatient-relateddelayinthediagnosisofbreastcancer.
Obesewomenaretwiceaslikelytopresenttoahealth-careprofes-sionalmorethan3monthsafterrstnoticingthesymptoms.
51Itispostulatedthatobesewomenaremorelikelytohavebigbreastsandabreastlumpmaybelessobviouswhichwouldleadtoadelayinseekingmedicalattention.
Alternatively,presenceofconfoundingfactorssuchasincreasedprepon-deranceofobesityinthelowersocio-economicclasses,bothofwhichisassociatedwithdelayindiagnosisofbreastcancer.
1,44–47ObesityandthetreatmentofbreastcancerThetreatmentofbreastcancercomprisessurgery,radiotherapy,chemotherapyandhormonaltreat-ment.
Allthesetreatmentmodalitiesmaybeadverselyaffectedbythepresenceofobesity.
Obesityandloco-regionalsurgeryABMIof30ormoreisanindependentprognosticfactorfortheriskofsurgicalinfectioninpatientswithbreastcancer.
52,53Axillarysurgeryistechni-callymorechallenginginobesewomenandisshowntobeassociatedwithanincreasedincidenceofaxillarydrainageandlymphoedema,especiallyifaxillarysurgeryisfollowedbyinfection.
54,55Ax-illarysurgeryinobesepatientsisassociatedwithanincreasedincidenceofradiotherapy-relatedlong-termcomplications,whichincludelymphoedema,reductioninshouldermobilityandbrachialplexo-pathy.
56EarlyresultsfromtheAxillaryLymphaticMappingAndNodalAxillaryClearance(ALMANAC)studyandothersentinelnodebiopsystudiessuggestthatobesityisanindependentpredictoroffailureoflessinvasiveaxillaryproceduressuchassentinelnodebiopsy.
57ObesityandradiotherapyThereisclearevidencethatthelargebreastwhichiscommoninobesewomenisassociatedwithtechnicaldifcultiesinprovidinganadequatedosetowholeofthebreast.
Someauthorshavesuggestedtheuseofmoreaggressivesurgicaltechniquessuchasreductionmammoplastyinobesewomentoachieveadequateoncologicaltreatment.
58Theincidenceofradiotherapy-relatedcomplicationsishigherinobesepatients.
ObesityandchemotherapyChemotherapyisassociatedwithadecreasedincidenceofamenorrhoeainobesewomencom-paredtotheirleancounterparts(71%vs.
80%).
59Itissuggestedthatoestrogenproductioncontinuesinobesepostmenopausalwomenduetoaromatisationintheperipheraladiposetissuewhichwouldcompromiseanyindirectadvantageofchemother-apyduetochemicallyinducedmenopauseparticu-larlyinpatientswithoestrogenreceptorpositivetumours.
Whenthebloodleukocytenadirisusedasasurrogatemarkerforthedrugeffect,obesepatientswhoreceiveintravenouscyclophospha-midemethotrexateand5-uorouracilhavelesssevereleukocytenadirsthantheleanpatientswhichsuggeststhatwhentheobesearetreatedaccordingtostandardschedulestheymaybesignicantlyunder-dosed.
60Furthermore,obesepatientsmaybegivenalowerdoseofchemother-apyinordertoavoidtoxicity,whichwouldcontributetowardsapoorerprognosis.
61ObesityandtheprognosisofbreastcancerTheoverallanddisease-freesurvivalisworseinmostbutnotallstudiesofprognosisofobesepre-andpostmenopausalwomenwithbreastcancer.
Thiseffectisapparentafteradjustmentforstageatdiagnosisandtheadequacytreatmentandmaybepartlyduetodelayeddetectionandmorerapidgrowthofmetastatictissueduetoimpairedcellularimmunityandhigheroestrogenlevels.
62–66TheAmericanCancerSociety'sCancerPreven-tionStudyII(CPS-II),aprospectivemortalitystudywhichincluded424168postmenopausalwomenand2852breastcancerdeathsfoundatfollow-upof14yearsthatbreastcancermortalityratesincreasedcontinuallyandsubstantiallywithin-creasingBMI(RR:3.
08,95%CI:2.
09–4.
51forBMI440.
0comparedtoBMI18.
5–20.
49).
Ifcausal,ARTICLEINPRESSObesityandbreastcancer:areviewoftheliterature89themultivariate-adjustedRRestimatesinthisstudycorrespondtoapproximately30–50%ofbreastcancerdeathsamongpostmenopausalwo-menintheUSpopulationbeingattributabletooverweight.
67Astudyof735node-positivepatientsfoundatamedianfollow-upof10.
7years,the10-year,disease-freeratefornon-obesepatientswas54%(95%CI:50–58%)comparedwith40%(CI:33–47%)forpatientsclassiedasobese.
Althoughobesepatientstendedtohavesomewhatlessfavourableoutcomebasedonstandardprognosticcriteria,aproportional-hazardsregressionmodeladjustingforotherfactorsindicatedthatriskfordiseaserecurrenceamongobesepatientswas1.
33timesthatofthenon-obesepopulation(CI:1.
05–1.
68).
68Thenegativeeffectofobesityonbreastcancersurvivalhasalsobeendemonstratedinseveralsmall-scalestudies.
Astudyof213womenwithbreastcancerfoundthattheestimatedsurvivalprobabilityforwomenwithBMIof20wasabout12%higherthanthosewithBMIof24,overa10-yearfollow-up.
69Theprognosisofbreastcancerwaspoorinbothpremenopausalandpostmeno-pausalobesewomen.
70Premenopausalobesewo-menhadupto70%decreasedsurvivalandrecurrence-freeintervalofbreastcancerafteradjustmentforstageatdiagnosisandtreat-ment.
65,71Ameta-analysisof8029womenfoundthatBMIhadaprognosticsignicanceinbreastcancer,hazardratio1.
56(95%CI:1.
22–2.
00).
However,thiseffectwasfoundtobeheteroge-neousandsomestudieshavereportednoadversesurvivaleffectofhighBMI.
7,72–77ThesedifferencesinreportedsurvivalinbreastcancerpatientswithhighBMIcanpartlybeexplainedbytheuseofdifferingdenitionsofobesitybyvariousstudiesandthefactthatsomestudieshaveanalysedthedataforoverweightandobesepatientstogether.
However,thepossibilityofpublicationbiasagainstnegativestudiesshouldnotbedismissed.
Thereisindirectevidencethatpoorsurvivalinwomenwithbreastcancerinlowersocio-economicclassesmaybepartlyexplainedbythegreaterincidenceofobesityinlowersocialclasses.
30,45,47,78,79Thehostfactorssuchascellularimmunityandnutritionthatmaydeterminemetas-tasesandrecurrenceofbreastcancermaybeunfavourableindeprivedobesepatientsoflowersocio-economicstatus.
45,80Itisalsosuggestedthatwomenfromlowersocio-economicclassestendtohavepooraccessandutilisationofthediagnosticandtherapeuticsupportforbreastcancer.
81Insummary,consistent,independentandpositiveassociationhasbeenfoundbetweenobesityandbreastcancerinpostmenopausalwomen,andinthemajorityoftheliteraturebetweenobesityandpoorprognosisofbreastcancerinbothpre-andpostmenopausalwomen.
Theattributable-riskes-timatesduetoobesityarecomparabletothoseduetoapositivefamilyhistory(6–19%).
70,82Itissuggestedthatreductionofobesitycandecreasethecasesofbreastcancerbyone-tenthinEuropewithaconsequentreductioninmortality.
83Despiteadecreaseinmortalityfrombreastcancerinrecentyears,breastcancerkills12000womenayearintheUnitedKingdomalone,andtensofthousandsinEurope.
Itisfearedthatincreasingobesityinwomenwillmanifestitseffectofincreasedincidenceofbreastcancerinpostmeno-pausalwomeninthecomingyears.
Sinceobesityisoneofthefewriskfactorsforbreastcancerwhichcanbemodiedthroughoutlife,84apublichealthpolicy,planningandhealtheducationcampaignareurgentlyrequiredtoaddresstherisingproblemsofobesityandbreastcancer.
AcknowledgementsIamgratefulforthehelpofthestaffoftheRosewellLibrary,ConquestHospital,St.
Leonard-on-Sea.
References1.
SeidellJC.
Timetrendsinobesity:anepidemiologicalperspective.
HormMetabRes1997;29(4):155–8.
2.
HMSO.
HealthSurveysofEngland:cardiovasculardisease.
London.
HMSO,1998.
3.
PrenticeA,JebbSA.
ObesityinBritain:gluttonyorsloth.
BMJ1995;311(7002):4379.
4.
WorldHealthOrganisation.
MeasuringobesityFclassica-tionanddescriptionofanthropometricdata.
Copenhagen;WHO:1989.
5.
HanTS,vanLeerEM,SeidellJC,LeanME.
Waistcircumfer-enceactionlevelsintheidenticationofcardiovascularriskfactors:prevalencestudyinarandomsample.
BMJ1995;311(7017):14015.
6.
HuangZ,HankinsonSE,ColditzGA,etal.
Dualeffectsofweightandweightgainonbreastcancerrisk.
JAMA1997;278(17):140711.
7.
KatohA,WatzlafVJ,D'AmicoF.
Anexaminationofobesityandbreastcancersurvivalinpost-menopausalwomen.
BrJCancer1994;70(5):92833.
8.
LondonSJ,ColditzGA,StampferMJ,etal.
Prospectivestudyofrelativeweight,height,andriskofbreastcancer.
JAMA1989;262(20):28538.
9.
PathakDR,WhittemoreAS.
Combinedeffectsofbodysize,parity,andmenstrualeventsonbreastcancerincidenceinsevencountries.
AmJEpidemiol1992;135(2):15368.
10.
vandenBrandtPA,SpiegelmanD,YaunSS,etal.
Pooledanalysisofprospectivecohortstudiesonheight,weight,andbreastcancerrisk.
AmJEpidemiol2000;152(6):51427.
11.
VattenLJ,KvinnslandS.
Prospectivestudyofheight,bodymassindexandriskofbreastcancer.
ActaOncol1992;31(2):195200.
ARTICLEINPRESS90A.
R.
Carmichael,T.
Bates12.
UrsinG,LongneckerMP,HaileRW,GreenlandS.
Ameta-analysisofbodymassindexandriskofpremenopausalbreastcancer.
Epidemiology1995;6(2):13741.
13.
PeacockSL,WhiteE,DalingJR,VoigtLF,MaloneKE.
Relationbetweenobesityandbreastcancerinyoungwomen.
AmJEpidemiol1999;149(4):33946.
14.
WillettWC,BrowneML,BainC,etal.
Relativeweightandriskofbreastcanceramongpremenopausalwomen.
AmJEpidemiol1985;122(5):73140.
15.
ChangS,BuzdarAU,HurstingSD.
Inammatorybreastcancerandbodymassindex.
JClinOncol1998;16(12):37315.
16.
WentenM,GillilandFD,BaumgartnerK,SametJM.
Associa-tionsofweight,weightchange,andbodymasswithbreastcancerriskinHispanicandnon-Hispanicwhitewomen.
AnnEpidemiol2002;12(6):4354417.
SchapiraDV,KumarNB,LymanGH,CoxCE.
Obesityandbodyfatdistributionandbreastcancerprognosis.
Cancer1991;67(2):5238.
18.
SchapiraDV,KumarNB,LymanGH,CoxCE.
Abdominalobesityandbreastcancerrisk.
AnnInternMed1990;112(3):1826.
19.
Ballard-BarbashR.
Anthropometryandbreastcancer.
BodysizeFamovingtarget.
Cancer1994;74(3Suppl):1090100.
20.
FolsomAR,KayeSA,PrineasRJ,etal.
Increasedincidenceofcarcinomaofthebreastassociatedwithabdominaladiposityinpostmenopausalwomen.
AmJEpidemiol1990;131(5):794803.
21.
LiCl,StanfordJL,DalingJR.
Anthropometricvariablesinrelationtoriskofbreastcancerinmiddle-agedwomen.
IntJEpidemiol2000;29(2):20813.
22.
TornbergSA,CarstensenJM.
RelationshipbetweenQuete-let'sindexandcancerofbreastandfemalegenitaltractin47,000womenfollowedfor25years.
BrJCancer1994;69(2):35861.
23.
MorimotoLM,WhiteE,ChenZ,etal.
Obesity,bodysize,andriskofpostmenopausalbreastcancer:theWomen'sHealthInitiative(UnitedStates).
CancerCausesControl2002;13:74151.
24.
TretliS.
Heightandweightinrelationtobreastcancermortalityandmorbidity:aprospectivestudyof570,000womeninNorway.
IntJCancer1989;44:2330.
25.
SellersTA,KushiLH,PotterJD,etal.
Effectoffamilyhistory,body-fatdistribution,andreproductivefactorsontheriskofpostmenopausalbreastcancer.
NEnglJMed1992;326(20):13239.
26.
WillettWC.
Whoissusceptibletocancerofthebreast,colonandprostateAnnNYAcadSci1995;768:111.
27.
MagnussonC,BaronJ,PerssonI,etal.
Bodysizeindifferentperiodsoflifeandbreastcancerriskinpost-menopausalwomen.
IntJCancer1998;76(1):2934.
28.
LaGuardiaM,GiammancoM.
Breastcancerandobesity.
PanminervaMed2001;43(2):12333.
29.
StollBA.
Adiposityasariskdeterminantforpostmenopausalbreastcancer.
IntJObesRelatMetabDisord2000;24(5):52733.
30.
StollBA.
Obesityandbreastcancer.
IntJObesRelatMetabDisord1996;20(5):38992.
31.
KalekoM,RutterWJ,MillerAD.
OverexpressionofthehumaninsulinlikegrowthfactorIreceptorpromotesligand-dependentneoplastictransformation.
MolCellBiol1990;10(2):46473.
32.
MacaulayVM.
Insulin-likegrowthfactorsandcancer.
BrJCancer1992;65(3):31120.
33.
PollakMN,PolychronakosC,YouseS,RichardM.
Char-acterizationofinsulin-likegrowthfactorI(IGF-I)receptorsofhumanbreastcancercells.
BiochemBiophysResCommun1988;154(1):32631.
34.
ReavenGM.
SyndromeX.
BloodPressSuppl1992;4:136.
35.
StollBA.
Breastcancer:theobesityconnection.
BrJCancer1994;69(5):799801.
36.
StollBA.
Nutritionandbreastcancerrisk:cananeffectviainsulinresistancebedemonstratedBreastCancerResTreat1996;38(3):23946.
37.
DaniellHW,TamE,FiliceA.
LargeraxillarymetastasesinobesewomenandsmokerswithbreastcancerFaninuencebyhostfactorsonearlytumorbehavior.
BreastCancerResTreat1993;25(3):193201.
38.
FriedenreichCM,RohanTE.
Physicalactivityandriskofbreastcancer.
EurJCancerPrev1995;4(2):14551.
39.
KorzeniowskiS,DybaT.
Reproductivehistoryandprognosisinpatientswithoperablebreastcancer.
Cancer1994;74(5):15914.
40.
MerzenichH,BoeingH,WahrendorfJ.
Dietaryfatandsportsactivityasdeterminantsforageatmenarche.
AmJEpidemiol1993;138(4):21724.
41.
MaehleBO,TretliS,SkjaervenR,ThorsenT.
Premorbidbodyweightanditsrelationstoprimarytumourdiameterinbreastcancerpatients;itsdependenceonestrogenandprogesteronreceptorstatus.
BreastCancerResTreat2001;68(2):15969.
42.
CuiY,WhitemanMK,FlawsJA,etal.
Bodymassandstageofbreastcanceratdiagnosis.
IntJCancer2002;98(2):27983.
43.
HallHI,CoatesRJ,UhlerRJ,etal.
Stageofbreastcancerinrelationtobodymassindexandbracupsize.
IntJCancer1999;82(1):237.
44.
RichardsonJL,LangholzB,BernsteinL,etal.
Stageanddelayinbreastcancerdiagnosisbyrace,socioeconomicstatus,ageandyear.
BrJCancer1992;65(6):9226.
45.
SchrijversCT,MackenbachJP,LutzJM,QuinnMJ,ColemanMP.
Deprivationandsurvivalfrombreastcancer.
BrJCancer1995;72(3):73843.
46.
StollBA.
Obesity,socialclassandWesterndiet:alinktobreastcancerprognosis.
EurJCancer1996;32A(8):12935.
47.
TorgersonD.
Riskfactorsforbreastcancer.
Socioeconomicdifferencesmightbeexplainedbybodymass.
BMJ1994;309(6969):1662.
48.
ClearyMP,MaihleNJ.
Theroleofbodymassindexintherelativeriskofdevelopingpremenopausalversuspostmeno-pausalbreastcancer.
ProcSocExpBiolMed1997;216(1):2843.
49.
GiuffridaD,LupoL,LaPortaGA,etal.
Relationbetweensteroidreceptorstatusandbodyweightinbreastcancerpatients.
EurJCancer1992;28(1):1125.
50.
MaehleBO,TretliS.
Pre-morbidbody-mass-indexinbreastcancer:reversedeffectonsurvivalinhormonereceptornegativepatients.
BreastCancerResTreat1996;41(2):12330.
51.
ArndtV,SturmerT,StegmaierC,etal.
PatientdelayandstageofdiagnosisamongbreastcancerpatientsinGerma-nyFapopulationbasedstudy.
BrJCancer2002;86(7):103440.
52.
BertinML,CroweJ,GordonSM.
Determinantsofsurgicalsiteinfectionafterbreastsurgery.
AmJInfectControl1998;26(1):615.
53.
VintonAL,TraversoLW,JollyPC.
Woundcomplicationsaftermodiedradicalmastectomycomparedwithtylectomywithaxillarylymphnodedissection.
AmJSurg1991;161(5):5848.
54.
BanerjeeD,WilliamsEV,IlottJ,MonypennyIJ,WebsterDJ.
ObesitypredisposestoincreaseddrainagefollowingaxillaryARTICLEINPRESSObesityandbreastcancer:areviewoftheliterature91nodeclearance:aprospectiveaudit.
AnnRCollSurgEngl2001;83(4):26871.
55.
WernerRS,McCormickB,PetrekJ,etal.
Armedemainconservativelymanagedbreastcancer:obesityisamajorpredictivefactor.
Radiology1991;180(1):17784.
56.
BentzenSM,DischeS.
Morbidityrelatedtoaxillaryirradia-tioninthetreatmentofbreastcancer.
ActaOncol2000;39(3):33747.
57.
AhrendtGM,LaudP,TjoeJ,etal.
DoesbreasttumorlocationinuencesuccessofsentinellymphnodebiopsyJAmCollSurg2002;194(3):27884.
58.
NewmanLA,KuererHM,McNeeseMD,etal.
Reductionmammoplastyimprovesbreastconservationtherapyinpatientswithmacromastia.
AmJSurg2001;181(3):21520.
59.
MehtaRR,BeattieCW,GuptaTK.
Endocrineproleinbreastcancerpatientsreceivingchemotherapy.
BreastCancerResTreat1991;20:12532.
60.
PoikonenP,BlomqvistC,JoensuuH.
Effectofobesityontheleukocytenadirinwomentreatedwithadjuvantcyclopho-sphamide,methotrexate,anduorouracildosedaccordingtobodysurfacearea.
ActaOncol2001;40(1):6771.
61.
RosnerGL,HargisJB,HollisDR,etal.
Relationshipbetweentoxicityandobesityinwomenreceivingadjuvantchemo-therapyforbreastcancer:resultsfromcancerandleukemiagroupBstudy8541.
JClinOncol1996;14(11):30008.
62.
NewmanSC,MillerAB,HoweGR.
Astudyoftheeffectofweightanddietaryfatonbreastcancersurvivaltime.
AmJEpidemiol1986;123(5):76774.
63.
SenieRT,RosenPP,RhodesP,LesserML,KinneDW.
Obesityatdiagnosisofbreastcarcinomainuencesdurationofdisease-freesurvival.
AnnInternMed1992;116(1):2632.
64.
TornbergS,CarstensenJ.
Serumbeta-lipoprotein,serumcholesterolandQuetelet'sindexaspredictorsforsurvivalofbreastcancerpatients.
EurJCancer1993;29A(14):202530.
65.
TretliS,HaldorsenT,OttestadL.
Theeffectofpre-morbidheightandweightonthesurvivalofbreastcancerpatients.
BrJCancer1990;62(2):299303.
66.
ZhangS,FolsomAR,SellersTA,KushiLH,PotterJD.
Betterbreastcancersurvivalforpostmenopausalwomenwhoarelessoverweightandeatlessfat.
TheIowaWomen'sHealthStudy.
Cancer1995;76(2):27583.
67.
PetrelliJM,CalleEE,RodriguezC,ThunMJ.
Bodymassindex,height,andpostmenopausalbreastcancermortalityinaprospectivecohortofUSwomen.
CancerCausesControl2002;13(4):32532.
68.
BastarracheaJ,HortobagyiGN,SmithTL,KauSW,BuzdarAU.
Obesityasanadverseprognosticfactorforpatientsreceivingadjuvantchemotherapyforbreastcancer.
AnnInternMed1994;120(1):1825.
69.
KyogokuS,HirohataT,TakeshitaS,etal.
Survivalofbreast-cancerpatientsandbodysizeindicators.
IntJCancer1990;46(5):82431.
70.
Ballard-BarbashR,SwansonCA.
Bodyweight:estimationofriskforbreastandendometrialcancers.
AmJClinNutr1996;63(3Suppl):437S41S.
71.
Demark-WahnefriedW,WinerEP,RimerBK.
Whywomengainweightwithadjuvantchemotherapyforbreastcancer.
JClinOncol1993;11(7):141829.
72.
GreenbergER,VesseyMP,McPhersonK,DollR,YeatesD.
Bodysizeandsurvivalinpremenopausalbreastcancer.
BrJCancer1985;51(5):6917.
73.
JainM,MillerAB.
Pre-morbidbodysizeandtheprognosisofwomenwithbreastcancer.
IntJCancer1994;59(3):3638.
74.
MarretH,PerrotinF,BougnouxP,etal.
Lowbodymassindexisanindependentpredictivefactoroflocalrecurrenceafterconservativetreatmentforbreastcancer.
BreastCancerResTreat2001;66(1):1723.
75.
MenonKV,HodgeA,HoughtonJ,BatesT.
Bodymassindex,heightandcumulativemenstrualcycleatthetimeofdiagnosisarenotriskfactorsforpooroutcomeinbreastcancer.
Breast1999;8:32833.
76.
ObermairA,KurzC,HanzalE,etal.
Theinuenceofobesityonthedisease-freesurvivalinprimarybreastcancer.
AnticancerRes1995;15(5B):22659.
77.
SohrabiA,SandozJ,SprattJS,PolkJr,HC.
Recurrenceofbreastcancer.
Obesity,tumorsize,andaxillarylymphnodemetastases.
JAMA1980;244(3):2645.
78.
HaybittleJ,HoughtonJ,BaumM.
Socialclassandweightasprognosticfactorsinearlybreastcancer.
BrJCancer1997;75(5):72933.
79.
KarjalainenS,PukkalaE.
Socialclassasaprognosticfactorinbreastcancersurvival.
Cancer1990;66(4):81926.
80.
CarnonAG,SsemwogerereA,LamontDW,etal.
Relationbetweensocioeconomicdeprivationandpathologicalprog-nosticfactorsinwomenwithbreastcancer.
BMJ1994;309(6961):10547.
81.
AntmanK,Abraido-LanzaAF,BlumD,etal.
Reducingdisparitiesinbreastcancersurvival:aColumbiaUniversityandAvonBreastCancerResearchandCareNetworkSymposium.
BreastCancerResTreat2002;75:26980.
82.
HunterDJ,WillettWC.
Diet,bodysize,andbreastcancer.
EpidemiolRev1993;15(1):11032.
83.
LaVecchiaC.
Nutritionalfactorsandcancersofthebreast,endometriumandovary.
EurJCancerClinOncol1989;25(12):194551.
84.
KelseyJL,BernsteinL.
Epidemiologyandpreventionofbreastcancer.
AnnuRevPublicHealth1996;17:4767.
ARTICLEINPRESS92A.
R.
Carmichael,T.
Bates
- www.elsevier.com/locate/breast相关文档
- gastrostomy168post
- 11.71168post
- images168post
- Saturated168post
- support168post
- account168post
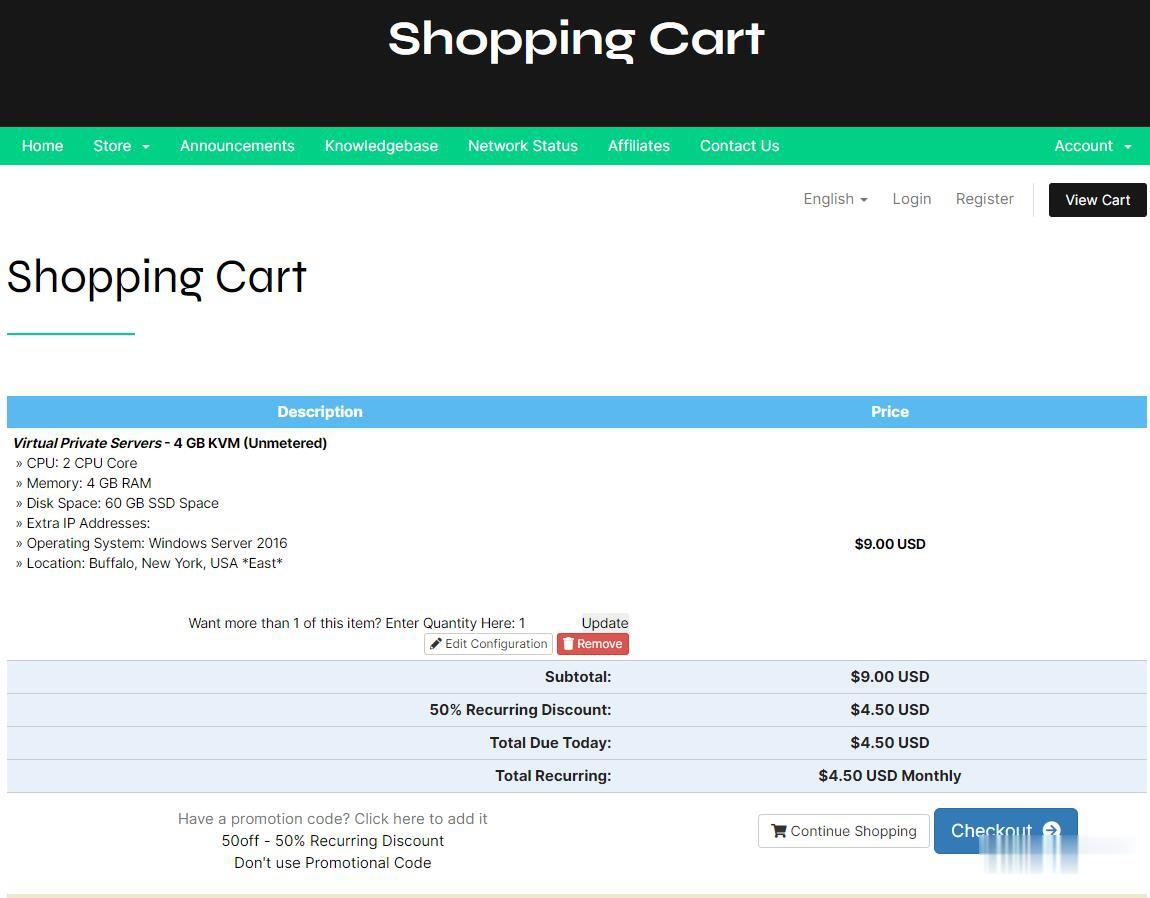
RFCHOST - 洛杉矶CN2 GIA VPS季付23.9美元起 100Mbps带宽
RFCHOST,这个服务商我们可能有一些朋友知道的。不要看官网是英文就以为是老外服务商,实际上这个服务商公司在上海。我们实际上看到的很多商家,有的是繁体,有的是英文,实际上很多都是我们国人朋友做的,有的甚至还做好几个品牌域名,实际上都是一个公司。对于RFCHOST商家还是第一次分享他们家的信息,公司成立大约2015年左右。目前RFCHOST洛杉矶机房VPS正进行优惠促销,采用CN2优化线路,电信双...
PacificRack(19.9美元/年)内存1Gbps带vps1GB洛杉矶QN机房,七月特价优惠
pacificrack怎么样?pacificrack商家发布了七月最新优惠VPS云服务器计划方案,推出新款优惠便宜VPS云服务器采用的是国产魔方管理系统,也就是PR-M系列,全系基于KVM虚拟架构,这次支持Windows server 2003、2008R2、2012R2、2016、2019、Windows 7、Windows 10以及Linux等操作系统,最低配置为1核心2G内存1Gbps带宽1...

CheapWindowsVPS$4.5/月,美国VPS/免费Windows系统/1Gbps不限流量/,可选美洲、欧洲、亚洲等8大机房
国外商家提供Windows系统的并不常见,CheapWindowsVPS 此次提供的 2 款 VPS 促销套餐,提供 5 折永久优惠码,优惠后月付 4.5 美元起,价格还是挺诱人的,VPS 不限流量,接入 1Gbps 带宽,8 个机房皆可选,其中洛杉矶机房还提供亚洲优化网络供选择,操作系统有 Windows 10 专业版、2012 R2、2016、Linux等。Cheap Windows VPS是...
168post为你推荐
-
摩根币JPM摩根币是什么?怎么赚钱是骗人的吗?12306崩溃为什么12306进不去云计算什么叫做“云计算”?www.983mm.comwww.47683.com百度关键词价格查询百度关键字如何设定竟价价格?336.com求那个网站 你懂得 1552517773@qqwww.544qq.COM跪求:天时达T092怎么下载QQm.kan84.net经常使用http://www.feikan.cc看电影的进来帮我下啊www.idanmu.com新开奇迹SF|再创发布网|奇迹SF|奇迹mu|网通奇迹|电信奇迹|45gtv.comLETSCOM是什么牌子?