opening科比凯拉
科比凯拉 时间:2021-03-24 阅读:()
Chapter18DNARepairandResistancetoCancerTherapyAntónioS.
Rodrigues,BrunoCostaGomes,CéliaMartins,MartaGromicho,NunoG.
Oliveira,PatríciaS.
GuerreiroandJoséRueffAdditionalinformationisavailableattheendofthechapterhttp://dx.
doi.
org/10.
5772/539521.
IntroductionHumansareconstantlyexposedtodiversechemicalandphysicalagentsthathavethepotentialtodamageDNA,suchasreactiveoxygenspecies(ROS),ionizingradiation(IR),UVlight,andvariousenvironmental,dietaryorpollutantchemicalagents.
Theintegrityandsurvivalofacelliscriticallydependentongenomestability,andcellspossessmulti‐plepathwaystorepairtheseDNAlesions.
Thesepathwaysarediverseandtargetdiffer‐enttypesoflesions.
ThecriticalroleplayedbyDNArepairinthemaintenanceofgenomestabilityishighlightedbythefactthatmanyenzymesinvolvedhavebeenconservedthroughevolution[1-4].
VeryrarelygermlinemutationsoccurinseveraloftheDNArepairgenesandarethecauseofcancerpredisposingsyndromes,suchasXerodermapigmentosum(XP),[5],Fanconianemia(FA)andataxiatelangiectasia(AT)andareassociatedwithinherentchromosomeinstability[2].
Oneofthemostwell-knownexamplesofadefectinDNArepairleadingtocanceristheassociationofgerm-lineBRCA1/2mutationswithbreast,ovarianandperitonealmalignan‐cies[6].
TheserarehumanDNArepairsyndromeshavebeeninvaluableinprovidingmech‐anisticexplanationsfortheinvolvementofDNArepairsystemincancer.
Theyhavealsobeeninstrumentalinthetranslationofthesefindingstotheclinic.
Ontheotherhand,recentstudieshaveshownthatdefectiveDNAdamagerepairispresentinvirtuallyallsporadictumours[7].
MutationsinDNArepairgenescouldbeei‐therresponsiblefortheoccurrenceoftumoursorcouldariseduetorandomaccumula‐tionofmutationsduringcyclingofcancercells.
ThepresenceofincorrectDNArepairintumourcellspredisposesthemtoaccumulateevenmoregeneticalterations.
Forexample,colorectalandendometrialcancerswithdefectiveDNAmismatchrepair(MMR)dueto2013Rodriguesetal.
;licenseeInTech.
ThisisanopenaccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/3.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
mutationsintheMLH1andMSH2genesexhibitincreasedratesofacquisitionofsinglenucleotidechangesandsmallinsertions/deletions[8].
Thus,thepresenceofa"mutatorphenotype"[9]couldincreasetheevolutionaryacquisitionofalterationsthatultimatelycouldleadtoenhanceddrugresistance.
AfurtherreminderontheimportanceofDNArepairistheobservationthatmutationsinspecificgenescanleadnottoanincreaseincancerbuttoacceleratedagingsyndromes[7].
AnexampleofthisisCockayne'ssyndrome(CS),whichcausessevereprogeroidsyndromes[10].
Mutationsinthegenesthatencodetwoproteinsinanucleotideexcisionrepair(NER)sub-pathwaycalledtranscriptioncoupledrepair(TCR)causeglobalprematurecelldeaththroughapoptosis.
InthiscaseapoptosisensuresthatDNAmutationsarenottransmittedtodaughtercells,albeitattheexpenseofcellviability,andhighlightstheimportanceofmain‐tainingDNAintegrity.
Onemajorproblemincancertherapyisthefactthatofthe7.
6millioncancerdeathsthatoc‐cureveryyearworldwide(2008data;http://www.
who.
int/cancer/en/),manyareduetofail‐ureofcancertherapyassociatedwithacquiredandintrinsicresistancemechanisms.
Thesemechanismsofresistancecanbeclassifiedindifferentways,butthemostcharacterizedarealteredcellulardrugtransport,increasedsurvivalordecreasedcelldeath,alteredDNAre‐pair,andalterationsindrugtargets[11,12].
OverthelastyearstheimportanceofDNAre‐pairpathwaysinresistancetochemotherapyhasbeenincreasinglyrecognized,buttranslationtotheclinicisstillscarce.
SincemanyclassicalcancertherapiestargetDNA,theinfluenceofDNArepairsystemsinresponsetoDNAdamagewhichprimarilyresultfromchemotherapyandradiotherapyiscriticaltocellsurvival.
TheuseofinhibitorsofDNAre‐pairorDNAdamagesignallingpathwaysprovidesaninterestingopportunitytotargetthegeneticdifferencesthatexistbetweennormalandtumourtissue[13,14].
TherationaleunderlyingtheuseofDNAdamagingagentsintherapeuticstrategiesistokillcancercellswhilesparingnormaltissues,duetoincreasedcellcyclingofcancercells.
Un‐fortunatelyhighlycyclingnormalcells(e.
g.
bonemarrow,hairfolliclesandgastrointestinalepithelia)arealsotargetedbyDNAdamagingtherapeuticagents,givingrisetothesecon‐daryeffectsnormallyseenaftercancertherapy(e.
g.
diarrhoea,mouthulcers,hairloss,anae‐miaandsusceptibilitytoinfections).
Nevertheless,DNA-damagingchemotherapeuticagentsareeffectiveandprolongsurvivalofcancerpatients[15].
Chemotherapeuticagentscommonlyusedincancertreatmentproduceaplethoraoflesionsthatcanbetargetsforcel‐lularresponses.
Forexample,DNAdoublestrandbreaks(DSBs),single-strandbreaks(SSBs),andoxidizedbasesareinducedbyionizingradiation(IR),anthracyclines,platinumcompoundsandtaxanes.
AnthracyclinesaretopoisomeraseIIinhibitorsandDNAinterca‐latingagents,whichwhenusedcanleadtoDSBs.
Platinumcompoundsarebifunctionalal‐kylatingagentsthatinducepredominantlyintra-andinterstrandcrosslinks(ICLs)andtaxanesaremitoticinhibitors.
Alltheselesionsinducecellularresponsesthatcoveramulti‐tudeofpathways,includingDNArepairpathways,DNAtolerancemechanisms,coordina‐tionnetworksthatlinkrepairandcellcycleprogression,aswellasapoptoticandothercelldeathpathwayswhenDNAdamageisirreparable[16-19].
NewResearchDirectionsinDNARepair490TheDNArepairpathwaysthatrespondtotheselesionsinclude:directrepairofalkylad‐ductsbyO6-alkylguanineDNAalkyltransferase(MGMT);repairofbasedamageandSSBsbybaseexcisionrepair(BER);repairofbulkyDNAadductsbynucleotideexcisionrepair(NER);repairofcross-linksbyDNAinterstrandcross-linkrepairandrepairofmismatchesandinsertion/deletionloopsbyDNAmismatchrepair(MMR);repairofDSBsbyhomolo‐gousrecombination(HR)andnon-homologousendjoining(NHEJ).
DetaileddescriptionofthebiochemicalpathwaysofDNArepairisbeyondthescopeofthischapterasseveralre‐viewsonthesubjecthavebeenpublished[1,17,20-23].
TheobservationthatavarietyoftumoursfrequentlypresentderegulatedexpressionofDNArepairgenes(e.
g.
MGMT,PARP1)rapidlyleadtothenotionthatDNArepairpath‐wayscouldbetargetedincancertreatmentandleadtopersonalizedtherapy[24,25].
Tu‐mourswithspecificDNArepairdefectscouldbecompletelydependentonback-upDNArepairpathwaysfortheirsurvival.
Thisdependencecouldbeexploitedtherapeuticallytoin‐ducecelldeathandapoptosisintumourcells[26,27].
Thegeneticstateinwhichsimultane‐ousinactivationof2genes(orpathways)islethal,whilelossofoneortheotheraloneisviableiscalledsyntheticlethality(alsoknownasconditionalgenetics).
Therationaleforin‐ducingsyntheticlethalityincanceristhatcertaincancercellslackonepathwaytorepairtheirDNA(e.
g.
HR)buthavealternativepathways(baseexcisionorsingle-strandrepair)thatallowthemtosurvive.
InhibitionofthesealternativepathwayswouldthenimpairDNArepairandinducecelldeath[26,27].
Thereforeitpredictsthatgenotoxicagentslead‐ingtoaparticulartypeofDNAdamagewillkillcancercellswithgeneticdeficitsinrepairofthattypeofdamage.
Recently,thisspecificanticancerstrategyhasbeenthefocusofintenseinvestigations[28,29].
InthecaseofthehereditaryBRCA1/2-deficientbreastandovariancancersyndromes,men‐tionedearlier,thisstrategyhasbeentranslatedintotheclinic,intheformofPARPinhibi‐tors.
TheseBRCA1/2-tumoursaredefectiveintherepairofDSBsbyHR.
WhenareplicationforkinoneofthesetumoursencountersaDNASSB,itconvertsthatintoaDSB,butthepresenceofaDSBpreventsprogressionofthereplicationapparatus.
SinceBRCA1/2arebothrequiredforDSBrepair,thetumourcellswiththosemutatedgeneswilldependonrepairofSSBstopreventDSBsfromoccurring.
TheDNArepairproteinPARP1isrequiredforrepairofSSBs,andsmallmolecularinhibitorsofPARP1willpreventrepairofSSBs,morespecifi‐callyincellsthataredeficientinBRCA1/2.
SincenormalcellshavetheabilitytorepairtheDSBsgeneratedatthereplicationfork,becausetheyhaveatleastonenormalalleleofBRCA1/2,theuseofPARPinhibitorshasthepotentialoftargetingonlytumourcells.
Thisproofofconceptprovenclinically,wherethePARP1inhibitorolaparibimprovesthepro‐gression-freesurvivaloffamilialbreastcancer[30].
Followingthisleadseveralsmallmole‐culeDNArepairinhibitorsarebeingdevelopedworldwide.
However,notallBRCA1/2defectivetumoursrespondequallywelltothistypeoftherapy.
Thus,inthepastyearsevidencehasaccumulatedthatdrugresistanceisalsolinkedtoalter‐ationsinthesepathways[31-33].
Thus,tumourcellsmayalsoacquireresistancebyinvokingbiochemicalmechanismsthatreducedrugactionorbyacquiringadditionalalterationsinDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952491DNAdamageresponsepathways[34].
Therefore,thefocushasalsobeendirectedonDNArepairpathwaysthatcouldberesponsibleforcancerdrugresistance.
Resistancetochemotherapylimitstheeffectivenessofanti-cancerdrugtreatment.
Tumoursmaybeintrinsicallydrug-resistantordevelopresistancetochemotherapyduringtreatment.
Acquiredresistanceisaparticularproblem,astumoursnotonlybecomeresistanttothedrugsoriginallyusedtotreatthem,butmayalsobecomecross-resistanttootherdrugswithdifferentmechanismsofaction.
Resistancetochemotherapyisbelievedtocausetreatmentfailureinover90%ofpatientswithmetastaticcancer[35].
Thus,drugresistanceisclearlyamajorclinicalproblem.
Theattempttodevelopmoretargetedtherapeuticshasbeenamajorobjectiveincancerre‐searchinlastyears,andmoreandmoremoleculartargetsarebeingidentified(e.
g.
tyrosinekinaseinhibitors,monoclonalantibodiestargetingmembranereceptorkinases).
Someofthesetargetedtherapiesareinclinicaluse,whileothersarebeingevaluatedinclinicaltrialstovalidatetheirefficacy.
Morerecently,thequestfortargetedtherapieshasalsofocusedonDNArepairpathways.
Unfortunately,resistancetothesetherapiesisalsolikelytoappear,ashasoccurredwithothertargetedtherapies,suchasthetyrosinekinaseinhibitorsofthefusionBCR-ABL1gene,responsibleformostcasesofchronicmyeloidleukaemia(e.
g.
imati‐nib,dasatinib,nilotinib).
TheapplicationofDNArepairinhibitorsintheclinichasalsoshowntobefraughtwithdifficulty,sincetheyalsotargetDNArepairpathwaysinnormalcells.
TheearlyclinicaltrialwithMGMTinhibitorsincombinationwithtemozolomide(TMZ)wasstoppedearlybecausethecombinedtreatmentsharmedbonemarrowaswellascancertissue,whereastheclinicalsuccessofPARPinhibitorstranspiredsincePARPisnotcriticaltocellsurvival.
Hence,unlikepastvisionsofa"magicbullet"towardscancer,futureresearchoncancertherapyshouldmorereasonablyenvisagecancertherapyasa"neverendingstory",inwhichnoveltargetedtherapeuticsareconstantlybeingovercomebytheevolutionaryprocessespresentincancerouscells[36].
2.
TargetingDNArepairpathwaysAsmentioned,DNArepairpathwaysincludethedirectreversaloflesions,essentiallyde-alkylationofalkylatedbasesbyMGMT,NER,BER,MMRandthedoublestrandbreakre‐pairbyHRandNHEJ.
Alterationsinallthesepathwayshavebeenobservedindrugresistanttumourcells;however,theclinicalsignificanceofthealterationsisnotcompletelyunderstood.
Numerousgenesinvolvedineachofthesepathwayshavebeenshowntobeup-ordown-regulatedindiversetypesoftumoursandconstituteapotentialsourceofbio‐markerstoevaluatedrugresistancetocancerchemotherapeutics[25,32,33].
3.
MGMTanddrugresistanceAlkylatingagentsarewidelyusedtotreatcancers,andoneofthemajorDNAlesionsformedoccursessentiallybythealkylationofDNAattheO6-positionofguanine,whichNewResearchDirectionsinDNARepair492subsequentlycangenerateDNAbreaksandcelldeath.
TMZ,streptozotocin,procarbazineanddacarbazineareexamplesofcancerchemotherapeuticsthatmethylateDNA[37].
Directrepairofalkylatedguanineresiduesproceedsthroughtheremovalofthealkylmoi‐etybyMGMT.
MGMTisaconservedproteinfromprokaryotesthrougheukaryotes.
TheMGMTproteinremovesthealkylgroupfromO6-alkylguaninebydirecttransfertoacys‐teineresidueinitsactivesitetowhichthealkylgroupbecomescovalentlyattached,result‐ingintheinactivationoftheprotein.
TheMGMTproteinissubsequentlyubiquitinatedanddegradedbytheproteasome[38,39].
TheO6-alkylguanineadductaccountsforabout10%oftotalalkylations,butdisplaysastrongmutagenicandcytotoxicpotential,becauseO6-alkyl‐guaninesexhibitdistortedbasepairingcharacteristicsinpairingwiththymine,thereby,re‐sultinginG:CtoA:TtransitionsuponDNAreplication[40].
HencetheuniqueDNArepairmechanismwhichdependsonthesuicidaldegradationoftheMGMTprotein.
TumourexpressionofMGMTvariesandcorrelateswiththerapeuticresponsetoalkylatingagents.
NumerousstudieshavefoundastrongcorrelationbetweenMGMTactivityanddrugresistanceinprimarytumoursandestablishedhumantumourcelllines[16,41,42].
Highlevelsofexpressionhavealsobeennotedinmelanoma[43],pancreaticcarcinoma[16]besidesglioblastomas[44].
ResistancetoalkylatingagentssuchasTMZhasbeenlinkedtoover-expressionofMGMT[43].
ThereforeMGMTlevelsarebeingstudiedasbiomarkersofintrinsicchemosensitivitytoalkylatingagents,suchasTMZorBCNU(carmustine).
Conversely,reducedMGMTactivityinculturedtumourcellsandhumantumoursisof‐tentheresultofepigeneticsilencingbypromotermethylationofCpGislands,whichleadstotheformationofinactivechromatinthatlimitstranscription,andthereforehigh‐erchemosensitivitytoalkylation.
Hegietal.
reportedthatof206patientswithglioblasto‐mathatweretreatedwithTMZandradiotherapy,thosewithamethylatedMGMTpromoter(45%)hadasignificantlybettersurvival[45].
Hence,MGMTpromotermethyla‐tionstatusisemergingasaprognosticfactorfortumourtherapyandiscurrentlybeingassessedforselectingglioblastomachemosensitivitytowardsTMZ[46-48].
Themecha‐nismsunderlyingincreasedMGMTpromotermethylationarecomplexandnotcomplete‐lyknown,althoughitisoneofthemoststudiedDNArepairgenes[38].
InnormalcellsMGMTpromotermethylationisuncommon,butoccursfrequentlyintumours.
Approxi‐mately25%oftumoursofmanydifferenttypes,includingnon-small-cellcarcinomaofthelung,lymphoma,headandneckcancers,andupto40%ofgliomaandcolorectaltu‐mourswerefoundtopresentCpGislandpromotermethylation[49].
SincehighMGMTexpressionresultsindrugresistancetoalkylatingagents,onestrategytoovercomeresistanceandimproveefficacyistousepseudosubstratesofMGMT,suchasO6-benzylguanine(O6-BG)orO6-(4-bromothenyl)guanine(O6-BTGorlomeguatriborPaTrin-2)whichinactivatetheenzymeandenhancecelldeath[50].
O6-BGisaspecific,potent,andnontoxicinhibitorandleadstosensitizationofcancercellstocisplatin,chloroethylatingandmethylatingagents[51,52].
ClinicaltrialsareunderwaytotestcombinationsofO6-BGwithcarmustineorTMZforthetreatmentofglioma,anaplasticglioma,lymphoma,myeloma,co‐loncancer,melanomaandsarcoma,amongothers[53].
O6-BTGpresentshigherbioavailabil‐itythanO6-BG,butalsopresentshigherhaematologicaltoxicitywhenco-administeredwithDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952493TMZcomparedtoTMZalone.
Thereforefulluseofthisinhibitormaybemoredistant[54,55].
HaematologicaltoxicitywasalsoobservedwithO6-BTGco-administeredwithdacarba‐zineinpatientswithadvancedmelanomaandothersolidtumours[56].
ThecombinationofO6-BTGandTMZwasalsoevaluatedinaphaseIclinicaltrialforadvancedsolidtumours[57],andinapilotstudyforrefractoryacuteleukaemia[58].
AphaseIclinicaltrialwasalsoconductedassociatingO6-BTGwithIrinotecanforcolorectalcancer[59].
AphaseIIclinicaltrialofO6-BTGplusTMZforstageIVmetastaticcolorectalcancerisalreadycompleted.
Thetrialwasconsideredcompletedaftertherecruitmentof19patientsduetotheabsenceofre‐sponsesandalsobecauseevidencesfromotherstudiessuggestthattheO6-BTGdosingregi‐menwasinappropriate[55].
ThesestudiesshowedaconsistentdepletionofMGMTandprovidednon-toxicdosesofO6-BGorO6-BTGtobeusedinfurtherstudies.
Thehaematolog‐icaltoxicityobservedwiththecombinationofMGMTinhibitorsandchemotherapeuticagentsmightbeattributedtoaneffectivedepletionofMGMTinoff-targetcells[60].
Addi‐tionally,theadministrationofasub-optimaldoseoftheMGMTinhibitor,atherapeuticdos‐ingschedulethatallowstherecoveryoftheMGMTactivityorthechoiceofaninadequatetreatmentforthetypeofcancercouldexplainthelackofeffectsinclinicaltrials.
Inviewofthis,tumour-targeteddeliveryofMGMTinhibitorsbythedevelopmentofspecificformula‐tionsorlocaladministration[61]couldbeadoptedtoimprovethetherapeuticefficacyofthechemotherapeuticdrugsandtotranslateintotheclinictheresultsobtainedinpreclinicalstudies.
Nonetheless,itisnotclearifclinicalapplicationofMGMTinhibitorsisaviablether‐apyinallsettings.
4.
TargetingMMRincancerdrugresistanceMMRisinvolvedinthedetectionandrepairofbase-basemispairsduringDNAreplication,smallinsertion/deletionmutationsatrepetitivemicrosatelliteregionsandalsointheregula‐tionofhomologousrecombination[62].
MMRproteinsarealsoinvolvedintherepairofDNAdamagecausedbyROSandalkylatingagents.
MMRproteinsinteractwithcompo‐nentsofotherrepairpathways,includingNER,BER,andHR,thussignallingwithotherpathwaysinresponsetoDNAdamage.
TheMMRsystemconsistsofvariousproteins.
MSH2heterodimerizeswithMSH6orMSH3toformMutSαorMutSβ,respectively,bothofwhichareATPasesthatplayacriticalroleinmismatchrecognitionandinitiationofrepair.
ThisinducesaconformationalchangeinMutS,resultinginaclampthattranslocatesonDNAinaATPdependentmanner,recruitstheMutLcomplex,whichinhumansisaheterodimerconsistingoftheMLH1andPMS2proteins,anddisplacesDNApolymeraseandPCNA,thereafterrecruitinganexonuclease(EXO1)thatdegradesthenewlysynthesizedDNAstrand[63].
OtherMMRgenes(MLH1,MLH3,PMS1,andPMS2)areinvolvedinMMR.
MLH1alsoheterodimerizeswithPMS2,PMS1,orMLH3toformMutLα,MutLβ,orMutLγ,respectively[63].
Polymeraseδ(polδ)thenpolymerizestheDNAstretchandDNALigaseIperformsligation.
MMRdeficiencyleadstoawiderangeoftumourtypes.
GermlinedeficiencyinMMRac‐countsfortheLynchsyndrome(hereditarynon-polyposiscolorectalcancer-HNPCC),inNewResearchDirectionsinDNARepair494whichalargeincreaseinfrequencyofinsertionanddeletionmutationsinsimplerepeat(mi‐crosatellite)sequences,aphenomenonknownasmicrosatelliteinstability(MSI),isobserved[64].
DNAmismatchrepairdeficiencyinsporadictumoursisseenincolonic,gastric,endo‐metrial,andothersolidtumours.
MSIisalsoassociatedwithawidevarietyofnon-HNPCCandnon-colonictumours,includingendometrial,ovarian,gastric,cervical,breast,skin,lung,prostate,andbladdertumoursaswellasglioma,leukaemia,andlymphoma[65].
DefectsinMMRarealsoassociatedwithresistancetocertainchemotherapeuticagents[66].
ResistancetoalkylatingagentssuchasTMZandprocarbazineoccurswithinactivationofMMRintumourcells[63].
MMR-deficientcellsarerelativelyresistanttomethylatingagents(upto100fold),whereascellswithafunctioningMMRsystementereitherG2arrestorapoptosis,dependingontheseverityoftheDNAdamage[67].
DownregulationofproteinsoftheMMRpathwayisassociatedwithresistancetoclinicallyimportantdrugsincludingplatinum-containingcompounds,anthracyclines,alkylatingagents,antimetabolitesandepi‐podophyllotoxins[68].
Forexample,MSH2proteindeficiencybyenhancingMSH2degradationleadstosubstantialreductioninDNAmismatchrepairandincreasedresistancetothiopurines.
Somaticdele‐tionsofgenesregulatingMSH2degradationresultinundetectablelevelsofMSH2proteininleukaemiacells,MMRdeficiencyanddrugresistance[69].
Anotheragent,etoposide,isatopoisomeraseIIalpha(TOP2A)inhibitor,whichisusedinthetreatmentofbreastcancer.
AlterationsintheexpressionofdrugtargetsorDNArepairgenesareamongtheimportantresistancemechanismsagainstTOP2Ainhibitors.
DecreaseintheexpressionlevelsofTOP2A,andtheMMRgenesMSH2andMLH1mayplaysignifi‐cantrolesinthedevelopmentofchemotherapeuticresistancetoetoposideinbreastcancer.
Thesegenesmaybeconsideredforfurtherdevelopmentofnewstrategiestoovercomere‐sistanceagainsttopoisomeraseIIinhibitors[70].
MMRisalsoinvolvedinrepairofcross-linkingagentssuchasplatinumbasedchemothera‐peutics.
Increasedtolerancetoplatinum-inducedDNAdamagecanoccurthroughlossoffunctionoftheMMRpathway.
DuringMMR,cisplatin-inducedDNAadductsarerecog‐nizedbytheMMRpathway,butarenotrepaired,givingrisetosuccessiverepaircycles,ul‐timatelytriggeringapoptosis.
ThusinMMRdeficientcells,celldeathisnotasefficient,promotingtolerancetoplatinumagents[71].
MMR-deficientcellsarealsomoretolerantto6-thioguaninetreatment,usedtotreatleukae‐mias,thanMMR-proficientcells.
Theanti-metabolite6-thioguanineisincorporatedintoDNA,whereitcanbemethylatedbyS-adenosylmethionineto6-methylthioguanine(Me6-thioguanine),whichhassimilarmiscodingpropertiesasmethylguanine[68].
Nevertheless,althoughmanypreclinicalstudiessuggestMMR-deficientcellsareresistanttoalkylatingagents,fewclinicalstudieshavebeenpublishedregardingMMRdeficiencyandresponsetoalkylatingagents.
Onthecontrary,forexample,Maxwelletal.
,[72]foundthatMMRdeficiencydoesnotseemtoberesponsibleformediatingTMZresistanceinadultma‐lignantglioma.
CoupledwiththelackofsubstantialdatalinkingpolymorphismswithintheMMRgenesandresistancetochemotherapyorradiotherapy,publishedworksuggeststhatDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952495theMMRpathwayhaslowpriorityinthequestfornewcancertherapies.
However,ongo‐ingresearchontheroleofmicroRNAsandcancerdrugresistancecouldincreaseinterestinthispathway.
PublishedworkhassuggestedthatforexamplemiR-21targetsMSH2andconsequentlyinducesresistanceto5-Fluorouracil(5-FU)incolorectalcancer[73](seethesectionofmicroRNAsanddrugresistance).
5.
TargetingBERincancerdrugresistanceBERisthemainpathwayforremovingsmall,non-helix-distortingbaselesionsfromthege‐nome.
Thus,BERtargetspredominantlybaselesionsthatariseduetooxidative,alkylation,deamination,anddepurination/depyrimidinationdamage.
Someexamplesofchemothera‐peuticagentsthatgeneratelesionsthataretargetedbyBERincludeTMZ,melphalan,dacar‐bazine/procarbazine,andstreptozotocin[33].
SomechemotherapeuticagentsalsogenerateROSasa"by-product"suchasplatinum-baseddrugs(i.
e.
oxaliplatinandcisplatin),anthra‐cyclines,(i.
e.
epirubicin,daunorubicin,doxorubicin)andpaclitaxel[31,33].
ROSinduceDNAlesionsthatarealsorepairedbytheBERpathway.
Additionally,IRproducesanum‐berofDNAlesionsthatarerepairedbytheBERpathway.
EndogenousproductionofROSalsogivesrisetoseverallesions,whicharevariableinnumberandconsequence.
Forin‐stancethehighlymutagenic8-hydroxyguanine(8-oxoG)isformedinlargequantitiesasaconsequenceofthehighoxidationpotentialofthisbase,andhasamiscodingeffect,duetoDNApolymeraseactivitywhichinsertsadenineoppositeto8-oxoG,resultinginG:CtoA:Ttransitionmutations.
TheBERpathwayisinitiatedbyoneofmanyDNAglycosylases,whichrecognizeandcata‐lyzetheremovalofdifferentdamagedbases.
AfterrecognitionofthedamagedbasebytheappropriateDNAglycosylase,itcatalyzesthecleavageofanN-glycosidicbond,thusre‐movingthedamagedbaseandcreatinganapurinicorapyrimidinicsite(APsite).
TheDNAbackboneiscleavedbyeitheraDNAAPendonucleaseoraDNAAPlyase,activitypresentinsomeglycosylases.
Thiscreatesasingle-strandedDNAnick5'totheAPsite.
ThenewlycreatednickisprocessedbytheAPendonuclease,creatingasingle-nucleotidegapintheDNA.
AtthispointBERcanproceedthroughashort-patchBER,wherepolymeraseβ(polβ)introducesasinglenucleotidepasttheabasicsiteandLigaseIIIαsealstheDNAnick,orthroughalong-patchBER,wherePolymeraseδ/εintroducestwotoeightnucleotidespasttheabasicsite.
TheresultingoverhangDNAisexcisedbyFEN1endonucleaseandthenicksealedbyDNAligaseI[74].
Inadditiontotheseenzymes,anumberofaccessoryproteinsareinvolvedinBER,includingtheX-raycross-complementationgroup1protein(XRCC1),PARP1,theproliferatingcellnuclearantigen(PCNA),andtheheterotrimertermed9-1-1,whichfunctioninscaffoldsforthecoreBERenzymes[75].
PreclinicalevidenceshaveimpliedtheBERpathwayintherepairofDNAlesionsinducedbyantimetabolites,monofunctionalalkylatingdrugs,radiotherapyandradiomimeticagents.
Moreover,BERmodulationmayalsosensitizecancercellstotheeffectofchemother‐apeuticdrugsthatareabletogenerateROS[31,33].
Therefore,targetingBERwithinhibitorsNewResearchDirectionsinDNARepair496ofthemultifunctionalAPEndonuclease1andDNApolβisanattractivefieldtothedevel‐opmentofnoveltherapeuticcompounds.
SomestudieshavefoundderegulationofBERgenesintumours.
Forexamplepolβhasbeenshowntobeoverexpressedinavarietyoftumourcells[76].
N-methylpurineDNAglycosy‐lase(MPG)overexpression,togetherwithinhibitionofBER,sensitizesgliomacellstotheal‐kylatingagentTMZinaDNApolβ-dependentmanner,suggestingthattheexpressionlevelofbothMPGandpolβmightbeusedtopredicttheeffectivenessofBERinhibitionandPARP-mediatedpotentiationofTMZincancertreatment[77].
Werecentlyobservedanin‐creaseinexpressionoftheBERgenesMDB4andNTHL1inImatinibresistantK562leukae‐miacells,andknockdownoftheirexpressioninresistantcellsusingsiRNAdecreasedcellsurvivalaftertreatmentwithdoxorubicin[78].
Nevertheless,theinvolvementofderegulat‐edBERcomponentsinchemotherapyresistanceisnotcompletelyevidentatpresent,exceptforPARP,andtheAPendonucleases.
Thefollowingtextshalldescribeongoingresearchtar‐getingthesecomponentsoftheBERpathway.
ThemajorAPendonucleaseinmammaliancellsisapurinic/apyrimidinicendonuclease1/redox-factor-1(APE1/Ref-1,alsocalledAPEX1),andhasbeenfoundtobeelevatedinanumberofcancerssuchasovarian[79],prostate[80],osteosarcoma[81]andtesticularcan‐cer[82].
Over-expressionofAPE1invitroledtoincreasedprotectionagainstbleomycin[82].
ThuselevatedlevelsofAPE1incancercellshavebeenpostulatedtobeareasonforchemo‐therapeuticresistance[81,83,84].
InhibitionofAPE1hasbeenshowntoincreasecellkillingandapoptosisandalsotosensitizecancercellstochemotherapeuticagents,andthusAPE1isconsideredasamoleculartargetintherapeutics[85,86].
APE1endonucleaseactivityisindirectlyinhibitedbyblockedAPsitesthatresultfromthebindingofthesmallmoleculemethoxyamine(MX)totheDNA.
WiththeAPE1'ssubstrateunavailable,BERcannotproceedandthecytotoxicabasicsitesaccumulateinthecell,eventuallyleadingtocelldeath.
ThepromisingresultsfrominvitroandinvivoexperimentsshowingMXsensitizationtothecytotoxiceffectofTMZ[87-90],carmustine[91],pemetrexed[92]and5-iodo-2'-deoxyuridine(IdUrd)aswellasapotentiationofIdUrd-mediatedradiosensitization[93,94],inmultiplesolidtumoursmodels,providedtheproof-of-concepttoconductclinicaltrialswithMXasadjuvanttherapyofanticanceragents.
APhaseIclinicaltrialofpemetrexedandoralmethoxyaminehydrochloride(TRC102)inpatientswithadvancedrefractorycancerisalreadycompleted[95].
Accord‐ingtotheauthors,thisdrugiswelltoleratedafterdailyoraladministrationandpotenti‐atestheactivityofchemotherapy.
Safety,pharmacokineticandpharmacodynamicprofileofMXwasalsoevaluatedincombinationwithTMZinaPhaseIclinicaltrialforpa‐tientswithadvancedsolidtumours[96].
Currently,twoclinicaltrials(PhaseI)arere‐cruitingpatientstostudythesideeffectsandthebestdoseofMXtobeadministeredincombinationwithTMZandfludarabinephosphateinpatientswithadvancedsolidtu‐moursandrelapsedorrefractoryhematologicmalignancies,respectively.
InviewoftheemergingrolesofAPE1,manyeffortshavebeenmadetodevelopsmallmole‐culeinhibitorsthatcanbetranslatedtotheclinic.
Insilicobasedapproacheswithdesignofpharmacophoremodels[97,98]andhigh-throughputscreeningofseveralcommerciallyDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952497availablelibrariesofcompoundshavebeenperformedtoidentifyapharmacologicallyac‐tiveinhibitorforAPE1[86,99-102].
LucanthoneactsasadirectinhibitorofAPE1butalsointeractswithothercellulartargetsandtheassociatedtoxicityhinderstheirtherapeuticuse[103,104].
CRT0044876wasidentifiedbyafluorescence-basedhigh-throughputassayandshowedpromisingresultsininvitrostudies[105].
However,someauthorswerenotabletoreproducethereportedeffectsofthiscompound[85].
HypersensitivityofDNApolβ-nullcellstomethylmethanesulfonate(MMS),aDNA-meth‐ylatingagent,displayedanotherpotentialtargetinBER[106].
Severalsmall-moleculeinhibi‐torsofDNApolβhavebeenidentifiedandmanyofthesecompoundsarenaturalproducts,suchaskoetjapicacid(KJA),atriterpenoid.
PamoicacidwasoneofthefirstsyntheticsmallmoleculeinhibitorsofDNApolβtobecharacterizedandismoreactivethantheformercompound[107].
Nevertheless,theactuallyknowninhibitorsofDNApolβhavelowpoten‐cyandspecificitythatmakethemweakcandidatestodrugdevelopment(foracomprehen‐sivereviewsee[108]).
InviewofthepreclinicaldatathatsuggestanimportantroleofDNAPolβintherepairofchemotherapeutic-inducedDNAdamage,thedesignofeffectiveDNAPolβinhibitorsisanattractiveresearcharea.
InwhatconcernsPARP1,thisenzymeisaDNAdamagesensorthatbindstoDNAbreakstoactivatetherepairpathways.
PARP1isnotdirectlyinvolvedintherepairofthelesionsbutisessentialtosignalthedamageandtocoordinatethefunctionsofsever‐alBERandDSBrepairproteins.
PARPinhibitorshavebeenthoroughlydevelopedandseveralreviewspaperspublishedunderthistopic.
ForarecentcomprehensivereviewonPARPinhibitorsseeJavleetal[109].
PARPinhibitorswerefirstevaluatedinclinicaltri‐alsaschemosensitizers.
AfterAG014699combinationwithTMZ[110],otherPARPinhibi‐tors,specificallyINO-1001,ABT-888andAZD2281werealsotestedasadjuvanttherapyofmultipleanticanceragentssuchasgemcitabine,carboplatin,TMZorchemotherapeuticcombinations(e.
g.
cisplatinplusgemcitabine)[111].
Currently,severalPARPinhibitorsarebeingevaluatedinclinicaltrials,eitherincombinationwithchemotherapeuticdrugsorinmonotherapy[28,109,112-117].
Someofthesechemicalsshowedanenhancementofthetoxicityinnormaltissuesthatre‐quireddoseadjustmentsandoptimizationofthetherapeuticschedule.
Interestingly,pre‐clinicalandclinicaldatarevealedthatPARPinhibitorsassingleagentscouldbelesstoxictothenormalcellsandaremoreeffectiveinkillingBRCA1-andBRCA2-mutatedcancercellssincethesecellsaredefectiveinHR,thebackuppathwayresponsiblefortherepairofDSBsgeneratedafterPARPchemicalinhibition.
Similarly,mutationsinotherproteinsrelatedtotheDNAdamageresponse,suchasATMandPTENhavealsobeenassociatedtodefectsinDSBrepairandmaybeinvolvedinanincreasedsensitivitytoPARPinhibitors[118-120].
ThesefindingsledtoanovelpotentialtherapeuticindicationoftheDNArepairinhibitorsassingleagentsincancertherapywhichiscurrentlybeingevaluatedinclinicaltrials[121].
ThissyntheticlethalapproachwasalsoreportedinaninvitrostudywithAPE1inhibitorsinBRCAandATMdeficientcells[116,122].
Recently,negativeresultsfromthefirstphaseIIIclinicaltrialinbreastcancerpatientswithacombinationofiniparib(BSI-201)andgemcitabine/carboplatinwerereported[123].
TheNewResearchDirectionsinDNARepair498mechanismofactionofthisinhibitorisnotfullyunderstood,anissuethatshouldbefurtherclarified.
Nonetheless,promisingpositiveoutcomeshavealreadybeensuggestedwithotherPARPinhibitors[124,125].
AfurtherunderstandingofthecomplexPARPinteractome,thediscoveryofPARP1specificsmallmoleculeinhibitorsandanaccurateselectionofthebestcandidatestothetreatmentisstillneededtoimprovethequalityofinformationobtainedfrompreclinicalandclinicaltrialsandtopromotethedevelopmentofcurrentlyknownPARPinhibitorsaswelltodiscovernovelcompounds.
6.
TargetingNERindrugresistanceNERrepairsDNAlesionswhichalterthehelicalstructureoftheDNAmoleculeandin‐terferewithDNAreplicationandtranscription,suchasbulkyadductsandcross-linkingagents[2].
Briefly,NERconsistsoftherecognitionofDNAdamageanddemarcationofthespecificareaaffected,followedbytheformationofacomplextounwindthedam‐agedportionandexcisea24-32oligonucleotidesectionthatcontainsthelesion.
Finally,theexcisednucleotidesareresynthesizedandligated.
TwoNERsub-pathwaysexistwithpartlydistinctsubstratespecificity:globalgenomenucleotideexcisionrepair(GGR)sur‐veystheentiregenomefordistortinglesionsandtranscription-coupledrepair(TCR)fo‐cusesspecificallyinthetranscribedstrandofexpressedgenes,bytargetingdamagethatblockselongatingRNApolymerases.
Intotalmorethan30proteinsparticipateinNER[126].
ThegenesinvolvedinGGRareDNAdamagerecognitionbyXPC-HR23Bcom‐plex,lesiondemarcationandverificationbyaTFIIHcomplex,assemblyofapre-incisioncomplex(RPA,XPAandXPG),DNAopeningbyXPBandXPDhelicases,dualincisionbyERCC1-XPFandXPGendonucleases,releaseoftheexcisedoligomer,repairsynthesistofillintheresultinggap,andligationbyligaseI.
DefectsintheproteinsinvolvedinNERresultinthreeautosomalrecessivedisordersXP,CS,andTTD.
ThemostrelevantclassofchemotherapeuticsassociatedwithNERistheplatinum-basedgroupofagents.
Platinum-basedchemotherapyhasbeenusedforthetreatmentofawidevarietyofsolidtumoursincludinglung,headandneck,ovarian,cervical,andtes‐ticularcancerformanyyears[127].
TheseagentsinteractwithDNAtoformpredomi‐nantlyintra-strandcross-linkDNAadductsthattriggeraseriesofintracellulareventsthatultimatelyresultincelldeath.
Themoststudiedplatinumbasedcancertherapeuticsarecisplatinandthelesstoxiccarboplatinandoxaliplatin,buttherehasbeenaresur‐genceinthedevelopmentofplatinumbaseddrugs,andmoreplatinumbasedchemo‐therapeuticsareinclinicaltrials[128].
Thebasicmechanismofactionofcisplatin(andcarboplatin)involvescovalentbindingtopurineDNAbases:platinumbindingtotheN7positionoftheimidazoleringofthepu‐rinebasesofDNA—guanine(G)andadenine(A)—toformeithermonofunctionalorbifunctionaladducts.
Inthecaseofcisplatin,mostoccuronthesameDNAstrandandinvolvebasesadjacenttooneanother,andarethereforeknownasintra-strandadductsorcrosslinks,namelyGpG1,2intra-strand(60–65%ofalladducts)andApG1,2intra-DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952499strand(20–25%)whichprimarilyleadstocellularapoptosis[128].
TheseDNAlesionsarerepairedbytheNERpathway.
Cisplatinhasbeenusedsuccessfullyastherapytotreatmetastatictesticularcancerwith>90%curerate.
ThehighsensitivityoftesticulartumourcellsisattributedtoreducedDNA-re‐paircapacityinresponsetoplatinum–DNAadducts[129].
ExtractsfromtesticularcancercellshadlowconstitutiveNERcapacityand,inparticular,lowlevelsoftheproteinXPA[130].
FurtherstudieshaveshownlowlevelsofXPAandotherNERproteins(XPFandERCC1),intesticularcancers.
ThissuggestedthatreducingNERcapacityinacancerholdsthepotentialtosensitizethecancertocisplatin.
ParallelstudiesrevealedthatincreasedDNArepaircapacitywasacommonfunctionincancersthatwereinherentlyresistanttocis‐platinorthatacquiredresistancefollowingtreatment[130].
Clinicalstudiesinovariancancerpatientshavecorrelatedincreasedexcisionrepaircross-complementationgroup1–(ERCC1)mRNAlevelswithclinicalresistancetoplatinumbasedchemotherapy[131,132].
Inmetastaticcolorectalcancerpatients,higherERCC1ex‐pressionlevelswereconsideredaspredictiveforlowersurvivalrateswhentreatedwithox‐aliplatinincombinationwith5-fluorouracil,suggestingthatenhancedDNArepairdecreasestheefficacyofplatinum-basedtreatment[133].
Inanotherstudyasubgroupof761patientswithmetastaticlungcancertreatedwithaplatinumbasedcompoundwereretro‐spectivelyevaluatedbyimmunohistochemicalanalysisofERCC1.
Thisstudyshowedastat‐isticallysignificantsurvivalbenefitinpatientswithlowlevelsofERCC1whohadreceivedplatinumbasedchemotherapy,comparedtopatientswithlowlevelsofERCC1whodidnotreceivechemotherapyandpatientswithhighlevelsofERCC1whoreceivedcisplatinche‐motherapy[134].
Also,lowERCC1expressioncorrelatedwithprolongedsurvivalaftercis‐platinplusgemcitabinechemotherapyinnon-smallcelllungcancer(NSCLC)[135].
Hence,itishypothesizedthathighexpressionoftheERCC1genemightbeapositiveprog‐nosticfactor,andcouldpredictdecreasedsensitivitytoplatinum-basedchemotherapy.
Ex‐pressionofERCC1hasbeenusedtostratifypatientstreatedwithplatinumbasedchemotherapeuticswithsomesuccess,andalsotopredictimprovedsurvivalinplatinumtreatedpatients[136].
Nonetheless,resultsfromthepublisheddataareinconsistent.
Tode‐riveamorepreciseestimationoftherelationshipbetweenERCC1andtheprognosisandpredictiveresponsetochemotherapyofNSCLC,ameta-analysiswasperformedandresultsindicatedthathighERCC1expressionmightindeedbeafavourableprognosticandadrugresistancepredictivefactorforNSCLC[137].
Otherstudieswithdifferenttumour/chemotherapyassociationshaveshownthatERCC1mRNAexpressionintumoursmaybeapredictivemarkerofsurvivalforIrinotecan-resist‐antmetastaticcolorectalcancerreceiving5-FUandOxaliplatincombinationchemotherapy[133].
InthisstudypatientswhosetumourshadlowERCC1mRNAexpressionhadasignifi‐cantlylongermediansurvivalthanthosewithhighERCC1expression.
OthergenesinvolvedinNERhavebeenshowntoinfluencedrugresistance.
Forexample,increasedexpressionofexcisionrepaircross-complementationgroup4(ERCC4orXPF)wasobservedinhydroxycamptothecin(HCPT)treatedbladdercancertissuecomparedtoun‐NewResearchDirectionsinDNARepair500treatedsamples.
ComplementaryinvitrostudiesshowedthatenhancedERCC4expressiondecreasedthesensitivityofbladderT24cellsand5637cellstoHCPT,whereasaftergenesi‐lencingofERCC4thechemotherapeuticresistanceofbladdercancercellstoHCPTwassig‐nificantlydecreased[138].
SincetheNERpathwayiscrucialfortherepairofbulkyadductsandcross-linkingagentsinnormalcells,thedevelopmentandapplicationofNERinhibitorsinclinicalsettingsisscarce,althoughpreclinicaldatashowthatthemanipulationofthispathwaycouldbearelevantstrategyincancerchemotherapy.
Forexample,preclinicalstudieshavedemonstratedthatthechemotherapeuticactionoftheplatinumagentoxaliplatinisimprovedwhencombinedwithcetuximab,achimericIgG1monoclonalantibodytargetingtheepidermalgrowthfac‐torreceptor.
ThisantibodyhasbeenshowntoreducetheexpressionofERCC4andERCC1.
Aconcomitantincreaseintheaccumulationofplatinumandapurinic/apyrimidinicsitesonDNAduringoxaliplatintreatmentwasobserved,thusleadingtoanincreaseinapoptosis[139,140].
Theseinterestingresultsaresuggestivethattargetingotherpathwaysthatregu‐lateexpressionofDNArepairgenescouldbeapromisingstrategy.
7.
HRanddrugresistanceHRrepairsDSBs,whichoccurthroughexposuretovariouschemotherapeuticagents,in‐cludingIR,topoisomeraseinhibitorsandDNAcrosslinkingagents(e.
g.
mitomycin,campto‐thecins,etoposide,doxorubicin,daunorubicinandbleomycin).
HRisalsorecruitedtorestartstalledreplicationforksandtorepairICL,therepairofwhichalsoinvolvestheFAproteincomplex.
HRensurestheaccuraterepairofDSBsbyusingahomologousundamagedDNAstrandfromanintactsisterchromatidasatemplateforDNApolymerasetoextendpastthebreak,andisthusrestrictedtolateSandG2ofthecellcycle.
ComponentsofHRincludetheRADgroupofproteins(includingRAD50,RAD51,RAD52,andRAD54),RPA,XRCC2,XRCC3,andtheBRCAproteins.
Briefly,HRoccursthroughpre-synapsis,preparationofarecombinationproficientDNAend;synapsis,formationofajointmoleculebetweenthere‐combinationproficientDNAendandadouble-strandedhomologoustemplateDNA;post-synapsisandresolution,repairofDNAstrandsandseparationoftherecombinedDNAmolecules[19].
DSBscanalsoberepairedbyNHEJthatdonotutilizesignificanthomologyatthebrokenends.
InNHEJ,DSBsarerecognizedbytheKuproteinthatthenbindsandac‐tivatestheproteinkinaseDNA-PKcs,leadingtorecruitmentandactivationofend-process‐ingenzymes,polymerasesandDNAligaseIV.
WhereasHRisrestrictedtolateSandG2,NHEJfunctionsinallphasesofthecellcycleandligatesbrokenDNAendswithouttheneedofanundamagedtemplate.
FollowingDNAlesionsinitialcheckpointsignallingisperformedbythekinasesATRandATM,twophosphatidylinositol3-kinasefamilymembers.
Activationofthesekinasesleadstoactivationoftheeffectorkinases,checkpointkinases1and2(Chk1andChk2;serine/threoninekinases).
TheactivatedeffectorkinasesarethenabletotransientlydelaycellcycleprogressionthroughtheG1,S,ortheG2phasessothatDNAcanbeefficientlyrepaired.
TheDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952501ATM/Chk2pathwaypredominantlyregulatestheG1checkpointandtheATR/Chk1path‐waytheSandG2checkpoints.
However,thereiscross-talkbetweenthepathwaysimplyingaroleforbothATRandATMpathwaysinallcellcyclecheckpoints.
Inadditiontodirectlyregulatingthecellcycle,thepathwaysalsoaffectDNArepair,transcription,chromatinreg‐ulation,andcelldeath.
Manydetailsofthesepathwaysarenotfullyknown.
OneconsequenceofDSBsisthelocalizedalterationofchromatinadjacenttoDSBsinordertofacilitaterecruitmentofrepairproteins.
Forexamples,ATMnotonlyphosphorylatesDNArepairproteinsrecruitedtoDNAendsbutalsothehistonevariantH2AXinnucleo‐somesadjacenttoDSBs,whichisalsophosphorylatedbyDNA-dependentproteinkinase(DNA-PK),anotherproteinkinaseactivatedbyDSBs.
PhosphorylatedH2AX(knownasγ-H2AX)aroundDSBsfacilitatestherecruitmentofanumberofDNArepairproteinsandchromatinmodulatingfactors.
Thepresenceoflargepatchesofγ-H2AXaroundaDSBhasmadeitsdetectionbyfluorescenttaggedantibodiesabiomarkerforDSBs[141,142].
ThereisaccumulatingevidencefortheexistenceofHRdefectsnotonlyinfamilialcancersbutalsoinsporadiccancers.
Mutationsorepigeneticalterationshavebeenobservedinsev‐eralgenesknowntobeinvolvedinHRregulationandrepair,suchasBRCA1andBRCA2.
FunctionalanalysisofhumancancertissuesandcancercelllineshasrevealedHRdeficien‐cy,chromatid-typechromosomalaberrations,severeICLhypersensitivity,andimpairedfor‐mationofdamage-inducedRAD51foci.
Forexample,althoughgeneticmutationsinBRCA1orBRCA2areonlyrarelyfoundinsporadictumors,incontrasttofamilialbreastandovari‐ancancers,epigeneticgeneinactivationoftheBRCA1promoterisafairlycommoneventinsporadicbreastcancers,withaberrantmethylationbeingdetectedin11to14%ofcases[143].
Non-triple-negativesporadicbreastcancersmayalsoharborHRdefects.
Ithasbeensuggestedthat~20%ofthesecancersaredefectiveinHRasmeasuredbyanimpairedabilitytomountRAD51fociinresponsetochemotherapy[144].
Thereisemergingevidencethatapproximatelyuptoonefifthofnon-familialbreastcancersharbourHRdefectsthatmaybeusefultargetsfortherapy.
TheBRCA1andBRCA2proteinsareinvolvedinHR,inassociationwithFAproteins,form‐ingacomplexDNAdamageresponsenetwork[145].
BRCA1expressionlevelshavebeendemonstratedtobeabiomarkerofsurvivalfollowingcisplatin-basedchemotherapyforNSCLCandovariancancer,suggestingthatthisgenecouldbeinvolvedinresponsetoplati‐numtherapy[146,147].
InvitrostudiesindicatethatlossofBRCA1orBRCA2increasessen‐sitivitytoagentsthatcauseDSBssuchasbleomycinand/orICLsincludingplatinumagents.
Conversely,lossofBRCA1orBRCA2mayincreaseresistancetomicrotubuleinterferingagentssuchastaxanesandvincristine[148,149].
Incontrast,BRCA1mayincreasesensitivitytospindlepoisonsbyactivatingthemitoticspindlecheckpointandsignallingthroughaproapoptoticpathway.
ThisdualroleofincreasingapoptosisandthereforesensitivitytospindlepoisonsandalsopromotingDNArepairandcellsurvivalaftertreatmentwithDNA-damagingdrugsmayinfluencetheresponseofbreastandovariancancercellstotreatment[150].
Chemotherapyinbreastandovariancancersisattainedbytreatmentwithplatinumbasedcompoundsandanthracyclinesandalsotaxanes,allofwhichinducebothNewResearchDirectionsinDNARepair502SSBsandDSBs.
EffortsareunderwaytouseBCRA1asapredictivemarkerforchemothera‐pycustomizationandresponse[151].
Regardingothertypesofcancer,BRCA1promoterhypermethylationisalsofoundinap‐proximately5-30%ofsporadicovariancancers.
Also,mutationsinBRCA1andBRCA2haverecentlybeenfoundinupto20%ofunselectedovariancancers[152].
Thus,theseHRdefi‐cientcancersareviabletargetsforsyntheticlethalityapproacheswithPARPinhibitors.
De‐fectsintheFA/BRCApathwayaswellasATMdefectshavebeendescribedinavarietyofothermalignancies,suchasprostaticadenocarcinoma,colorectalcancer,leukaemia,lym‐phoma,andmedulloblastoma[153,154].
However,itremainstobeseenwhetherthesede‐fectscanbetargetedeffectivelyintheclinic.
Single-agentchemotherapywithanitrogenmustard,usuallyChlorambucil,isthestandardinitialtherapyforChroniclymphocyticleukaemia(CLL)andatleast60–80%ofpatientsre‐spondbuteventuallyallpatientsbecomeresistanttotheseagents.
XRCC3proteinlevelsandDNA-damageinducedRAD51focicorrelateswithchlorambucildrugresistanceinlympho‐cytesfromCLLpatientsandwithmelphalanandcisplatinresistanceinepithelialtumorcelllines,indicatingthatincreasedHRcanbeinvolvedindrugresistancetotheseagents[155].
AnothercomponentoftheHRpathway,RAD51,hasbeenfoundtobeincreasedinex‐pressioninawiderangeofhumantumors,mostlikelycontributingtodrugresistanceofthesetumors.
Over-expressionofRAD51indifferentcelltypesleadstoincreasedhomol‐ogousrecombinationandincreasedresistancetoDNAdamagingagentstodisruptionofthecellcycleandapoptoticcelldeath.
RAD51expressionisincreasedinp53-negativecells,andsinceTP53isoftenmutatedintumorcells,thereisatendencyforRAD51tobeoverexpressedintumorcells,leadingtoincreasedresistancetoDNAdamageanddrugsusedinchemotherapies[156].
Chronicmyeloidleukaemia(CML)celllinesexpressingthefusionproteinBCR-ABL1uti‐lizeanalternativenon-homologousend-joiningpathway(ALTNHEJ)torepairDSBs.
TheexpressionlevelsofPARP1andDNAligaseIIIαservedasbiomarkerstoidentifyasubgroupofCMLpatientswhomaybecandidatesfortherapiesthattargettheALTNHEJpathwaywhentreatmentwithTKIshasfailed[157].
Tamoxifen-andaromatase-re‐sistantderivativesofMCF7cellsandEstrogenReceptor-/ProgesteroneReceptor-(ER-/PR-)cellshavehighersteady-statelevelsofDNAligaseIIIαandincreasedlevelsofPARP1,anotherALTNHEJcomponent.
Notably,therapy-resistantderivativesofMCF7cellsandER-/PR-cellsexhibitedsignificantlyincreasedsensitivitytoacombinationofPARPandDNAligaseIIIinhibitorsthatincreasedthenumberofDSBs.
Thus,ALTNHEJmaybeanoveltherapeutictargetinbreastcancersthatareresistanttofrontlinetherapiesandchangesinNHEJproteinlevelsmayserveasbiomarkerstoidentifytumorsthatarecan‐didatesforthistherapeuticapproach[158].
AnotherinterestingapproachinthisfieldistotargetcomponentsoftheDNAdamageresponse,namelyDNAdamagesignallingandcell-cyclecheckpoints[34].
Themembersofthephosphatidylinositol(PI)3-kinase-like(PIKK)familyperformcrucialrolesintheactivationofDSBrepairpathways,namelyinHRandNHEJ.
ATM,aPIKKfamilymem‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952503ber,isaDSBsignallingproteinmainlyimplicatedinthephosphorylationofeffectorpro‐teinsfromHR.
ATMhasbeenalsoinvolvedintheregulationofNHEJ.
KU55933,2-morpholin-4-yl-6-thianthren-1-yl-pyran-4-oneisaspecificandpotentsmall-moleculeinhibitorofATMidentifiedbyscreeningofacombinatoriallibrary.
Preclinicalstudieshaveshownanincreaseinthecytotoxicityofmultiplechemotherapeuticdrugsasdoxor‐ubicin,etoposide,camptothecinandionizingradiation[159,160]whiletheUV-inducedcellulareffectswerenotmodified.
Morerecently,KU60019,animprovedanalogueofKU55933,wasdeveloped.
Besidesitsradiosensitizingproperties,invitrostudiesrevealedthatKU60019mayalsoimpairthemigrationandinvasionoftumorcellsbyinhibitingATM-mediatedAKTphosphorylation[161].
DNA-PKisalsoatargettothedevelopmentofchemo-andradiosensitizers[162].
Infact,theidentificationofspecificsmallmoleculemodulatorsofDNA-PK[163-165],namelyNU7441andNU7026,wasshowntopotentiatetheeffectsofionizingradiationaswellaschemother‐apeuticagentsinhumantumorcelllinesandininvivoxenograftmodels.
AnotherexampleisthedevelopmentofAZD7762,whichpotentlyinhibitsChk1andChk2,abrogatesDNAdamage-inducedSandG2checkpoints,enhancestheefficacyofgemcita‐bineandtopotecan,andmodulatesdownstreamcheckpointpathwayproteins[166].
Thisagenthasbeenevaluatedinclinicaltrials,howeverduetoaninadequateresponsethedrughasbeendiscontinuedin2011(http://www.
astrazenecaclinicaltrials.
com).
8.
MicroRNAsandchemotherapyresistanceMicroRNAs(miRs)aresmallnon-codingRNAs(19to25nucleotides)thatregulategeneexpressionbybindingto3'untranslatedregion(UTR)ofseveralmRNAs,thusblockingtranslation.
Recently,itwasalsoshownthatmiRscanactbybindingtoopenreadingframesor5'UTRofmRNAs,asrevisedbyIorioandCroce[167].
DuetosmallsizeandincompletecomplementaritytomRNA,onemiRcanhaveawidespreadeffectonthetranscriptomeofacell,actingasahallmarkofseveraldiseases,includingcancer.
Nu‐merousstudieshavebeenperformedregardingbiogenesisandfunctionofmiRs,beingrevisedelsewhere[168-170].
InvitroandinvivostudieshavesuggestedthatmiRNAsmightbeusefulasdiagnosticandprognosticmarkers,andrecentdatasuggestthatmiR‐NAprofilingcanbeusedfortumortyping.
AlthoughitiswellestablishedthatmiRshaveanimportantroleincancer,thecomplexityoftheiractionremainstobeunderstoodandquestionsregardingtheiruseascancertherapyneedfurtherinvestigation.
ThestrongpleiotropyofmiRsinderegulatingnormalcellularhomeostasisduetomisexpression,hasledinvestigatorstobelievethattheyarevaluabletar‐getsforcancertherapyandconsequentlyfordrugresistance.
Twomajorapproachesforus‐ingmiRsastherapeuticscanbedescribed.
First,miRscanbeusedassinglemoleculesorcombinedinordertotargetoneormultipletranscripts.
Inthisapproach,amiRorasetofmiRsareantagonizedormimickedtoaltermiRlevelsandconsequentlychangetheproteinNewResearchDirectionsinDNARepair504outcomeinacancercell.
Second,miRscanactasmodulatorsofcellsensitivityforcancertherapy[167,171].
Thissecondapproachwillbeourfocus.
ManystudiesregardingmiRsexpressionpatternsincancercellshavebeenperformed.
ThesestudiesnotonlyallowinvestigatorstodeterminenovelbiomarkersforabetterandeasilyprognosticationofseveraltypesofcancerbutalsothefunctionalroleofthesamemiRs.
ThesecangiveustheknowledgeifthelossorgainofmiRfunctioninter‐fereswiththeoriginalbalanceofproteinlevelswhichmaybeimportant,butnotonly,indrugresponseandconsequentlyleadtodrugresistance.
SincemiRsexpressionseemstobetissue,gradeandstagespecific,theectopicexpressionorrepressionofmiRsinconjugationwithcancertherapyseemspromising.
Forthatreason,recentstudiesthatevaluatemiRexpressionprofilesofsensitiveandresistantcelllineshavebeenmadeinordertofindthekeymiRsignaturesrelatedtodrugresponse,whichnotonlypromotefurtheranalysisofthemechanismsofcancerdrugresistance,butalsoallowthediscov‐eryofnewdrugtargetsandindividualizedmedicine.
AlthoughthestudyofthetherapeuticpotentialofmiRsisstillrecent,severalstudieshavebeenpublishedandcompiled.
Forexample,Tianetal.
[172]andKutanzietal.
[173],publish‐edcompilationsofseveralstudiesreportinginfluenceofmiRsinmechanismsofdrugresist‐anceandhowtheycanmodulatedrugresponseinbreastcancer.
WithregardtomiRsandmodulationofdrugresistancethroughregulationofDNAdamageandrepairgenes,studiesarescarce.
ItisknownthatmiRshaveanimportantroleinDNAdamageresponse,whichincludesDNArepair[174,175].
OneexamplehowmiRscaninflu‐encedrugresistancethroughDNArepairisdemonstratedbyValerieetal.
[73].
TheauthorsshowedthatmiR-21targetsMSH2andconsequentlyinducesresistanceto5-FUincolorectalcancer.
SincemiR-21hasapleiotropiceffect,itispossiblethatitcouldregulateothergenesassociatedwithdrugresistance.
However,theimpactofMSH2seemstobeofextremeim‐portanceonacquired5-FUresistancesincewhenknockedoutcellsforMSH2aretransfectedwithmiR-21,cell-cyclearrestorapoptosisisnotaltered.
Theseresultsshowthattheinhibi‐tionofmiR-21actionmightrepresentanimportanttreatmenttoovercome5-FUresistance.
AcorrelationbetweenmiR-21andMSH2inbreastcancerwasalsofound[176].
Itisrecog‐nizedthatTGF-βisapromoterofmiR-21processingthroughtheinteractionwiththeSMADandDROSHAcomplex.
Ontheotherhand,MSH2isaproventargetofmiR-21.
Thus,TGF-βinhibitsMSH2geneexpressionandconsequentlyincreasesdrugresistance.
Indeed,tofindoutifTGF-βcontributestodrugresistancethroughMSH2,theauthorstestedtheresponseofbreastcancerMDA-MB-231celllinetocisplatin,methylmethanesulfonate(MMS)anddoxorubicininthepresenceandabsenceofTGF-β.
ExposuretoTGF-βfor24hincreasedcellviabilityupontreatmentwiththeseDNAdamagingagentsandknockdownofMSH2in‐ducedresistancetobothcisplatinanddoxorubicin.
Incontrast,transfectionoftheanti-miR-21enhancedtheeffectofcisplatininMDA-MB-231cells.
AnotherexampleofmiRinfluenceinDNArepairandconsequentdrugresponseismiR-182thattargetsBRCA1.
MoskwaandcolleaguesshowedthatectopicexpressionofmiR-182re‐pressesBRCA1proteinexpressionandsensitizesbreastcancercellstoPARPinhibitors[177].
However,PARPinhibitorsaremostlyusedinpatientswithBRCA1inheritedmuta‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952505tions.
Therefore,thequestionifPARPinhibitorsareusefultherapeuticdrugsinsporadicbreastcancerrises.
Theoretically,ifadministratedwithBRCA1repressorssuchasmiR-182,PARPinhibitorscanhavethesameeffectasininheritedbreastcancer.
Furtherstudiesneedtobedoneinordertoclarifythisissue.
Asdescribedpreviously,MGMThasDNArepairactivityinsofarasitcanremovemutagen‐icO6-alkylguanineinducedbyalkylatingagents.
AlthoughTMZhasbeenwidelyusedinglioblastomamultiforme(GBM),manypatientsbecomeorareresistanttothischemothera‐pyagent,sinceMGMTcanrepairtheDNAdamageinducedbyTMZ.
Epigeneticregulationmechanisms,suchasmethylationoftheMGMTgenepromotercansensitizecancercellstoalkylatingchemotherapeuticdrugs.
GlioblastomapatientswithpositivemethylationstatusofMGMTgenepromoterhavebeenreportedtopresentabetterresponsetoTMZtreatment[44],buttheseresultshavenotbeenconfirmedbyotherstudies,andthereforeresultsareambiguous[178].
Indeed,somepatientswithunmethylatedstatusofMGMTpromotergenealsohavegoodresponsetoTMZ,whichpointsouttootherregulatorymechanismsofMGMTexpression[179].
Thus,miRsappearasgoodalternativeregulationcandidatesofMGMTexpressionlevels.
RecentevidencealsosuggeststhatthemiR-181familymightbeassociatedtodrugresponse[180].
Theauthorsfoundthatglioblastomapatientswithlowex‐pressionofmiR-181bandmiR-181chaveabetterresponsetoTMZ.
Onthecontrary,miR-181dseemstopost-transcriptionallyregulateMGMTsincebothdirectlyinteractandin‐verselycorrelateinrelationtoexpressionlevels[181].
ThisfactisimportantbecauseitcouldbeapredictivebiomarkerforchemotherapyresponseinGBM.
LakomyandcollaboratorsfoundthathighexpressionofmiR-195andmiR-196bissignificantlyassociatedwithlongersurvivalofGBMpatientsandmiR-21andmiR-181cwithhighriskGBMpatients[182].
HowevernoneofthesemiRswereassociatedwithMGMTgenepromoterstatus.
AltogetherthepotentialforuseofmiRsincancertherapyishigh,soarethechallenges,sinceeachmiRcantargetuptohundredsofmRNAtargets.
Therapidelucidationoftheroletheyplayincancersuggestthattranslationofthisknowledgewillrapidlyreachtheclinic.
9.
PhytochemicalsasalternativetherapiesagainstdrugresistanceAsdiscussedpreviously,frequentlynoveltherapeuticsthatshowpromisingresultsinpre‐clinicalassaysrevealunacceptabletoxicityinclinicaltrials.
Sincecancercellsfrequentlypresentderegulationofmultiplecellularpathways,targetingmultiplepathwaysseemsmorepromisingthanusingsingleagentsthattargetsinglepathways.
Inrecentyearsnaturaldietarycompoundssuchascurcumin,resveratrolandsoyisoflavonessuchasgenistein,havereceivedattentionduetothefactthattheyfrequentlytargetmultiplecellsignallingpathways,includingthecellcycle,apoptosis,proliferation,survival,invasion,angiogenesis,metastasisandinflammation.
Thustheiruseinchemopreventionhasgainedattention[183,184].
Additionally,sincemostofthecancerdrugsdevelopedhavebeendeliberatelydirectedtowardspecificmoleculartargetsthatareinvolvedinonewayoranotherinenablingpartic‐ularcellularfunctions,inresponsetomonotherapycancercellsmayreducetheirdepend‐NewResearchDirectionsinDNARepair506enceonaparticularproficiency(e.
g.
asinglerepairpathway),becomingmoredependentonanother,thuscontributingtoacquiredrugresistance.
Thus,asanalternativeapproach,se‐lectiveco-targetingofmultiplecoreandemerginghallmarkproficienciesinmechanism-guidedcombinationscouldresultinmoreeffectiveanddurabletherapiesforhumancancer[185].
Phytochemicalscanbehighlypleiotropic,modulatingnumeroustargets,includingtheactivationoftranscriptionfactors,receptors,kinases,cytokines,enzymes,andgrowthfac‐tors[186].
Thereforecurrenteffortsarehighlyengagedindiscoveringnaturalplant-basedchemicalsthatcouldassistinthefightagainstdrugresistance.
ForexamplesoyisoflavonesinhibitedAPE1expressioninprostatecancercellsinatime-anddose-dependentmanner,whereasIRup-regulatedexpressionofthisBERgene,inre‐sponsetoDNAdamage[187-190].
PretreatmentofcancercellswithsoyisoflavonesinhibitedtheincreaseinexpressionofAPE1,andenhancedtheefficacyofchemotherapyandradiationtherapyofmultiplecancersmodelsinvitroandinvivo,possiblythroughdown-regulationofthisDNArepairgene[188].
Anotherphytochemical,resveratrol,wasal‐soshowntoinhibitAPE1endonucleaseactivityandrendermelanomacellsmoresensitivetotreatmentwiththealkylatingagentdacarbazine[191].
Thusbothresveratrolandisofla‐vonessuchasgenisteincanhavetherapeuticpotentialasanAPEinhibitor.
Aseriesofana‐logsofresveratrolhavebeengeneratedinrecentyears,whichexhibitincreasedpotencyand/orarangeofselectiveactivitiescomparedtotheparentalcompoundresveratrol,andpossiblyimprovedpharmacokineticproperties[192].
Aclinicaltrialofresveratrolincoloncancerhasrecentlybeencompleted(http://www.
clinicaltrials.
gov).
ResveratrolcanalsoincreaseBRCA1andBRCA2expression,althoughnoeffectisseenattheproteinlevel[193].
AnincreaseinBRAC1expressioncanleadtoincreasedarrestofcellsintheG2phase,thusmakingthemmuchmoresensitivetoconventionaltherapy.
Onecommonche‐motherapeuticdrugisdoxorubicin,whichpredominantlyinducesDNAdamageinG2phasecells[194].
Resveratrol,curcuminandthenaturallyoccurringflavolignandeoxypodophyllo‐toxin[195]caninduceG2/Mcellcyclearrest,andaltertheexpressionofcellcycleregulatoryproteins,thusallowingdoxorubicintoinducelesionsandasaconsequenceenhancetheapop‐toticeffect[186,196,197].
LeCorreetal.
,alsodemonstratedthatresveratrolhasaneffectontheexpressionofgenesimplicatedintheregulationofBRCA1proteinfunctionsandinmultiplenuclearprocessesmodulatedbyBRCA1inhumanbreastcancerandfibrocysticbreastcells[198].
OneofthemechanismsbywhichresveratrolcanenhanceBRAC1expressionisbyassoci‐ationwithBRCA1,repressingthearomatichydrocarbonreceptor(AhR).
AhRbindsmanynat‐uraldietarybioactivecompoundsthereforecombinationdietswithAhRantagonistsmayoffertheadvantageofhighercancerpreventionefficacies[199].
InHR-deficienttumours,patientswithheterozygousmutationsintheHRgenesBRCA1andBRCA2developbreastandovariantumourswithfunctionallossofHRactivity,anddeficiencyinthispathwaymaydictatethesensitivityoftumourstocertainDNA-damagingagentsandthismaybeanotherpossibleap‐proachtotestnaturalcompoundstoovercomeresistance,andoncemoreenhancecombinato‐rystrategiestooptimizetreatmentoutcome[32].
Recentlyanextractofneemleaveswascharacterizedandasignificantup-regulationofgenesassociatedwithmetabolism,inflammationandangiogenesis,suchasHMOX1andDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952507AKRwasobserved.
Howevergenesassociatedwithcellcycle,DNAreplication,recombina‐tion,andrepairfunctionsweredown-regulated[200].
Onestudyanalysed531compoundsderivedfromplantsandfoundnocorrelationwithgenesinvolvedinNER(ERCC1,XPA,XPC,DDB2,ERCC4,ERCC5)orBER(MPG,APE1,OGG1,XRCC1,LIG3,POLB).
Itispossiblethatnaturalcompoundsmaytargetdifferentmolecularpathwaysfromthoseofstandardanti-tumordrugs,henceifDNArepairisinvolvedinthedevelopmentofresistancetoestab‐lishedanticancerdrugs,naturalcompoundsmaybeattractivesourcesofnoveldrugssuita‐bletotreatdrugresistanttumours,withtheadvantageofhavingreducedsideeffects[201].
Likewise,mostplantderivativescanactasantioxidantsandsomeofthemcanincreasehu‐manMGMTexpression(e.
g.
curcumin,silymarin,sulforaphaneandresveratrol)beyonditssteady-statelevels,havingaroleincancerchemoprevention[202].
Additionally,bothBRCA1andMGMTgenesaresusceptibletohypermethylation,andgreenteapolyphenolsandbioflavonoidshavebeenshowntoreversetheeffectsofDNAhypermethylation[203].
Theseresultssuggestthatsomedietarycompoundsmayhaveapotentialdemethylat‐ingeffect,andcouldbepromisingadjuvantstochemotherapyindrugresistantsettings.
Anotherissueincancerchemotherapyistheuseofmonotherapyvscombinedtherapy,andseveralstudieshavebeenperformedregardingpossiblecombinatorychemotherapywithnat‐uralcompounds(lessaggressivethanthemajorityofchemotherapeuticdrugs),albeitinpre‐clinicalsettings,e.
g.
silibininextract[204],ixabepilone[205]andcurcumin[206].
Someoftheseagentsarebeingevaluatedinclinicaltrials.
Silibininstronglysynergizedthegrowth-inhibito‐ryeffectofdoxorubicininprostatecarcinomacells,whichwasassociatedwithastrongG2-Marrestfollowedbyapoptosis[204].
Ixabepilone,ananalogueofthenaturalproductepothiloneB,isalreadyindicatedforthetreatmentoflocallyadvancedormetastaticbreastcancerintheUS.
InaphaseIIItrialinwomenwithlocallyadvancedormetastaticbreastcancerthatwerepretreatedwith,orresistantto,anthracyclines(e.
g.
doxorubicin)andresistanttotaxanes,pro‐gression-freesurvivalwassignificantlylongerinixabepilonepluscapecitabinerecipientscom‐paredwithrecipientsofcapecitabinemonotherapy[205].
Combinationtherapyusingcurcuminwithgemcitabine-basedchemotherapy,inaphaseI/IIstudy,inpatientswithpancre‐aticcancerwarrantsfurtherinvestigationintoitsefficacy[206].
Finally,aninterestingrecentdevelopmentconcernstheobservationthatmiRscouldberegu‐latedbynaturalagents,leadingtotheinhibitionofcancercellgrowth,epithelialtomesenchy‐maltransition(EMT),drugresistance,andmetastasis[207].
Formostepithelialtumors,progressiontowardmalignancyisaccompaniedbyalossofepithelialdifferentiationandashifttowardmesenchymalphenotype[185].
DuringtheacquisitionofEMTcharacteristics,cancercellslosetheexpressionofproteinsthatpromotecell-cellcontact,suchasE-cadherinandγ-catenin,andgaintheexpressionofmesenchymalmarkers,suchasvimentin,fibronectin,andN-cadherin,leadingtoenhancedcancercellmigrationandinvasion.
Ithasbeenshownthatdown-regulationorthelossintheexpressionofthemiR-200familyisassociatedwithEMT.
Gemcitabine-resistantpancreaticcellshavingEMTcharacteristicsshowedlowexpres‐sionofthemiR-200familyandmiR-200islostininvasivebreastcancercelllineswithmesen‐chymalphenotype.
HencetheinterestingobservationthatisoflavonecouldinducemiR-200expressioningemcitabine-resistantpancreaticcells,resultinginalteredcellularmorphologyNewResearchDirectionsinDNARepair508frommesenchymal-to-epithelialappearanceandinducedE-cadherindistributionthatismoresimilartoepithelial-likecells.
Likewise,let-7hasbeenfoundtoregulatecellproliferationanddifferentiation,andinhibittheexpressionofmultipleoncogenes,includingrasandmyc,andagainitwasobservedthatisoflavonecouldsignificantlyup-regulatetheexpressionoflet-7family,suggestingthatthisphytochemicalcouldreverseEMTcharacteristicsinpartduetotheup-regulationoflet-7[207].
Otherreportshaveshownthatcurcumin,isoflavone,indole-3-car‐binol(I3C),3,3′-diindolylmethane(DIM),()-epigallocatechin-3-gallate(EGCG)orresveratrol,canaltermiRNAexpressionprofiles,leadingtotheinhibitionofcancergrowth,inductionofapoptosis,reversalofEMTphenotype,andincreasingdrugsensitivity[208].
ItremainstobeseenifphytochemicalscanaffectmiRsthatregulateDNArepairpathways,butsinceanygivenmiRcantargetseveraltranscripts,thisregulationishighlylikely.
Over‐all,naturalcompounds,mayhaveanimportantroleinchemopreventionandincombinedtherapy,andmaypreventresistancetochemotherapy[188,189,208-210].
10.
ConclusionandfuturedirectionsAsdiscussedinthischapter,theultimatetargetofchemotherapyandradiotherapyisthecancercell,anduseofDNAdamagingagentsisjustifiablesincemostofthesecellsarehigh‐lycyclingcells.
ThetargetingofDNArepairpathwaysisbutoneofthemanystrategiesde‐velopedinthefightagainstcancer.
CancercellsfrequentlypossessalteredDNArepaircapacities,andthiscanbeputtouseintheclinic.
ThusthequestforspecifictherapiesthattargetDNArepairhasproducedmanypotentiallyusefulagents(Table1).
Usingsuchagentscantheoreticallyincreasetheefficacyofexistingchemotherapyand/orradiotherapy.
Nevertheless,thesamedifficultiesencounteredbyallotheralternativestrategiesarealsoarisingwhenwedisruptDNArepairprocesses.
ThesuccessoftheseagentsultimatelywilldependonourbasicknowledgeofthevariousDNArepairprocessespresentinagivencelltypeortissue.
NotallDNArepairpathwaysarepresentinalltissues,asevidencedbythefactthatmutationsinspecificpathwaysgiverisepreferentiallytocertaintumourtypesandnotothers.
Secondly,thesuccesswillalsode‐pendonthespecificgenomicandgeneticlandscapeofeachtumour,implyingthatdifferentcombinationsofinhibitorsandchemicalagentsshallhavetobetailoredtoeachtumour.
Wearestillfarfromachievingthisgoal,butgreatstrideshavebeentakeninthepastyears.
Thirdly,weshallhavetoredirectthestrategytodiscovera"cureforcancer"andinsteadfollowstrategiesthatallowustoaccompanytheinevitableandinexorableevolutionofthecancercellandconsistentlyfindandimplementmoreandmoretargetedtherapies,evenifthesestrategiesleadustoreturntoabandonedtherapies.
Theresurgenceofdrugholidays,inwhichatherapyisabandonedtemporarilytobetakenupafteracertainperiod,notun‐likewhatcanbeadoptedwithantibiotics,isonesuchstrategy.
Inthiscasetheabsenceofaselectivepressureimposedbyaspecificagentmayleadcancercellstoloseresistancetothisagent,makingthemagainvulnerabletothesameagent.
Thisstrategyhasbeenfollowedincertaincancersandcouldbeadaptedinothers,withtheadvantageofofferingreducedtimeonchemotherapy,reducedcumulativetoxiceffects,andimprovedqualityoflife[211,212].
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952509TargetDrugConditionortumorCombinationtherapyagent(s)Phaseofclinicaltrialplanned,ongoingorrecentlycompleted*ReferenceMGMTO6-BenzylguanineMultipleMyelomaandPlasmaCellNeoplasmGlioblastoma,GliosarcomaMelanomaColorectalCancerCarmustineTemodarCarmustineCarmustinePhaseIIcompletedPhaseIIcompletedPhaseIIcompletedPhaseIIcompletedwww.
cancer.
govPARP1AZD-2281/KU59436(Olaparib)TripleNegativeBreastCancerTripleNegativeMetastaticBreastCancerKnownBRCAOvarianCancerorKnownBRCA/TripleNeg.
BreastCancerCisplatinPaclitaxelPhaseI/IIactivePhaseI/IIcompletedwww.
astrazeneca.
comAG014699/PF-01367338(Rucaparib)SolidtumorsMelanomaTemozolomideVariousagentsPhaseIcompletedPhaseIIongoingwww.
pfizer.
comINO-1001MelanomaTemozolomidePhaseIterminatedwww.
inotekcorp.
comBSI-201/(Iniparib)UterineCarcinosarcomaCarboplatin,Paclitaxel,PhaseIIactivewww.
biparsciences.
comwww.
sanofi.
comBreastCancerGemcitabine/CarboplatinPhaseIIcompletedPhaseIIIactiveABT-888/(Veliparib)BreastcancerCarboplatinTemozolomidePhaseIIactivewww.
abbott.
comProstateCancerTemozolomidePhaseIactiveMelanomaTemozolomidePhaseIIactiveVariouscancersVariousagentsPhaseI/IIactiveMK4827SolidBRCAOvarianSingleagentVariousagentsPhaseIongoingwww.
merck.
comCEP-9722SolidtumoursTMZVariousagentsPhaseIwww.
cephalon.
comwww.
tevapharm.
comGPI1016/E7016SolidtumoursTMZVariousagentsPhaseIwww.
eisai.
comLT673HematologicalcancersSolidtumoursVariousagentsPhaseIongoingwww.
bmrn.
comNMS-P118Preclinical;highlyselectiveagainstPARP-5(tankyrase)www.
nervianoms.
comBERMethoxyamine/TRC-102AdvancedrefractorysolidcancersHematologicalcancersPemetrexedTMZFludarabinePhaseIactivePhaseIongoingwww.
traconpharma.
comATMKinaseKU55933Preclinicalwww.
astrazeneca.
comCHK1AZD7762www.
astrazeneca.
comPF-00477736www.
pfizer.
comXL844www.
exelixis.
comFACurcuminGastrointestinalcancersPhaseIINewResearchDirectionsinDNARepair510TargetDrugConditionortumorCombinationtherapyagent(s)Phaseofclinicaltrialplanned,ongoingorrecentlycompleted*ReferencePathwayc-ABLImatinibVarioussolidtumoursPhaseIIIwww.
novartis.
comEGFRErlotinibNSCLCMonotherapyorcombinationPhaseII/IIIwww.
gene.
comGefinitibwww.
astrazeneca.
com*Asof10September2012,http://clinicaltrials.
govTable1.
Targetedtherapeuticsindevelopment,inclinicaluseorinclinicaltrials*.
ThisleadstothefinalandperhapsmostchallengingprobleminthedevelopmentofagentsthatmodulateDNArepair,whichistoxicitytonormalcells,inparticulartothehematopoieticsystemandthegastrointestinalepithelia.
Variousstrategiesarebeingfol‐lowedtominimizetoxicity,whichincludetheintermittentadministrationduringthera‐py,mentionedabove,alternatingwithothertherapies,usinghighlylocalizedradiotherapytogetherwithinhibitorstominimizecollateraldamage,andusinginhibitorsassingleagents[213,214].
Altogether,thecombineduseofthevariousweaponsatourdisposalinacoordinated,comprehensivefashioncouldeffectivelyleadtoimprovedpa‐tienttreatment.
AcknowledgementsThisworkwassupportedbygrantsPTDC/SAUGMG/71720/2006fromFundaodeCiênciaeTecnologia(FCT),andPEst-OE/SAU/UI0009/2011-12fromFCT.
M.
G.
wassupportedbyCIENCIA2008(FCT).
CIGMHissupportedbyFCT.
B.
G.
(SFRH/BD/64131/2009),P.
G.
(SFRH/BD/70293/2010)andC.
M.
(SFRH/BD/81097/2011)aresupportedbyPh.
D.
grantsfromFCT.
AuthordetailsAntónioS.
Rodrigues1*,BrunoCostaGomes1,CéliaMartins1,MartaGromicho1,NunoG.
Oliveira2,PatríciaS.
Guerreiro2andJoséRueff1*Addressallcorrespondenceto:sebastiao.
rodrigues@fcm.
unl.
pt1CIGMH–DepartmentofGenetics,FacultyofMedicalSciences,UniversidadeNovadeLis‐boa,Lisboa,Portugal2ResearchInstituteforMedicinesandPharmaceuticalSciences(iMed.
UL),UL,FacultyofPharmacy,UniversidadedeLisboa,Lisboa,PortugalDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952511References[1]FriedbergEC.
DNARepairAndMutagenesis:ASMPress;2006.
[2]HoeijmakersJ.
Genomemaintenancemechanismsforpreventingcancer.
Nature.
2001;411:366-74.
[3]HarperJW,ElledgeSJ.
TheDNADamageResponse:TenYearsAfter.
Molecularcell.
2007;28(5):739-45.
[4]LinZ,NeiM,MaH.
TheoriginsandearlyevolutionofDNAmismatchrepairgenes—multiplehorizontalgenetransfersandco-evolution.
NucleicAcidsResearch.
2007;35(22):7591-603.
[5]LehmannA,McGibbonD,StefaniniM.
Xerodermapigmentosum.
OrphanetJournalofRareDiseases.
2011;6(1):70.
[6]ParadisoA,FormentiS.
Hereditarybreastcancer:clinicalfeaturesandriskreductionstrategies.
AnnalsofOncology.
2011;22(suppl1):i31-i6.
[7]HoeijmakersJHJ.
DNADamage,Aging,andCancer.
NewEnglandJournalofMedi‐cine.
2009;361(15):1475-85.
[8]LengauerC,KinzlerKW,VogelsteinB.
Geneticinstabilitiesinhumancancers.
Na‐ture.
1998;396(6712):643-9.
[9]LoebLA.
AMutatorPhenotypeinCancer.
CancerResearch.
2001;61(8):3230-9.
[10]LagerwerfS,VrouweMG,OvermeerRM,FousteriMI,MullendersLHF.
DNAdam‐ageresponseandtranscription.
DNARepair.
2011;10(7):743-50.
[11]RodriguesAS,Dinis,J.
,Gromicho,M.
,Martins,M.
,Laires,A.
andRueff,J.
.
GenomicsandCancerDrugResistance.
CurrentPharmaceuticalBiotechnology.
2012;13(5):651-73.
[12]GilletJ-P,GottesmanMM.
MechanismsofMultidrugResistanceinCancerMulti-DrugResistanceinCancer.
In:ZhouJ,editor.
:HumanaPress;2010.
p.
47-76.
[13]O'ConnorMJ,MartinNMB,SmithGCM.
Targetedcancertherapiesbasedonthein‐hibitionofDNAstrandbreakrepair.
Oncogene.
2007;26(56):7816-24.
[14]Al-EjehF,KumarR,WiegmansA,LakhaniSR,BrownMP,KhannaKK.
HarnessingthecomplexityofDNA-damageresponsepathwaystoimprovecancertreatmentoutcomes.
Oncogene.
2010;29(46):6085-98.
[15]HurleyLH.
DNAanditsassociatedprocessesastargetsforcancertherapy.
NatRevCancer.
2002;2(3):188-200.
[16]KokkinakisDM,AhmedMM,DelgadoR,FruitwalaMM,MohiuddinM,Albores-SaavedraJ.
RoleofO6-Methylguanine-DNAMethyltransferaseintheResistanceofPancreaticTumorstoDNAAlkylatingAgents.
CancerResearch.
1997;57(23):5360-8.
NewResearchDirectionsinDNARepair512[17]SancarA,Lindsey-BoltzLA,nsal-KamazK,LinnS.
MolecularMechanismsofMammalianDNArepairandtheDNADamageCheckpoints.
AnnualReviewofBio‐chemistry.
2004;73(1):39-85.
[18]LiebermanHB.
DNADamageRepairandResponseProteinsasTargetsforCancerTherapy.
CurrentMedicinalChemistry.
2008;15(4):360-7.
[19]JacksonSP,BartekJ.
TheDNA-damageresponseinhumanbiologyanddisease.
Na‐ture.
2009;461(7267):1071-8.
[20]SchofieldM,HsiehP.
DNAmismatchrepair:molecularmechanismsandbiologicalfunction.
AnnuRevMicrobiol.
2003;57:579-608.
[21]PeltomkiP.
RoleofDNAMismatchRepairDefectsinthePathogenesisofHumanCancer.
JournalofClinicalOncology.
2003;21(6):1174-9.
[22]NguewaPA,FuertesMA,ValladaresB,AlonsoC,PérezJM.
Poly(ADP-Ribose)Poly‐merases:Homology,StructuralDomainsandFunctions.
NovelTherapeuticalAppli‐cations.
ProgressinBiophysicsandMolecularBiology.
2005;88(1):143-72.
[23]KassEM,JasinM.
CollaborationandcompetitionbetweenDNAdouble-strandbreakrepairpathways.
FEBSLetters.
2010;584(17):3703-8.
[24]LiSX,SjolundA,HarrisL,SweasyJB.
DNArepairandpersonalizedbreastcancertherapy.
EnvironmentalandMolecularMutagenesis.
2010;51(8-9):897-908.
[25]HelledayT.
Homologousrecombinationincancerdevelopment,treatmentandde‐velopmentofdrugresistance.
Carcinogenesis.
2010;31(6):955-60.
[26]BryantHE,SchultzN,ThomasHD,ParkerKM,FlowerD,LopezE,etal.
SpecifickillingofBRCA2-deficienttumourswithinhibitorsofpoly(ADP-ribose)polymerase.
Nature.
2005;434(7035):913-7.
[27]FarmerH,McCabeN,LordCJ,TuttANJ,JohnsonDA,RichardsonTB,etal.
Target‐ingtheDNArepairdefectinBRCAmutantcellsasatherapeuticstrategy.
Nature.
2005;434(7035):917-21.
[28]ChiarugiA.
AsnapshotofchemoresistancetoPARPinhibitors.
TrendsinPharmaco‐logicalSciences.
2012;33(1):42-8.
[29]DavarD,BeumerJH,HamiehL,TawbiH.
RoleofPARPInhibitorsinCancerBiologyandTherapy.
CurrMedChem.
2012;19(23):3907-21.
Epub2012/07/14.
[30]FongPC,BossDS,YapTA,TuttA,WuP,Mergui-RoelvinkM,etal.
InhibitionofPoly(ADP-Ribose)PolymeraseinTumorsfromBRCAMutationCarriers.
NewEng‐landJournalofMedicine.
2009;361(2):123-34.
[31]KelleyMR,FishelML.
DNArepairproteinsasmoleculartargetsforcancertherapeu‐tics.
Anti-CancerAgentsinMedicinalChemistry.
2008;8(4):417-25.
[32]EversB,HelledayT,JonkersJ.
Targetinghomologousrecombinationrepairdefectsincancer.
TrendsinPharmacologicalSciences.
2010;31(8):372-80.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952513[33]HelledayT,PetermannE,LundinC,HodgsonB,SharmaRA.
DNArepairpathwaysastargetsforcancertherapy.
NatureReviewsCancer.
2008;8(3):193-204.
[34]BouwmanP,JonkersJ.
TheeffectsofderegulatedDNAdamagesignallingoncancerchemotherapyresponseandresistance.
NatRevCancer.
2012;12(9):587-98.
[35]LongleyDB,JohnstonPG.
Molecularmechanismsofdrugresistance.
TheJournalofPathology.
2005;205(2):275-92.
[36]StrattonMR,CampbellPJ,FutrealPA.
Thecancergenome.
Nature.
2009;458(7239):719-24.
[37]DrablsF,FeyziE,AasPA,VaagbCB,KavliB,BratlieMS,etal.
AlkylationdamageinDNAandRNA—repairmechanismsandmedicalsignificance.
DNARepair.
2004;3(11):1389-407.
[38]KainaB,ChristmannM,NaumannS,RoosWP.
MGMT:Keynodeinthebattleagainstgenotoxicity,carcinogenicityandapoptosisinducedbyalkylatingagents.
DNARepair.
2007;6(8):1079-99.
[39]JacintoFV,EstellerM.
MGMThypermethylation:Aprognosticfoe,apredictivefriend.
DNARepair.
2007;6(8):1155-60.
[40]MargisonGP,SantibáezKorefMF,PoveyAC.
Mechanismsofcarcinogenicity/chemotherapybyO6-methylguanine.
Mutagenesis.
2002;17(6):483-7.
[41]ZaidiNH,LiuL,GersonSL.
QuantitativeimmunohistochemicalestimatesofO6-al‐kylguanine-DNAalkyltransferaseexpressioninnormalandmalignanthumancolon.
ClinicalCancerResearch.
1996;2(3):577-84.
[42]LeeSM,RaffertyJA,ElderRH,FanCY,BromleyM,HarrisM,etal.
Immunohistolog‐icalexaminationoftheinter-andintracellulardistributionofO6-alkylguanineDNA-alkyltransferaseinhumanliverandmelanoma.
BrJCancer.
1992;66(2):355-60.
[43]AugustineCK,YooJS,PottiA,YoshimotoY,ZipfelPA,FriedmanHS,etal.
GenomicandMolecularProfilingPredictsResponsetoTemozolomideinMelanoma.
ClinicalCancerResearch.
2009;15(2):502-10.
[44]HegiME,LiuL,HermanJG,StuppR,WickW,WellerM,etal.
CorrelationofO6-MethylguanineMethyltransferase(MGMT)PromoterMethylationWithClinicalOut‐comesinGlioblastomaandClinicalStrategiestoModulateMGMTActivity.
JournalofClinicalOncology.
2008;26(25):4189-99.
[45]HegiME,DiserensA-C,GorliaT,HamouM-F,deTriboletN,WellerM,etal.
MGMTGeneSilencingandBenefitfromTemozolomideinGlioblastoma.
NewEnglandJour‐nalofMedicine.
2005;352(10):997-1003.
[46]HegiME,DiserensA-C,GodardS,DietrichP-Y,RegliL,OstermannS,etal.
ClinicalTrialSubstantiatesthePredictiveValueofO-6-Methylguanine-DNAMethyltransfer‐asePromoterMethylationinGlioblastomaPatientsTreatedwithTemozolomide.
ClinicalCancerResearch.
2004;10(6):1871-4.
NewResearchDirectionsinDNARepair514[47]HegiME,SciuscioD,MuratA,LevivierM,StuppR.
EpigeneticDeregulationofDNARepairandItsPotentialforTherapy.
ClinicalCancerResearch.
2009;15(16):5026-31.
[48]SuzukiT,NakadaM,YoshidaY,NambuE,FuruyamaN,KitaD,etal.
TheCorrela‐tionbetweenPromoterMethylationStatusandtheExpressionLevelofO6-Methyl‐guanine-DNAMethyltransferaseinRecurrentGlioma.
JapaneseJournalofClinicalOncology.
2011;41(2):190-6.
[49]EstellerM,HamiltonSR,BurgerPC,BaylinSB,HermanJG.
InactivationoftheDNArepairgeneO6-methylguanine-DNAmethyltransferasebypromoterhypermethyla‐tionisacommoneventinprimaryhumanneoplasia.
CancerRes.
1999;59(4):793-7.
Epub1999/02/24.
[50]NakadaM,FurutaT,HayashiY,MinamotoT,HamadaJ-i.
Thestrategyforenhanc‐ingtemozolomideagainstmalignantglioma.
FrontiersinOncology.
2012;2.
[51]QuinnJA,DesjardinsA,WeingartJ,BremH,DolanME,DelaneySM,etal.
PhaseITrialofTemozolomidePlusO6-BenzylguanineforPatientsWithRecurrentorPro‐gressiveMalignantGlioma.
JournalofClinicalOncology.
2005;23(28):7178-87.
[52]MakiY,MurakamiJ,AsaumiJ-i,TsujigiwaH,NagatsukaH,KokeguchiS,etal.
RoleofO6-methylguanine–DNAmethyltransferaseandeffectofO6-benzylguanineontheanti-tumoractivityofcis-diaminedichloroplatinum(II)inoralcancercelllines.
Oraloncology.
2005;41(10):984-93.
[53]BattsE,MaiselC,KaneD,LiuL,FuP,O'BrienT,etal.
O6-benzylguanineandBCNUinmultiplemyeloma:aphaseIItrial.
CancerChemotherapyandPharmacology.
2007;60(3):415-21.
[54]RansonM,HerseyP,ThompsonD,BeithJ,McArthurGA,HaydonA,etal.
Random‐izedTrialoftheCombinationofLomeguatribandTemozolomideComparedWithTemozolomideAloneinChemotherapyNaivePatientsWithMetastaticCutaneousMelanoma.
JournalofClinicalOncology.
2007;25(18):2540-5.
[55]KhanOA,RansonM,MichaelM,OlverI,LevittNC,MortimerP,etal.
AphaseIItrialoflomeguatribandtemozolomideinmetastaticcolorectalcancer.
BrJCancer.
2008;98(10):1614-8.
[56]TawbiHA,VillaruzL,TarhiniA,MoschosS,SuleckiM,ViveretteF,etal.
InhibitionofDNArepairwithMGMTpseudosubstrates:phaseIstudyoflomeguatribincom‐binationwithdacarbazineinpatientswithadvancedmelanomaandothersolidtu‐mours.
BrJCancer.
2011;105(6):773-7.
[57]RansonM,MiddletonMR,BridgewaterJ,LeeSM,DawsonM,JowleD,etal.
Lome‐guatrib,apotentinhibitorofO6-alkylguanine-DNA-alkyltransferase:phaseIsafety,pharmacodynamic,andpharmacokinetictrialandevaluationincombinationwithte‐mozolomideinpatientswithadvancedsolidtumors.
ClinCancerRes.
2006;12(5):1577-84.
Epub2006/03/15.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952515[58]CaporasoP,TurrizianiM,VendittiA,MarchesiF,BuccisanoF,TirindelliMC,etal.
Novelroleoftriazenesinhaematologicalmalignancies:PilotstudyofTemozolo‐mide,LomeguatribandIL-2inthechemo-immunotherapyofacuteleukaemia.
DNARepair.
2007;6(8):1179-86.
[59]SabharwalA,CorriePG,MidgleyRS,PalmerC,BradyJ,MortimerP,etal.
AphaseItrialoflomeguatribandirinotecaninmetastaticcolorectalcancer.
CancerChemotherPharmacol.
2010;66(5):829-35.
Epub2009/12/30.
[60]KainaB,MargisonGP,ChristmannM.
TargetingO(6)-methylguanine-DNAmethyl‐transferasewithspecificinhibitorsasastrategyincancertherapy.
CellMolLifeSci.
2010;67(21):3663-81.
Epub2010/08/19.
[61]KochD,HundsbergerT,BoorS,KainaB.
LocalintracerebraladministrationofO6-benzylguaninecombinedwithsystemicchemotherapywithtemozolomideofapa‐tientsufferingfromarecurrentglioblastoma.
JournalofNeuro-Oncology.
2007;82(1):85-9.
[62]JiricnyJ.
Themultifacetedmismatch-repairsystem.
NatRevMolCellBiol.
2006;7:335-46.
[63]LiG.
MechanismsandfunctionsofDNAmismatchrepair.
CellRes.
2008;18:85-98.
[64]AaltonenL,PeltomakiP,LeachF,SistonenP,PylkkanenL,MecklinJ,etal.
Cluestothepathogenesisoffamilialcolorectalcancer.
Science.
1993;260(5109):812-6.
[65]BolandCR,ThibodeauSN,HamiltonSR,SidranskyD,EshlemanJR,BurtRW,etal.
ANationalCancerInstituteWorkshoponMicrosatelliteInstabilityforCancerDetec‐tionandFamilialPredisposition:DevelopmentofInternationalCriteriafortheDeter‐minationofMicrosatelliteInstabilityinColorectalCancer.
CancerResearch.
1998;58(22):5248-57.
[66]AebiS,Kurdi-HaidarB,GordonR,CenniB,ZhengH,FinkD,etal.
LossofDNAMismatchRepairinAcquiredResistancetoCisplatin.
CancerResearch.
1996;56(13):3087-90.
[67]HawnMT,UmarA,CarethersJM,MarraG,KunkelTA,BolandCR,etal.
EvidenceforaConnectionbetweentheMismatchRepairSystemandtheG2CellCycleCheck‐point.
CancerResearch.
1995;55(17):3721-5.
[68]LageH,DietelM.
InvolvementoftheDNAmismatchrepairsysteminantineoplasticdrugresistance.
Journalofcancerresearchandclinicaloncology.
1999;125(3):156-65.
[69]DioufB,ChengQ,KrynetskaiaNF,YangW,CheokM,PeiD,etal.
SomaticdeletionsofgenesregulatingMSH2proteinstabilitycauseDNAmismatchrepairdeficiencyanddrugresistanceinhumanleukemiacells.
NatMed.
2011;17(10):1298-303.
[70]KaplanE,GunduzU.
ExpressionanalysisofTOP2A,MSH2andMLH1genesinMCF7cellsatdifferentlevelsofetoposideresistance.
BiomedPharmacother.
2012;66(1):29-35.
Epub2012/01/31.
NewResearchDirectionsinDNARepair516[71]PoveyAC,BadawiAF,CooperDP,HallCN,HarrisonKL,JacksonPE,etal.
DNAAlkylationandRepairintheLargeBowel:AnimalandHumanStudies.
TheJournalofNutrition.
2002;132(11):3518S-21S.
[72]MaxwellJA,JohnsonSP,McLendonRE,ListerDW,HorneKS,RasheedA,etal.
Mis‐matchRepairDeficiencyDoesNotMediateClinicalResistancetoTemozolomideinMalignantGlioma.
ClinicalCancerResearch.
2008;14(15):4859-68.
[73]ValeriN,GaspariniP,BraconiC,PaoneA,LovatF,FabbriM,etal.
MicroRNA-21inducesresistanceto5-fluorouracilbydown-regulatinghumanDNAMutShomolog2(hMSH2).
ProceedingsoftheNationalAcademyofSciences.
2010;107(49):21098-103.
[74]RobertsonA,KlunglandA,RognesT,LeirosI.
DNARepairinMammalianCells.
CellularandMolecularLifeSciences.
2009;66(6):981-93.
[75]WallaceSS,MurphyDL,SweasyJB.
Baseexcisionrepairandcancer.
CancerLetters.
2012(0).
[76]SrivastavaDK,HusainI,ArteagaCL,WilsonSH.
DNApolymeraseβexpressiondif‐ferencesinselectedhumantumorsandcelllines.
Carcinogenesis.
1999;20(6):1049-54.
[77]TangJ-b,SvilarD,TrivediRN,WangX-h,GoellnerEM,MooreB,etal.
N-methylpur‐ineDNAglycosylaseandDNApolymeraseβmodulateBERinhibitorpotentiationofgliomacellstotemozolomide.
Neuro-Oncology.
2011;13(5):471-86.
[78]DinisJ,SilvaV,GromichoM,MartinsC,LairesA,TavaresP,etal.
DNAdamagere‐sponseinimatinibresistantchronicmyeloidleukemiaK562cells.
LeukLymphoma.
2012;53(10):2004-14.
Epub2012/04/06.
[79]MooreDH,MichaelH,TrittR,ParsonsSH,KelleyMR.
AlterationsintheExpressionoftheDNARepair/RedoxEnzymeAPE/ref-1inEpithelialOvarianCancers.
ClinicalCancerResearch.
2000;6(2):602-9.
[80]KelleyMR,ChengL,FosterR,TrittR,JiangJ,BroshearsJ,etal.
ElevatedandAlteredExpressionoftheMultifunctionalDNABaseExcisionRepairandRedoxEnzymeApe1/ref-1inProstateCancer.
ClinicalCancerResearch.
2001;7(4):824-30.
[81]WangD,LuoM,KelleyMR.
Humanapurinicendonuclease1(APE1)expressionandprognosticsignificanceinosteosarcoma:enhancedsensitivityofosteosarcomatoDNAdamagingagentsusingsilencingRNAAPE1expressioninhibition.
MolCancerTher.
2004;3(6):679-86.
Epub2004/06/24.
[82]RobertsonKA,BullockHA,XuY,TrittR,ZimmermanE,UlbrightTM,etal.
AlteredExpressionofApe1/ref-1inGermCellTumorsandOverexpressioninNT2CellsConfersResistancetoBleomycinandRadiation.
CancerResearch.
2001;61(5):2220-5.
[83]BobolaMS,FinnLS,EllenbogenRG,GeyerJR,BergerMS,BragaJM,etal.
Apurinic/ApyrimidinicEndonucleaseActivityIsAssociatedwithResponsetoRadiationandDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952517ChemotherapyinMedulloblastomaandPrimitiveNeuroectodermalTumors.
Clini‐calCancerResearch.
2005;11(20):7405-14.
[84]SilberJR,BobolaMS,BlankA,SchoelerKD,HaroldsonPD,HuynhMB,etal.
TheApurinic/ApyrimidinicEndonucleaseActivityofApe1/Ref-1ContributestoHumanGliomaCellResistancetoAlkylatingAgentsandIsElevatedbyOxidativeStress.
ClinicalCancerResearch.
2002;8(9):3008-18.
[85]BapatA,FishelML,KelleyMR.
Goingapeasanapproachtocancertherapeutics.
Antioxidants&redoxsignaling.
2009;11(3):651-68.
Epub2008/08/22.
[86]BapatA,GlassLS,LuoM,FishelML,LongEC,GeorgiadisMM,etal.
Novelsmall-moleculeinhibitorofapurinic/apyrimidinicendonuclease1blocksproliferationandreducesviabilityofglioblastomacells.
JPharmacolExpTher.
2010;334(3):988-98.
Epub2010/05/28.
[87]TavernaP,LiuL,HwangHS,HansonAJ,KinsellaTJ,GersonSL.
Methoxyaminepo‐tentiatesDNAsinglestrandbreaksanddoublestrandbreaksinducedbytemozolo‐mideincoloncancercells.
MutatRes.
2001;485(4):269-81.
Epub2001/10/05.
[88]RinneM,CaldwellD,KelleyMR.
TransientadenoviralN-methylpurineDNAglyco‐sylaseoverexpressionimpartschemotherapeuticsensitivitytohumanbreastcancercells.
MolCancerTher.
2004;3(8):955-67.
Epub2004/08/10.
[89]YanL,BulgarA,MiaoY,MahajanV,DonzeJR,GersonSL,etal.
Combinedtreat‐mentwithtemozolomideandmethoxyamine:blockingapurininc/pyrimidinicsitere‐paircoupledwithtargetingtopoisomeraseIIalpha.
ClinCancerRes.
2007;13(5):1532-9.
Epub2007/03/03.
[90]FishelML,HeY,SmithML,KelleyMR.
Manipulationofbaseexcisionrepairtosen‐sitizeovariancancercellstoalkylatingagenttemozolomide.
ClinCancerRes.
2007;13(1):260-7.
Epub2007/01/04.
[91]LiuL,YanL,DonzeJR,GersonSL.
Blockageofabasicsiterepairenhancesantitumorefficacyof1,3-bis-(2-chloroethyl)-1-nitrosoureaincolontumorxenografts.
MolCan‐cerTher.
2003;2(10):1061-6.
Epub2003/10/28.
[92]BulgarAD,WeeksLD,MiaoY,YangS,XuY,GuoC,etal.
Removalofuracilbyura‐cilDNAglycosylaselimitspemetrexedcytotoxicity:overridingthelimitwithme‐thoxyaminetoinhibitbaseexcisionrepair.
CellDeathDis.
2012;3:e252.
Epub2012/01/13.
[93]TavernaP,HwangHS,SchuppJE,RadivoyevitchT,SessionNN,ReddyG,etal.
In‐hibitionofbaseexcisionrepairpotentiatesiododeoxyuridine-inducedcytotoxicityandradiosensitization.
CancerResearch.
2003;63(4):838-46.
[94]YanT,SeoY,SchuppJE,ZengXH,DesaiAB,KinsellaTJ.
Methoxyaminepotentiatesiododeoxyuridine-inducedradiosensitizationbyalteringcellcyclekineticsanden‐hancingsenescence.
MolecularCancerTherapeutics.
2006;5(4):893-902.
NewResearchDirectionsinDNARepair518[95]WeissG,GordonM,RosenL,SavvidesP,AdamsB,AlvarezD,etal.
FinalresultsfromaphaseIstudyoforalTRC102(methoxyamineHCl),aninhibitorofbase-exci‐sionrepair,topotentiatetheactivityofpemetrexedinpatientswithrefractorycan‐cer.
[abstract].
JClinOncol.
2010;28(15s):abstract2576.
[96]SawidesP,XuY,LiuL,BokarJ,SilvermanP,DowlatiA,etal.
Pharmacokineticpro‐fileofthebase-excisionrepairinhibitormethoxyamine-HCl(TRC102;MX)givenasanone-hourintravenousinfusionwithtemozolomide(TMZ)inthefirst-in-humanphaseIclinicaltrial.
[abstract].
JClinOncol2010;28(15s):abstracte13662.
[97]MohammedMZ,VyjayantiVN,LaughtonCA,DekkerLV,FischerPM,WilsonDM,3rd,etal.
DevelopmentandevaluationofhumanAPendonucleaseinhibitorsinmel‐anomaandgliomacelllines.
BrJCancer.
2011;104(4):653-63.
Epub2011/01/27.
[98]ZawahirZ,DayamR,DengJ,PereiraC,NeamatiN.
Pharmacophoreguideddiscov‐eryofsmall-moleculehumanapurinic/apyrimidinicendonuclease1inhibitors.
JMedChem.
2009;52(1):20-32.
Epub2008/12/17.
[99]SimeonovA,KulkarniA,DorjsurenD,JadhavA,ShenM,McNeillDR,etal.
Identifi‐cationandcharacterizationofinhibitorsofhumanapurinic/apyrimidinicendonu‐cleaseAPE1.
PLoSOne.
2009;4(6):e5740.
Epub2009/06/02.
[100]SeipleLA,CardellinaJH,2nd,AkeeR,StiversJT.
Potentinhibitionofhumanapurin‐ic/apyrimidinicendonuclease1byarylstibonicacids.
MolPharmacol.
2008;73(3):669-77.
Epub2007/11/29.
[101]RaiG,VyjayantiVN,DorjsurenD,SimeonovA,JadhavA,WilsonDM,etal.
Synthe‐sis,BiologicalEvaluation,andStructure-ActivityRelationshipsofaNovelClassofApurinic/ApyrimidinicEndonuclease1Inhibitors.
JournalofMedicinalChemistry.
2012;55(7):3101-12.
[102]SrinivasanA,WangL,ClineC,XieZ,SobolRW,XieX,etal.
IdentificationandChar‐acterizationofHumanApurinic/ApyrimidinicEndonuclease-1Inhibitors.
Biochemis‐try.
2012;[Epubaheadofprint].
[103]LuoM,KelleyMR.
Inhibitionofthehumanapurinic/apyrimidinicendonuclease(APE1)repairactivityandsensitizationofbreastcancercellstoDNAalkylatingagentswithlucanthone.
AnticancerRes.
2004;24(4):2127-34.
Epub2004/08/28.
[104]NaiduMD,AgarwalR,PenaLA,CunhaL,MezeiM,ShenM,etal.
Lucanthoneanditsderivativehycanthoneinhibitapurinicendonuclease-1(APE1)bydirectproteinbinding.
PLoSOne.
2011;6(9):e23679.
Epub2011/09/22.
[105]MadhusudanS,SmartF,ShrimptonP,ParsonsJL,GardinerL,HoulbrookS,etal.
IsolationofasmallmoleculeinhibitorofDNAbaseexcisionrepair.
NucleicAcidsRes.
2005;33(15):4711-24.
Epub2005/08/23.
[106]HortonJK,Joyce-GrayDF,PachkowskiBF,SwenbergJA,WilsonSH.
Hypersensitivi‐tyofDNApolymerasebetanullmousefibroblastsreflectsaccumulationofcytotoxicDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952519repairintermediatesfromsite-specificalkylDNAlesions.
DNARepair.
2003;2(1):27-48.
[107]HuHY,HortonJK,GrykMR,PrasadR,NaronJM,SunDA,etal.
IdentificationofsmallmoleculesyntheticinhibitorsofDNApolymerasebetabyNMRchemicalshiftmapping.
JBiolChem.
2004;279(38):39736-44.
Epub2004/07/20.
[108]BarakatK,GajewskiM,TuszynskiJA.
DNARepairInhibitors:TheNextMajorSteptoImproveCancerTherapy.
CurrTopMedChem.
2012;12(12):1376-90.
[109]JavleM,CurtinNJ.
TheroleofPARPinDNArepairanditstherapeuticexploitation.
BritJCancer.
2011;105(8):1114-22.
[110]PlummerR,JonesC,MiddletonM,WilsonR,EvansJ,OlsenA,etal.
PhaseIStudyofthePoly(ADP-Ribose)PolymeraseInhibitor,AG014699,inCombinationwithTemo‐zolomideinPatientswithAdvancedSolidTumors.
ClinCancerRes.
2008;14(23):7917-23.
[111]UnderhillC,ToulmondeM,BonnefoiH.
AreviewofPARPinhibitors:frombenchtobedside.
AnnalsofOncology.
2011;22(2):268-79.
[112]AshworthA.
ASyntheticLethalTherapeuticApproach:Poly(ADP)RibosePolymer‐aseInhibitorsfortheTreatmentofCancersDeficientinDNADouble-StrandBreakRepair.
JournalofClinicalOncology.
2008;26(22):3785-90.
[113]deBonoJS,AshworthA.
Translatingcancerresearchintotargetedtherapeutics.
Na‐ture.
2010;467(7315):543-9.
[114]RouleauM,PatelA,HendzelMJ,KaufmannSH,PoirierGG.
PARPinhibition:PARP1andbeyond.
NatRevCancer.
2010;10(4):293-301.
[115]CalvertH,AzzaritiA.
Theclinicaldevelopmentofinhibitorsofpoly(ADP-ribose)polymerase.
AnnalsofOncology.
2011;22(suppl1):i53-i9.
[116]YapTA,SandhuSK,CardenCP,deBonoJS.
Poly(ADP-Ribose)polymerase(PARP)inhibitors:Exploitingasyntheticlethalstrategyintheclinic.
CA:ACancerJournalforClinicians.
2011;61(1):31-49.
[117]KummarS,ChenA,ParchmentR,KindersR,JiJ,TomaszewskiJ,etal.
AdvancesinusingPARPinhibitorstotreatcancer.
BMCmedicine.
2012;10(1):25.
[118]BryantHE,HelledayT.
Inhibitionofpoly(ADP-ribose)polymeraseactivatesATMwhichisrequiredforsubsequenthomologousrecombinationrepair.
NucleicAcidsRes.
2006;34(6):1685-91.
Epub2006/03/25.
[119]Mendes-PereiraAM,MartinSA,BroughR,McCarthyA,TaylorJR,KimJS,etal.
SyntheticlethaltargetingofPTENmutantcellswithPARPinhibitors.
EMBOMolMed.
2009;1(6-7):315-22.
Epub2010/01/06.
NewResearchDirectionsinDNARepair520[120]LeungM,RosenD,FieldsS,CesanoA,BudmanDR.
Poly(ADP-ribose)polymerase-1inhibition:preclinicalandclinicaldevelopmentofsyntheticlethality.
MolMed.
2011;17(7-8):854-62.
Epub2011/03/23.
[121]TuttA,RobsonM,GarberJE,DomchekSM,AudehMW,WeitzelJN,etal.
Oralpoly(ADP-ribose)polymeraseinhibitorolaparibinpatientswithBRCA1orBRCA2mutationsandadvancedbreastcancer:aproof-of-concepttrial.
Lancet.
2010;376(9737):235-44.
Epub2010/07/09.
[122]SultanaR,McNeillDR,AbbottsR,MohammedMZ,ZdzienickaMZ,QutobH,etal.
SyntheticlethaltargetingofDNAdouble-strandbreakrepairdeficientcellsbyhu‐manapurinic/apyrimidinicendonucleaseinhibitors.
IntJCancer.
2012.
Epub2012/03/02.
[123]GuhaM.
PARPinhibitorsstumbleinbreastcancer.
NatBiotechnol.
2011;29(5):373-4.
[124]DentR,LindemanG,ClemonsM,WildiersH,ChanA,McCarthyN,etal.
SafetyandefficacyoftheoralPARPinhibitorolaparib(AZD2281)incombinationwithpaclitax‐elforthefirst-orsecond-linetreatmentofpatientswithmetastatictriple-negativebreastcancer:ResultsfromthesafetycohortofaphaseI/IImulticentertrial[ab‐stract].
JClinOncol2010;28(15s):abstr1018.
[125]GelmonKA,TischkowitzM,MackayH,SwenertonK,RobidouxA,TonkinK,etal.
Olaparibinpatientswithrecurrenthigh-gradeserousorpoorlydifferentiatedovari‐ancarcinomaortriple-negativebreastcancer:aphase2,multicentre,open-label,non-randomisedstudy.
TheLancetOncology.
2011;12(9):852-61.
[126]WoodRD,MitchellM,LindahlT.
HumanDNArepairgenes,2005.
MutationRe‐search/FundamentalandMolecularMechanismsofMutagenesis.
2005;577(1–2):275-83.
[127]RabikCA,DolanME.
Molecularmechanismsofresistanceandtoxicityassociatedwithplatinatingagents.
CancerTreatmentReviews.
2007;33(1):9-23.
[128]KellandL.
Theresurgenceofplatinum-basedcancerchemotherapy.
NatRevCancer.
2007;7(8):573-84.
[129]KberleB,GrimaldiKA,SuntersA,HartleyJA,KellandLR,MastersJRW.
DNARe‐paircapacityandcisplatinsensitivityofhumantestistumourcells.
InternationalJournalofCancer.
1997;70(5):551-5.
[130]MastersJRW,KoberleB.
Curingmetastaticcancer:lessonsfromtesticulargerm-celltumours.
NatRevCancer.
2003;3(7):517-25.
[131]DabholkarM,Bostick-BrutonF,WeberC,BohrVA,EgwuaguC,ReedE.
ERCC1andERCC2ExpressioninMalignantTissuesFromOvarianCancerPatients.
JournaloftheNationalCancerInstitute.
1992;84(19):1512-7.
[132]ReedE.
ERCC1andClinicalResistancetoPlatinum-BasedTherapy.
ClinicalCancerResearch.
2005;11(17):6100-2.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952521[133]ShirotaY,StoehlmacherJ,BrabenderJ,XiongY-P,UetakeH,DanenbergKD,etal.
ERCC1andThymidylateSynthasemRNALevelsPredictSurvivalforColorectalCancerPatientsReceivingCombinationOxaliplatinandFluorouracilChemotherapy.
JournalofClinicalOncology.
2001;19(23):4298-304.
[134]OlaussenKA,DunantA,FouretP,BrambillaE,AndréF,HaddadV,etal.
DNARe‐pairbyERCC1inNon–Small-CellLungCancerandCisplatin-BasedAdjuvantChe‐motherapy.
NewEnglandJournalofMedicine.
2006;355(10):983-91.
[135]LordRVN,BrabenderJ,GandaraD,AlberolaV,CampsC,DomineM,etal.
LowERCC1ExpressionCorrelateswithProlongedSurvivalafterCisplatinplusGemcita‐bineChemotherapyinNon-SmallCellLungCancer.
ClinicalCancerResearch.
2002;8(7):2286-91.
[136]WeberpalsJ,GarbuioK,O'BrienA,Clark-KnowlesK,DoucetteS,AntonioukO,etal.
TheDNArepairproteinsBRCA1andERCC1aspredictivemarkersinsporadicovar‐iancancer.
InternationalJournalofCancer.
2009;124(4):806-15.
[137]JiangJ,LiangX,ZhouX,HuangR,ChuZ,ZhanQ.
ERCC1expressionasaprognos‐ticandpredictivefactorinpatientswithnon-smallcelllungcancer:ameta-analysis.
MolecularBiologyReports.
2012;39(6):6933-42.
[138]LiJ,ZhangJ,LiuY,YeG.
IncreasedexpressionofDNArepairgeneXPFenhancesresistancetohydroxycamptothecininbladdercancer.
Medicalsciencemonitor:in‐ternationalmedicaljournalofexperimentalandclinicalresearch.
2012;18(4):BR156-62.
Epub2012/03/31.
[139]PrewettM,DeeviDS,BassiR,FanF,EllisLM,HicklinDJ,etal.
TumorsEstablishedwithCellLinesSelectedforOxaliplatinResistanceRespondtoOxaliplatinifCom‐binedwithCetuximab.
ClinicalCancerResearch.
2007;13(24):7432-40.
[140]Balin-GauthierD,DelordJP,PillaireMJ,RochaixP,HoffmanJS,BugatR,etal.
Ce‐tuximabpotentiatesoxaliplatincytotoxiceffectthroughadefectinNERandDNAreplicationinitiation.
BrJCancer.
2008;98(1):120-8.
[141]RogakouEP,PilchDR,OrrAH,IvanovaVS,BonnerWM.
DNADouble-strandedBreaksInduceHistoneH2AXPhosphorylationonSerine139.
JournalofBiologicalChemistry.
1998;273(10):5858-68.
[142]PaullTT,RogakouEP,YamazakiV,KirchgessnerCU,GellertM,BonnerWM.
Acrit‐icalroleforhistoneH2AXinrecruitmentofrepairfactorstonuclearfociafterDNAdamage.
Currentbiology:CB.
2000;10(15):886-95.
[143]EstellerM,SilvaJM,DominguezG,BonillaF,Matias-GuiuX,LermaE,etal.
Promot‐erHypermethylationandBRCA1InactivationinSporadicBreastandOvarianTu‐mors.
JournaloftheNationalCancerInstitute.
2000;92(7):564-9.
[144]GraeserM,McCarthyA,LordCJ,SavageK,HillsM,SalterJ,etal.
AMarkerofHo‐mologousRecombinationPredictsPathologicCompleteResponsetoNeoadjuvantNewResearchDirectionsinDNARepair522ChemotherapyinPrimaryBreastCancer.
ClinicalCancerResearch.
2010;16(24):6159-68.
[145]WangW.
EmergenceofaDNA-damageresponsenetworkconsistingofFanconianaemiaandBRCAproteins.
NatRevGenet.
2007;8(10):735-48.
[146]TaronM,RosellR,FelipE,MendezP,SouglakosJ,RoncoMS,etal.
BRCA1mRNAexpressionlevelsasanindicatorofchemoresistanceinlungcancer.
HumanMolecu‐larGenetics.
2004;13(20):2443-9.
[147]QuinnJE,CarserJE,JamesCR,KennedyRD,HarkinDP.
BRCA1andimplicationsforresponsetochemotherapyinovariancancer.
GynecologicOncology.
2009;113(1):134-42.
[148]QuinnJE,KennedyRD,MullanPB,GilmorePM,CartyM,JohnstonPG,etal.
BRCA1FunctionsasaDifferentialModulatorofChemotherapy-inducedApoptosis.
CancerResearch.
2003;63(19):6221-8.
[149]HusainA,HeG,VenkatramanES,SpriggsDR.
BRCA1Up-RegulationIsAssociatedwithRepair-mediatedResistancetocis-Diamminedichloroplatinum(II).
CancerRe‐search.
1998;58(6):1120-3.
[150]KennedyRD,QuinnJE,MullanPB,JohnstonPG,HarkinDP.
TheRoleofBRCA1intheCellularResponsetoChemotherapy.
JournaloftheNationalCancerInstitute.
2004;96(22):1659-68.
[151]MargeliM,CirauquiB,CastellaE,TapiaG,CostaC,Gimenez-CapitanA,etal.
ThePrognosticValueofBRCA1mRNAExpressionLevelsFollowingNeoadjuvantChe‐motherapyinBreastCancer.
PLoSONE.
2010;5(3):e9499.
[152]HennessyBTJ,TimmsKM,CareyMS,GutinA,MeyerLA,FlakeDD,etal.
SomaticMutationsinBRCA1andBRCA2CouldExpandtheNumberofPatientsThatBenefitFromPoly(ADPRibose)PolymeraseInhibitorsinOvarianCancer.
JournalofClini‐calOncology.
2010;28(22):3570-6.
[153]WestonVJ,OldreiveCE,SkowronskaA,OscierDG,PrattG,DyerMJS,etal.
ThePARPinhibitorolaparibinducessignificantkillingofATM-deficientlymphoidtu‐morcellsinvitroandinvivo.
Blood.
2010;116(22):4578-87.
[154]OffitK,LevranO,MullaneyB,MahK,NafaK,BatishSD,etal.
SharedGeneticSus‐ceptibilitytoBreastCancer,BrainTumors,andFanconiAnemia.
JournaloftheNa‐tionalCancerInstitute.
2003;95(20):1548-51.
[155]PanasciL,PaiementJ-P,ChristodoulopoulosG,BelenkovA,MalapetsaA,AloyzR.
ChlorambucilDrugResistanceinChronicLymphocyticLeukemia.
ClinicalCancerResearch.
2001;7(3):454-61.
[156]KleinHL.
TheconsequencesofRad51overexpressionfornormalandtumorcells.
DNARepair.
2008;7(5):686-93.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952523[157]TobinLA,RobertC,RapoportAP,GojoI,BaerMR,TomkinsonAE,etal.
TargetingabnormalDNAdouble-strandbreakrepairintyrosinekinaseinhibitor-resistantchronicmyeloidleukemias.
Oncogene.
2012.
Epub2012/05/30.
[158]TobinLA,RobertC,NagariaP,ChumsriS,TwaddellW,IoffeOB,etal.
TargetingabnormalDNArepairintherapy-resistantbreastcancers.
Molecularcancerresearch:MCR.
2012;10(1):96-107.
Epub2011/11/25.
[159]HicksonI,ZhaoY,RichardsonCJ,GreenSJ,MartinNMB,OrrAI,etal.
IdentificationandCharacterizationofaNovelandSpecificInhibitoroftheAtaxia-TelangiectasiaMutatedKinaseATM.
CancerResearch.
2004;64(24):9152-9.
[160]CowellIG,DurkaczBW,TilbyMJ.
SensitizationofbreastcarcinomacellstoionizingradiationbysmallmoleculeinhibitorsofDNA-dependentproteinkinaseandataxiatelangiectsiamutated.
BiochemicalPharmacology.
2005;71(1–2):13-20.
[161]GoldingSE,RosenbergE,ValerieN,HussainiI,FrigerioM,CockcroftXF,etal.
Im‐provedATMkinaseinhibitorKU-60019radiosensitizesgliomacells,compromisesin‐sulin,AKTandERKprosurvivalsignaling,andinhibitsmigrationandinvasion.
MolecularCancerTherapeutics.
2009;8(10):2894-902.
[162]ShinoharaET,GengL,TanJ,ChenH,ShirY,EdwardsE,etal.
DNA-DependentPro‐teinKinaseIsaMolecularTargetfortheDevelopmentofNoncytotoxicRadiation–SensitizingDrugs.
CancerResearch.
2005;65(12):4987-92.
[163]LeahyJJJ,GoldingBT,GriffinRJ,HardcastleIR,RichardsonC,RigoreauL,etal.
IdentificationofahighlypotentandselectiveDNA-dependentproteinkinase(DNA-PK)inhibitor(NU7441)byscreeningofchromenonelibraries.
Bioorganic&Me‐dicinalChemistryLetters.
2004;14(24):6083-7.
[164]CollisSJ,DeWeeseTL,JeggoPA,ParkerAR.
ThelifeanddeathofDNA-PK.
Onco‐gene.
2004;24(6):949-61.
[165]HardcastleIR,CockcroftX,CurtinNJ,El-MurrMD,LeahyJJJ,StockleyM,etal.
Dis‐coveryofPotentChromen-4-oneInhibitorsoftheDNA-DependentProteinKinase(DNA-PK)UsingaSmall-MoleculeLibraryApproach.
JournalofMedicinalChemis‐try.
2005;48(24):7829-46.
[166]ZabludoffSD,DengC,GrondineMR,SheehyAM,AshwellS,CalebBL,etal.
AZD7762,anovelcheckpointkinaseinhibitor,drivescheckpointabrogationandpo‐tentiatesDNA-targetedtherapies.
MolecularCancerTherapeutics.
2008;7(9):2955-66.
[167]IorioMV,CroceCM.
MicroRNAdysregulationincancer:diagnostics,monitoringandtherapeutics.
Acomprehensivereview.
EMBOMolecularMedicine.
2012;4(3):143-59.
[168]BartelD.
MicroRNAs:genomics,biogenesis,mechanism,andfunction.
Cell.
2004;116(2):281-97.
NewResearchDirectionsinDNARepair524[169]BartelD.
MicroRNAs:targetrecognitionandregulatoryfunctions.
Cell.
2009;136:215-33.
[170]GarzonR,CalinGA,CroceCM.
MicroRNAsinCancer.
AnnualReviewofMedicine.
2009;60(1):167-79.
[171]DiLevaG,BriskinD,CroceCM.
MicroRNAincancer:Newhopesforantineoplasticchemotherapy.
UpsalaJournalofMedicalSciences.
2012;117(2):202-16.
[172]TianW,ChenJ,HeH,DengY.
MicroRNAsanddrugresistanceofbreastcancer:ba‐sicevidenceandclinicalapplications.
ClinicalandTranslationalOncology.
2012:1-8.
[173]KutanziKR,YurchenkoOV,BelandFA,CheckhunVF,PogribnyIP.
MicroRNA-mediateddrugresistanceinbreastcancer.
ClinEpigenetics.
2011;2(2):171-85.
Epub2011/09/29.
[174]HuH,GattiRA.
MicroRNAs:newplayersintheDNAdamageresponse.
JournalofMolecularCellBiology.
2010.
[175]WoutersMD,vanGentDC,HoeijmakersJHJ,PothofJ.
MicroRNAs,theDNAdam‐ageresponseandcancer.
MutationResearch/FundamentalandMolecularMecha‐nismsofMutagenesis.
2011;717(1–2):54-66.
[176]YuY,WangY,RenX,TsuyadaA,LiA,LiuLJ,etal.
Context-DependentBidirection‐alRegulationoftheMutSHomolog2byTransformingGrowthFactorβContributestoChemoresistanceinBreastCancerCells.
MolecularCancerResearch.
2010;8(12):1633-42.
[177]MoskwaP,BuffaFM,PanY,PanchakshariR,GottipatiP,MuschelRJ,etal.
miR-182-MediatedDownregulationofBRCA1ImpactsDNARepairandSensitivitytoPARPInhibitors.
Molecularcell.
2011;41(2):210-20.
[178]SadonesJ,MichotteA,VeldP,ChaskisC,SciotR,MentenJ,etal.
MGMTpromoterhypermethylationcorrelateswithasurvivalbenefitfromtemozolomideinpatientswithrecurrentanaplasticastrocytomabutnotglioblastoma.
EuropeanJournalofCancer.
2009;45(1):146-53.
[179]StuppR,HegiME,MasonWP,vandenBentMJ,TaphoornMJB,JanzerRC,etal.
Ef‐fectsofradiotherapywithconcomitantandadjuvanttemozolomideversusradio‐therapyaloneonsurvivalinglioblastomainarandomisedphaseIIIstudy:5-yearanalysisoftheEORTC-NCICtrial.
TheLancetOncology.
2009;10(5):459-66.
[180]SlabyO,LakomyR,FadrusP,HrstkaR,KrenL,LzicarovaE,etal.
MicroRNA-181familypredictsresponsetoconcomitantchemoradiotherapywithtemozolomideinglioblastomapatients.
Neoplasma.
2010;57(3):264-9.
Epub2010/04/01.
[181]ZhangW,ZhangJ,HoadleyK,KushwahaD,RamakrishnanV,LiS,etal.
miR-181d:apredictiveglioblastomabiomarkerthatdownregulatesMGMTexpression.
Neuro-Oncology.
2012;14(6):712-9.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952525[182]LakomyR,SanaJ,HankeovaS,FadrusP,KrenL,LzicarovaE,etal.
MiR-195,miR-196b,miR-181c,miR-21expressionlevelsandO-6-methylguanine-DNAmethyl‐transferasemethylationstatusareassociatedwithclinicaloutcomeinglioblastomapatients.
CancerScience.
2011;102(12):2186-90.
[183]SurhY-J.
Cancerchemopreventionwithdietaryphytochemicals.
NatRevCancer.
2003;3(10):768-80.
[184]KhanN,AfaqF,MukhtarH.
Apoptosisbydietaryfactors:thesuicidesolutionfordelayingcancergrowth.
Carcinogenesis.
2006;28(2):233-9.
[185]HanahanD,WeinbergRobertA.
HallmarksofCancer:TheNextGeneration.
Cell.
2011;144(5):646-74.
[186]AnandP,SundaramC,JhuraniS,KunnumakkaraAB,AggarwalBB.
Curcuminandcancer:An"old-age"diseasewithan"age-old"solution.
CancerLetters.
2008;267(1):133-64.
[187]RaffoulJJ,BanerjeeS,CheM,KnollZE,DoergeDR,AbramsJ,etal.
Soyisoflavonesenhanceradiotherapyinametastaticprostatecancermodel.
IntJCancer.
2007;120(11):2491-8.
Epub2007/02/17.
[188]RaffoulJJ,BanerjeeS,Singh-GuptaV,KnollZE,FiteA,ZhangH,etal.
Down-regula‐tionofApurinic/ApyrimidinicEndonuclease1/RedoxFactor-1ExpressionbySoyIsoflavonesEnhancesProstateCancerRadiotherapyInvitroandInvivo.
CancerRe‐search.
2007;67(5):2141-9.
[189]RaffoulJJ,HeydariAR,HillmanGG.
DNARepairandCancerTherapy:TargetingAPE1/Ref-1UsingDietaryAgents.
Journalofoncology.
2012;2012:11.
[190]RaffoulJJ,SarkarFH,HillmanGG.
Radiosensitizationofprostatecancerbysoyiso‐flavones.
CurrCancerDrugTargets.
2007;7(8):759-65.
Epub2008/01/29.
[191]YangS,IraniK,HeffronSE,JurnakF,MeyskensFL.
Alterationsintheexpressionoftheapurinic/apyrimidinicendonuclease-1/redoxfactor-1(APE/Ref-1)inhumanmel‐anomaandidentificationofthetherapeuticpotentialofresveratrolasanAPE/Ref-1inhibitor.
MolecularCancerTherapeutics.
2005;4(12):1923-35.
[192]FuldaS.
Resveratrolandderivativesforthepreventionandtreatmentofcancer.
DrugDiscoveryToday.
2010;15(17–18):757-65.
[193]FustierP,LeCorreL,ChalabiN,Vissac-SabatierC,CommunalY,BignonYJ,etal.
ResveratrolincreasesBRCA1andBRCA2mRNAexpressioninbreasttumourcelllines.
BrJCancer.
2003;89(1):168-72.
[194]PotterAJ,GollahonKA,PalancaBJA,HarbertMJ,ChoiYM,MoskovitzAH,etal.
FlowcytometricanalysisofthecellcyclephasespecificityofDNAdamageinducedbyradiation,hydrogenperoxideanddoxorubicin.
Carcinogenesis.
2002;23(3):389-401.
NewResearchDirectionsinDNARepair526[195]ShinSY,YongY,KimCG,LeeYH,LimY.
DeoxypodophyllotoxininducesG2/McellcyclearrestandapoptosisinHeLacells.
CancerLetters.
2010;287(2):231-9.
[196]ParkC,KimGY,KimGD,ChoiBT,ParkYM,ChoiYH.
InductionofG2/Marrestandinhibitionofcyclooxygenase-2activitybycurcumininhumanbladdercancerT24cells.
OncolRep.
2006;15(5):1225-31.
Epub2006/04/06.
[197]SaG,DasT.
Anticancereffectsofcurcumin:cycleoflifeanddeath.
CellDivision.
2008;3(1):14.
[198]LeCorreL,FustierP,ChalabiN,BignonY-J,Bernard-GallonD.
EffectsofresveratrolontheexpressionofapanelofgenesinteractingwiththeBRCA1oncosuppressorinhumanbreastcelllines.
ClinicaChimicaActa.
2004;344(1–2):115-21.
[199]PapoutsisAJ,LamoreSD,WondrakGT,SelminOI,RomagnoloDF.
ResveratrolPre‐ventsEpigeneticSilencingofBRCA-1bytheAromaticHydrocarbonReceptorinHu‐manBreastCancerCells.
TheJournalofNutrition.
2010;140(9):1607-14.
[200]MahapatraS,KarnesR,HolmesM,YoungC,ChevilleJ,KohliM,etal.
NovelMolec‐ularTargetsof<i>AzadirachtaindicaAssociatedwithInhibitionofTumorGrowthinProstateCancer.
TheAAPSJournal.
2011;13(3):365-77.
[201]KonkimallaVSB,WangG,KainaB,EfferthT.
Microarray-basedExpressionofDNARepairGenesDoesnotCorrelatewithGrowthInhibitionofCancerCellsbyNaturalProductsDerivedfromTraditionalChineseMedicine.
CancerGenomics-Proteo‐mics.
2008;5(2):79-83.
[202]NitureSK,VeluCS,SmithQR,BhatGJ,SrivenugopalKS.
IncreasedexpressionoftheMGMTrepairproteinmediatedbycysteineprodrugsandchemopreventativenatu‐ralproductsinhumanlymphocytesandtumorcelllines.
Carcinogenesis.
2006;28(2):378-89.
[203]AggarwalBB,ShishodiaS.
Moleculartargetsofdietaryagentsforpreventionandtherapyofcancer.
BiochemicalPharmacology.
2006;71(10):1397-421.
[204]TyagiAK,SinghRP,AgarwalC,ChanDCF,AgarwalR.
SilibininStronglySynergiz‐esHumanProstateCarcinomaDU145CellstoDoxorubicin-inducedGrowthInhibi‐tion,G2-MArrest,andApoptosis.
ClinicalCancerResearch.
2002;8(11):3512-9.
[205]MoenMD.
Ixabepilone:InLocallyAdvancedorMetastaticBreastCancer.
Drugs.
2009;69(11):1471-8110.
2165/00003495-200969110-00006.
[206]KanaiM,YoshimuraK,AsadaM,ImaizumiA,SuzukiC,MatsumotoS,etal.
AphaseI/IIstudyofgemcitabine-basedchemotherapypluscurcuminforpatientswithgemcitabine-resistantpancreaticcancer.
CancerChemotherapyandPharmacology.
2011;68(1):157-64.
[207]LiY,VandenBoomTG,KongD,WangZ,AliS,PhilipPA,etal.
Up-regulationofmiR-200andlet-7byNaturalAgentsLeadstotheReversalofEpithelial-to-Mesen‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952527chymalTransitioninGemcitabine-ResistantPancreaticCancerCells.
CancerRe‐search.
2009;69(16):6704-12.
[208]LiY,KongD,WangZ,SarkarF.
RegulationofmicroRNAsbyNaturalAgents:AnEmergingFieldinChemopreventionandChemotherapyResearch.
Pharmaceuticalresearch.
2010;27(6):1027-41.
[209]SarkarFH,LiY.
Harnessingthefruitsofnatureforthedevelopmentofmulti-target‐edcancertherapeutics.
CancerTreatmentReviews.
2009;35(7):597-607.
[210]SarkarFH,LiY,WangZ,KongD,AliS.
ImplicationofmicroRNAsindrugresist‐ancefordesigningnovelcancertherapy.
Drugresistanceupdates:reviewsandcom‐mentariesinantimicrobialandanticancerchemotherapy.
2010;13(3):57-66.
[211]AdamsRA,MeadeAM,SeymourMT,WilsonRH,MadiA,FisherD,etal.
Intermit‐tentversuscontinuousoxaliplatinandfluoropyrimidinecombinationchemotherapyforfirst-linetreatmentofadvancedcolorectalcancer:resultsoftherandomisedphase3MRCCOINtrial.
TheLancetOncology.
2011;12(7):642-53.
[212]BeckerA,CrombagL,HeidemanDAM,ThunnissenFB,vanWijkAW,PostmusPE,etal.
Retreatmentwitherlotinib:RegainofTKIsensitivityfollowingadrugholidayforpatientswithNSCLCwhoinitiallyrespondedtoEGFR-TKItreatment.
Europeanjournalofcancer(Oxford,England:1990).
2011;47(17):2603-6.
[213]KelleyMR.
Chapter14-FutureDirectionswithDNARepairInhibitors:ARoadmapforDisruptiveApproachestoCancerTherapy.
In:MarkRK,editor.
DNARepairinCancerTherapy.
SanDiego:AcademicPress;2012.
p.
301-10.
[214]KelleyMR.
DNArepairinhibitors:wheredowegofromhereDNARepair(Amst).
2011;10(11):1183-5.
Epub2011/10/04.
NewResearchDirectionsinDNARepair528
Rodrigues,BrunoCostaGomes,CéliaMartins,MartaGromicho,NunoG.
Oliveira,PatríciaS.
GuerreiroandJoséRueffAdditionalinformationisavailableattheendofthechapterhttp://dx.
doi.
org/10.
5772/539521.
IntroductionHumansareconstantlyexposedtodiversechemicalandphysicalagentsthathavethepotentialtodamageDNA,suchasreactiveoxygenspecies(ROS),ionizingradiation(IR),UVlight,andvariousenvironmental,dietaryorpollutantchemicalagents.
Theintegrityandsurvivalofacelliscriticallydependentongenomestability,andcellspossessmulti‐plepathwaystorepairtheseDNAlesions.
Thesepathwaysarediverseandtargetdiffer‐enttypesoflesions.
ThecriticalroleplayedbyDNArepairinthemaintenanceofgenomestabilityishighlightedbythefactthatmanyenzymesinvolvedhavebeenconservedthroughevolution[1-4].
VeryrarelygermlinemutationsoccurinseveraloftheDNArepairgenesandarethecauseofcancerpredisposingsyndromes,suchasXerodermapigmentosum(XP),[5],Fanconianemia(FA)andataxiatelangiectasia(AT)andareassociatedwithinherentchromosomeinstability[2].
Oneofthemostwell-knownexamplesofadefectinDNArepairleadingtocanceristheassociationofgerm-lineBRCA1/2mutationswithbreast,ovarianandperitonealmalignan‐cies[6].
TheserarehumanDNArepairsyndromeshavebeeninvaluableinprovidingmech‐anisticexplanationsfortheinvolvementofDNArepairsystemincancer.
Theyhavealsobeeninstrumentalinthetranslationofthesefindingstotheclinic.
Ontheotherhand,recentstudieshaveshownthatdefectiveDNAdamagerepairispresentinvirtuallyallsporadictumours[7].
MutationsinDNArepairgenescouldbeei‐therresponsiblefortheoccurrenceoftumoursorcouldariseduetorandomaccumula‐tionofmutationsduringcyclingofcancercells.
ThepresenceofincorrectDNArepairintumourcellspredisposesthemtoaccumulateevenmoregeneticalterations.
Forexample,colorectalandendometrialcancerswithdefectiveDNAmismatchrepair(MMR)dueto2013Rodriguesetal.
;licenseeInTech.
ThisisanopenaccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/3.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
mutationsintheMLH1andMSH2genesexhibitincreasedratesofacquisitionofsinglenucleotidechangesandsmallinsertions/deletions[8].
Thus,thepresenceofa"mutatorphenotype"[9]couldincreasetheevolutionaryacquisitionofalterationsthatultimatelycouldleadtoenhanceddrugresistance.
AfurtherreminderontheimportanceofDNArepairistheobservationthatmutationsinspecificgenescanleadnottoanincreaseincancerbuttoacceleratedagingsyndromes[7].
AnexampleofthisisCockayne'ssyndrome(CS),whichcausessevereprogeroidsyndromes[10].
Mutationsinthegenesthatencodetwoproteinsinanucleotideexcisionrepair(NER)sub-pathwaycalledtranscriptioncoupledrepair(TCR)causeglobalprematurecelldeaththroughapoptosis.
InthiscaseapoptosisensuresthatDNAmutationsarenottransmittedtodaughtercells,albeitattheexpenseofcellviability,andhighlightstheimportanceofmain‐tainingDNAintegrity.
Onemajorproblemincancertherapyisthefactthatofthe7.
6millioncancerdeathsthatoc‐cureveryyearworldwide(2008data;http://www.
who.
int/cancer/en/),manyareduetofail‐ureofcancertherapyassociatedwithacquiredandintrinsicresistancemechanisms.
Thesemechanismsofresistancecanbeclassifiedindifferentways,butthemostcharacterizedarealteredcellulardrugtransport,increasedsurvivalordecreasedcelldeath,alteredDNAre‐pair,andalterationsindrugtargets[11,12].
OverthelastyearstheimportanceofDNAre‐pairpathwaysinresistancetochemotherapyhasbeenincreasinglyrecognized,buttranslationtotheclinicisstillscarce.
SincemanyclassicalcancertherapiestargetDNA,theinfluenceofDNArepairsystemsinresponsetoDNAdamagewhichprimarilyresultfromchemotherapyandradiotherapyiscriticaltocellsurvival.
TheuseofinhibitorsofDNAre‐pairorDNAdamagesignallingpathwaysprovidesaninterestingopportunitytotargetthegeneticdifferencesthatexistbetweennormalandtumourtissue[13,14].
TherationaleunderlyingtheuseofDNAdamagingagentsintherapeuticstrategiesistokillcancercellswhilesparingnormaltissues,duetoincreasedcellcyclingofcancercells.
Un‐fortunatelyhighlycyclingnormalcells(e.
g.
bonemarrow,hairfolliclesandgastrointestinalepithelia)arealsotargetedbyDNAdamagingtherapeuticagents,givingrisetothesecon‐daryeffectsnormallyseenaftercancertherapy(e.
g.
diarrhoea,mouthulcers,hairloss,anae‐miaandsusceptibilitytoinfections).
Nevertheless,DNA-damagingchemotherapeuticagentsareeffectiveandprolongsurvivalofcancerpatients[15].
Chemotherapeuticagentscommonlyusedincancertreatmentproduceaplethoraoflesionsthatcanbetargetsforcel‐lularresponses.
Forexample,DNAdoublestrandbreaks(DSBs),single-strandbreaks(SSBs),andoxidizedbasesareinducedbyionizingradiation(IR),anthracyclines,platinumcompoundsandtaxanes.
AnthracyclinesaretopoisomeraseIIinhibitorsandDNAinterca‐latingagents,whichwhenusedcanleadtoDSBs.
Platinumcompoundsarebifunctionalal‐kylatingagentsthatinducepredominantlyintra-andinterstrandcrosslinks(ICLs)andtaxanesaremitoticinhibitors.
Alltheselesionsinducecellularresponsesthatcoveramulti‐tudeofpathways,includingDNArepairpathways,DNAtolerancemechanisms,coordina‐tionnetworksthatlinkrepairandcellcycleprogression,aswellasapoptoticandothercelldeathpathwayswhenDNAdamageisirreparable[16-19].
NewResearchDirectionsinDNARepair490TheDNArepairpathwaysthatrespondtotheselesionsinclude:directrepairofalkylad‐ductsbyO6-alkylguanineDNAalkyltransferase(MGMT);repairofbasedamageandSSBsbybaseexcisionrepair(BER);repairofbulkyDNAadductsbynucleotideexcisionrepair(NER);repairofcross-linksbyDNAinterstrandcross-linkrepairandrepairofmismatchesandinsertion/deletionloopsbyDNAmismatchrepair(MMR);repairofDSBsbyhomolo‐gousrecombination(HR)andnon-homologousendjoining(NHEJ).
DetaileddescriptionofthebiochemicalpathwaysofDNArepairisbeyondthescopeofthischapterasseveralre‐viewsonthesubjecthavebeenpublished[1,17,20-23].
TheobservationthatavarietyoftumoursfrequentlypresentderegulatedexpressionofDNArepairgenes(e.
g.
MGMT,PARP1)rapidlyleadtothenotionthatDNArepairpath‐wayscouldbetargetedincancertreatmentandleadtopersonalizedtherapy[24,25].
Tu‐mourswithspecificDNArepairdefectscouldbecompletelydependentonback-upDNArepairpathwaysfortheirsurvival.
Thisdependencecouldbeexploitedtherapeuticallytoin‐ducecelldeathandapoptosisintumourcells[26,27].
Thegeneticstateinwhichsimultane‐ousinactivationof2genes(orpathways)islethal,whilelossofoneortheotheraloneisviableiscalledsyntheticlethality(alsoknownasconditionalgenetics).
Therationaleforin‐ducingsyntheticlethalityincanceristhatcertaincancercellslackonepathwaytorepairtheirDNA(e.
g.
HR)buthavealternativepathways(baseexcisionorsingle-strandrepair)thatallowthemtosurvive.
InhibitionofthesealternativepathwayswouldthenimpairDNArepairandinducecelldeath[26,27].
Thereforeitpredictsthatgenotoxicagentslead‐ingtoaparticulartypeofDNAdamagewillkillcancercellswithgeneticdeficitsinrepairofthattypeofdamage.
Recently,thisspecificanticancerstrategyhasbeenthefocusofintenseinvestigations[28,29].
InthecaseofthehereditaryBRCA1/2-deficientbreastandovariancancersyndromes,men‐tionedearlier,thisstrategyhasbeentranslatedintotheclinic,intheformofPARPinhibi‐tors.
TheseBRCA1/2-tumoursaredefectiveintherepairofDSBsbyHR.
WhenareplicationforkinoneofthesetumoursencountersaDNASSB,itconvertsthatintoaDSB,butthepresenceofaDSBpreventsprogressionofthereplicationapparatus.
SinceBRCA1/2arebothrequiredforDSBrepair,thetumourcellswiththosemutatedgeneswilldependonrepairofSSBstopreventDSBsfromoccurring.
TheDNArepairproteinPARP1isrequiredforrepairofSSBs,andsmallmolecularinhibitorsofPARP1willpreventrepairofSSBs,morespecifi‐callyincellsthataredeficientinBRCA1/2.
SincenormalcellshavetheabilitytorepairtheDSBsgeneratedatthereplicationfork,becausetheyhaveatleastonenormalalleleofBRCA1/2,theuseofPARPinhibitorshasthepotentialoftargetingonlytumourcells.
Thisproofofconceptprovenclinically,wherethePARP1inhibitorolaparibimprovesthepro‐gression-freesurvivaloffamilialbreastcancer[30].
Followingthisleadseveralsmallmole‐culeDNArepairinhibitorsarebeingdevelopedworldwide.
However,notallBRCA1/2defectivetumoursrespondequallywelltothistypeoftherapy.
Thus,inthepastyearsevidencehasaccumulatedthatdrugresistanceisalsolinkedtoalter‐ationsinthesepathways[31-33].
Thus,tumourcellsmayalsoacquireresistancebyinvokingbiochemicalmechanismsthatreducedrugactionorbyacquiringadditionalalterationsinDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952491DNAdamageresponsepathways[34].
Therefore,thefocushasalsobeendirectedonDNArepairpathwaysthatcouldberesponsibleforcancerdrugresistance.
Resistancetochemotherapylimitstheeffectivenessofanti-cancerdrugtreatment.
Tumoursmaybeintrinsicallydrug-resistantordevelopresistancetochemotherapyduringtreatment.
Acquiredresistanceisaparticularproblem,astumoursnotonlybecomeresistanttothedrugsoriginallyusedtotreatthem,butmayalsobecomecross-resistanttootherdrugswithdifferentmechanismsofaction.
Resistancetochemotherapyisbelievedtocausetreatmentfailureinover90%ofpatientswithmetastaticcancer[35].
Thus,drugresistanceisclearlyamajorclinicalproblem.
Theattempttodevelopmoretargetedtherapeuticshasbeenamajorobjectiveincancerre‐searchinlastyears,andmoreandmoremoleculartargetsarebeingidentified(e.
g.
tyrosinekinaseinhibitors,monoclonalantibodiestargetingmembranereceptorkinases).
Someofthesetargetedtherapiesareinclinicaluse,whileothersarebeingevaluatedinclinicaltrialstovalidatetheirefficacy.
Morerecently,thequestfortargetedtherapieshasalsofocusedonDNArepairpathways.
Unfortunately,resistancetothesetherapiesisalsolikelytoappear,ashasoccurredwithothertargetedtherapies,suchasthetyrosinekinaseinhibitorsofthefusionBCR-ABL1gene,responsibleformostcasesofchronicmyeloidleukaemia(e.
g.
imati‐nib,dasatinib,nilotinib).
TheapplicationofDNArepairinhibitorsintheclinichasalsoshowntobefraughtwithdifficulty,sincetheyalsotargetDNArepairpathwaysinnormalcells.
TheearlyclinicaltrialwithMGMTinhibitorsincombinationwithtemozolomide(TMZ)wasstoppedearlybecausethecombinedtreatmentsharmedbonemarrowaswellascancertissue,whereastheclinicalsuccessofPARPinhibitorstranspiredsincePARPisnotcriticaltocellsurvival.
Hence,unlikepastvisionsofa"magicbullet"towardscancer,futureresearchoncancertherapyshouldmorereasonablyenvisagecancertherapyasa"neverendingstory",inwhichnoveltargetedtherapeuticsareconstantlybeingovercomebytheevolutionaryprocessespresentincancerouscells[36].
2.
TargetingDNArepairpathwaysAsmentioned,DNArepairpathwaysincludethedirectreversaloflesions,essentiallyde-alkylationofalkylatedbasesbyMGMT,NER,BER,MMRandthedoublestrandbreakre‐pairbyHRandNHEJ.
Alterationsinallthesepathwayshavebeenobservedindrugresistanttumourcells;however,theclinicalsignificanceofthealterationsisnotcompletelyunderstood.
Numerousgenesinvolvedineachofthesepathwayshavebeenshowntobeup-ordown-regulatedindiversetypesoftumoursandconstituteapotentialsourceofbio‐markerstoevaluatedrugresistancetocancerchemotherapeutics[25,32,33].
3.
MGMTanddrugresistanceAlkylatingagentsarewidelyusedtotreatcancers,andoneofthemajorDNAlesionsformedoccursessentiallybythealkylationofDNAattheO6-positionofguanine,whichNewResearchDirectionsinDNARepair492subsequentlycangenerateDNAbreaksandcelldeath.
TMZ,streptozotocin,procarbazineanddacarbazineareexamplesofcancerchemotherapeuticsthatmethylateDNA[37].
Directrepairofalkylatedguanineresiduesproceedsthroughtheremovalofthealkylmoi‐etybyMGMT.
MGMTisaconservedproteinfromprokaryotesthrougheukaryotes.
TheMGMTproteinremovesthealkylgroupfromO6-alkylguaninebydirecttransfertoacys‐teineresidueinitsactivesitetowhichthealkylgroupbecomescovalentlyattached,result‐ingintheinactivationoftheprotein.
TheMGMTproteinissubsequentlyubiquitinatedanddegradedbytheproteasome[38,39].
TheO6-alkylguanineadductaccountsforabout10%oftotalalkylations,butdisplaysastrongmutagenicandcytotoxicpotential,becauseO6-alkyl‐guaninesexhibitdistortedbasepairingcharacteristicsinpairingwiththymine,thereby,re‐sultinginG:CtoA:TtransitionsuponDNAreplication[40].
HencetheuniqueDNArepairmechanismwhichdependsonthesuicidaldegradationoftheMGMTprotein.
TumourexpressionofMGMTvariesandcorrelateswiththerapeuticresponsetoalkylatingagents.
NumerousstudieshavefoundastrongcorrelationbetweenMGMTactivityanddrugresistanceinprimarytumoursandestablishedhumantumourcelllines[16,41,42].
Highlevelsofexpressionhavealsobeennotedinmelanoma[43],pancreaticcarcinoma[16]besidesglioblastomas[44].
ResistancetoalkylatingagentssuchasTMZhasbeenlinkedtoover-expressionofMGMT[43].
ThereforeMGMTlevelsarebeingstudiedasbiomarkersofintrinsicchemosensitivitytoalkylatingagents,suchasTMZorBCNU(carmustine).
Conversely,reducedMGMTactivityinculturedtumourcellsandhumantumoursisof‐tentheresultofepigeneticsilencingbypromotermethylationofCpGislands,whichleadstotheformationofinactivechromatinthatlimitstranscription,andthereforehigh‐erchemosensitivitytoalkylation.
Hegietal.
reportedthatof206patientswithglioblasto‐mathatweretreatedwithTMZandradiotherapy,thosewithamethylatedMGMTpromoter(45%)hadasignificantlybettersurvival[45].
Hence,MGMTpromotermethyla‐tionstatusisemergingasaprognosticfactorfortumourtherapyandiscurrentlybeingassessedforselectingglioblastomachemosensitivitytowardsTMZ[46-48].
Themecha‐nismsunderlyingincreasedMGMTpromotermethylationarecomplexandnotcomplete‐lyknown,althoughitisoneofthemoststudiedDNArepairgenes[38].
InnormalcellsMGMTpromotermethylationisuncommon,butoccursfrequentlyintumours.
Approxi‐mately25%oftumoursofmanydifferenttypes,includingnon-small-cellcarcinomaofthelung,lymphoma,headandneckcancers,andupto40%ofgliomaandcolorectaltu‐mourswerefoundtopresentCpGislandpromotermethylation[49].
SincehighMGMTexpressionresultsindrugresistancetoalkylatingagents,onestrategytoovercomeresistanceandimproveefficacyistousepseudosubstratesofMGMT,suchasO6-benzylguanine(O6-BG)orO6-(4-bromothenyl)guanine(O6-BTGorlomeguatriborPaTrin-2)whichinactivatetheenzymeandenhancecelldeath[50].
O6-BGisaspecific,potent,andnontoxicinhibitorandleadstosensitizationofcancercellstocisplatin,chloroethylatingandmethylatingagents[51,52].
ClinicaltrialsareunderwaytotestcombinationsofO6-BGwithcarmustineorTMZforthetreatmentofglioma,anaplasticglioma,lymphoma,myeloma,co‐loncancer,melanomaandsarcoma,amongothers[53].
O6-BTGpresentshigherbioavailabil‐itythanO6-BG,butalsopresentshigherhaematologicaltoxicitywhenco-administeredwithDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952493TMZcomparedtoTMZalone.
Thereforefulluseofthisinhibitormaybemoredistant[54,55].
HaematologicaltoxicitywasalsoobservedwithO6-BTGco-administeredwithdacarba‐zineinpatientswithadvancedmelanomaandothersolidtumours[56].
ThecombinationofO6-BTGandTMZwasalsoevaluatedinaphaseIclinicaltrialforadvancedsolidtumours[57],andinapilotstudyforrefractoryacuteleukaemia[58].
AphaseIclinicaltrialwasalsoconductedassociatingO6-BTGwithIrinotecanforcolorectalcancer[59].
AphaseIIclinicaltrialofO6-BTGplusTMZforstageIVmetastaticcolorectalcancerisalreadycompleted.
Thetrialwasconsideredcompletedaftertherecruitmentof19patientsduetotheabsenceofre‐sponsesandalsobecauseevidencesfromotherstudiessuggestthattheO6-BTGdosingregi‐menwasinappropriate[55].
ThesestudiesshowedaconsistentdepletionofMGMTandprovidednon-toxicdosesofO6-BGorO6-BTGtobeusedinfurtherstudies.
Thehaematolog‐icaltoxicityobservedwiththecombinationofMGMTinhibitorsandchemotherapeuticagentsmightbeattributedtoaneffectivedepletionofMGMTinoff-targetcells[60].
Addi‐tionally,theadministrationofasub-optimaldoseoftheMGMTinhibitor,atherapeuticdos‐ingschedulethatallowstherecoveryoftheMGMTactivityorthechoiceofaninadequatetreatmentforthetypeofcancercouldexplainthelackofeffectsinclinicaltrials.
Inviewofthis,tumour-targeteddeliveryofMGMTinhibitorsbythedevelopmentofspecificformula‐tionsorlocaladministration[61]couldbeadoptedtoimprovethetherapeuticefficacyofthechemotherapeuticdrugsandtotranslateintotheclinictheresultsobtainedinpreclinicalstudies.
Nonetheless,itisnotclearifclinicalapplicationofMGMTinhibitorsisaviablether‐apyinallsettings.
4.
TargetingMMRincancerdrugresistanceMMRisinvolvedinthedetectionandrepairofbase-basemispairsduringDNAreplication,smallinsertion/deletionmutationsatrepetitivemicrosatelliteregionsandalsointheregula‐tionofhomologousrecombination[62].
MMRproteinsarealsoinvolvedintherepairofDNAdamagecausedbyROSandalkylatingagents.
MMRproteinsinteractwithcompo‐nentsofotherrepairpathways,includingNER,BER,andHR,thussignallingwithotherpathwaysinresponsetoDNAdamage.
TheMMRsystemconsistsofvariousproteins.
MSH2heterodimerizeswithMSH6orMSH3toformMutSαorMutSβ,respectively,bothofwhichareATPasesthatplayacriticalroleinmismatchrecognitionandinitiationofrepair.
ThisinducesaconformationalchangeinMutS,resultinginaclampthattranslocatesonDNAinaATPdependentmanner,recruitstheMutLcomplex,whichinhumansisaheterodimerconsistingoftheMLH1andPMS2proteins,anddisplacesDNApolymeraseandPCNA,thereafterrecruitinganexonuclease(EXO1)thatdegradesthenewlysynthesizedDNAstrand[63].
OtherMMRgenes(MLH1,MLH3,PMS1,andPMS2)areinvolvedinMMR.
MLH1alsoheterodimerizeswithPMS2,PMS1,orMLH3toformMutLα,MutLβ,orMutLγ,respectively[63].
Polymeraseδ(polδ)thenpolymerizestheDNAstretchandDNALigaseIperformsligation.
MMRdeficiencyleadstoawiderangeoftumourtypes.
GermlinedeficiencyinMMRac‐countsfortheLynchsyndrome(hereditarynon-polyposiscolorectalcancer-HNPCC),inNewResearchDirectionsinDNARepair494whichalargeincreaseinfrequencyofinsertionanddeletionmutationsinsimplerepeat(mi‐crosatellite)sequences,aphenomenonknownasmicrosatelliteinstability(MSI),isobserved[64].
DNAmismatchrepairdeficiencyinsporadictumoursisseenincolonic,gastric,endo‐metrial,andothersolidtumours.
MSIisalsoassociatedwithawidevarietyofnon-HNPCCandnon-colonictumours,includingendometrial,ovarian,gastric,cervical,breast,skin,lung,prostate,andbladdertumoursaswellasglioma,leukaemia,andlymphoma[65].
DefectsinMMRarealsoassociatedwithresistancetocertainchemotherapeuticagents[66].
ResistancetoalkylatingagentssuchasTMZandprocarbazineoccurswithinactivationofMMRintumourcells[63].
MMR-deficientcellsarerelativelyresistanttomethylatingagents(upto100fold),whereascellswithafunctioningMMRsystementereitherG2arrestorapoptosis,dependingontheseverityoftheDNAdamage[67].
DownregulationofproteinsoftheMMRpathwayisassociatedwithresistancetoclinicallyimportantdrugsincludingplatinum-containingcompounds,anthracyclines,alkylatingagents,antimetabolitesandepi‐podophyllotoxins[68].
Forexample,MSH2proteindeficiencybyenhancingMSH2degradationleadstosubstantialreductioninDNAmismatchrepairandincreasedresistancetothiopurines.
Somaticdele‐tionsofgenesregulatingMSH2degradationresultinundetectablelevelsofMSH2proteininleukaemiacells,MMRdeficiencyanddrugresistance[69].
Anotheragent,etoposide,isatopoisomeraseIIalpha(TOP2A)inhibitor,whichisusedinthetreatmentofbreastcancer.
AlterationsintheexpressionofdrugtargetsorDNArepairgenesareamongtheimportantresistancemechanismsagainstTOP2Ainhibitors.
DecreaseintheexpressionlevelsofTOP2A,andtheMMRgenesMSH2andMLH1mayplaysignifi‐cantrolesinthedevelopmentofchemotherapeuticresistancetoetoposideinbreastcancer.
Thesegenesmaybeconsideredforfurtherdevelopmentofnewstrategiestoovercomere‐sistanceagainsttopoisomeraseIIinhibitors[70].
MMRisalsoinvolvedinrepairofcross-linkingagentssuchasplatinumbasedchemothera‐peutics.
Increasedtolerancetoplatinum-inducedDNAdamagecanoccurthroughlossoffunctionoftheMMRpathway.
DuringMMR,cisplatin-inducedDNAadductsarerecog‐nizedbytheMMRpathway,butarenotrepaired,givingrisetosuccessiverepaircycles,ul‐timatelytriggeringapoptosis.
ThusinMMRdeficientcells,celldeathisnotasefficient,promotingtolerancetoplatinumagents[71].
MMR-deficientcellsarealsomoretolerantto6-thioguaninetreatment,usedtotreatleukae‐mias,thanMMR-proficientcells.
Theanti-metabolite6-thioguanineisincorporatedintoDNA,whereitcanbemethylatedbyS-adenosylmethionineto6-methylthioguanine(Me6-thioguanine),whichhassimilarmiscodingpropertiesasmethylguanine[68].
Nevertheless,althoughmanypreclinicalstudiessuggestMMR-deficientcellsareresistanttoalkylatingagents,fewclinicalstudieshavebeenpublishedregardingMMRdeficiencyandresponsetoalkylatingagents.
Onthecontrary,forexample,Maxwelletal.
,[72]foundthatMMRdeficiencydoesnotseemtoberesponsibleformediatingTMZresistanceinadultma‐lignantglioma.
CoupledwiththelackofsubstantialdatalinkingpolymorphismswithintheMMRgenesandresistancetochemotherapyorradiotherapy,publishedworksuggeststhatDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952495theMMRpathwayhaslowpriorityinthequestfornewcancertherapies.
However,ongo‐ingresearchontheroleofmicroRNAsandcancerdrugresistancecouldincreaseinterestinthispathway.
PublishedworkhassuggestedthatforexamplemiR-21targetsMSH2andconsequentlyinducesresistanceto5-Fluorouracil(5-FU)incolorectalcancer[73](seethesectionofmicroRNAsanddrugresistance).
5.
TargetingBERincancerdrugresistanceBERisthemainpathwayforremovingsmall,non-helix-distortingbaselesionsfromthege‐nome.
Thus,BERtargetspredominantlybaselesionsthatariseduetooxidative,alkylation,deamination,anddepurination/depyrimidinationdamage.
Someexamplesofchemothera‐peuticagentsthatgeneratelesionsthataretargetedbyBERincludeTMZ,melphalan,dacar‐bazine/procarbazine,andstreptozotocin[33].
SomechemotherapeuticagentsalsogenerateROSasa"by-product"suchasplatinum-baseddrugs(i.
e.
oxaliplatinandcisplatin),anthra‐cyclines,(i.
e.
epirubicin,daunorubicin,doxorubicin)andpaclitaxel[31,33].
ROSinduceDNAlesionsthatarealsorepairedbytheBERpathway.
Additionally,IRproducesanum‐berofDNAlesionsthatarerepairedbytheBERpathway.
EndogenousproductionofROSalsogivesrisetoseverallesions,whicharevariableinnumberandconsequence.
Forin‐stancethehighlymutagenic8-hydroxyguanine(8-oxoG)isformedinlargequantitiesasaconsequenceofthehighoxidationpotentialofthisbase,andhasamiscodingeffect,duetoDNApolymeraseactivitywhichinsertsadenineoppositeto8-oxoG,resultinginG:CtoA:Ttransitionmutations.
TheBERpathwayisinitiatedbyoneofmanyDNAglycosylases,whichrecognizeandcata‐lyzetheremovalofdifferentdamagedbases.
AfterrecognitionofthedamagedbasebytheappropriateDNAglycosylase,itcatalyzesthecleavageofanN-glycosidicbond,thusre‐movingthedamagedbaseandcreatinganapurinicorapyrimidinicsite(APsite).
TheDNAbackboneiscleavedbyeitheraDNAAPendonucleaseoraDNAAPlyase,activitypresentinsomeglycosylases.
Thiscreatesasingle-strandedDNAnick5'totheAPsite.
ThenewlycreatednickisprocessedbytheAPendonuclease,creatingasingle-nucleotidegapintheDNA.
AtthispointBERcanproceedthroughashort-patchBER,wherepolymeraseβ(polβ)introducesasinglenucleotidepasttheabasicsiteandLigaseIIIαsealstheDNAnick,orthroughalong-patchBER,wherePolymeraseδ/εintroducestwotoeightnucleotidespasttheabasicsite.
TheresultingoverhangDNAisexcisedbyFEN1endonucleaseandthenicksealedbyDNAligaseI[74].
Inadditiontotheseenzymes,anumberofaccessoryproteinsareinvolvedinBER,includingtheX-raycross-complementationgroup1protein(XRCC1),PARP1,theproliferatingcellnuclearantigen(PCNA),andtheheterotrimertermed9-1-1,whichfunctioninscaffoldsforthecoreBERenzymes[75].
PreclinicalevidenceshaveimpliedtheBERpathwayintherepairofDNAlesionsinducedbyantimetabolites,monofunctionalalkylatingdrugs,radiotherapyandradiomimeticagents.
Moreover,BERmodulationmayalsosensitizecancercellstotheeffectofchemother‐apeuticdrugsthatareabletogenerateROS[31,33].
Therefore,targetingBERwithinhibitorsNewResearchDirectionsinDNARepair496ofthemultifunctionalAPEndonuclease1andDNApolβisanattractivefieldtothedevel‐opmentofnoveltherapeuticcompounds.
SomestudieshavefoundderegulationofBERgenesintumours.
Forexamplepolβhasbeenshowntobeoverexpressedinavarietyoftumourcells[76].
N-methylpurineDNAglycosy‐lase(MPG)overexpression,togetherwithinhibitionofBER,sensitizesgliomacellstotheal‐kylatingagentTMZinaDNApolβ-dependentmanner,suggestingthattheexpressionlevelofbothMPGandpolβmightbeusedtopredicttheeffectivenessofBERinhibitionandPARP-mediatedpotentiationofTMZincancertreatment[77].
Werecentlyobservedanin‐creaseinexpressionoftheBERgenesMDB4andNTHL1inImatinibresistantK562leukae‐miacells,andknockdownoftheirexpressioninresistantcellsusingsiRNAdecreasedcellsurvivalaftertreatmentwithdoxorubicin[78].
Nevertheless,theinvolvementofderegulat‐edBERcomponentsinchemotherapyresistanceisnotcompletelyevidentatpresent,exceptforPARP,andtheAPendonucleases.
Thefollowingtextshalldescribeongoingresearchtar‐getingthesecomponentsoftheBERpathway.
ThemajorAPendonucleaseinmammaliancellsisapurinic/apyrimidinicendonuclease1/redox-factor-1(APE1/Ref-1,alsocalledAPEX1),andhasbeenfoundtobeelevatedinanumberofcancerssuchasovarian[79],prostate[80],osteosarcoma[81]andtesticularcan‐cer[82].
Over-expressionofAPE1invitroledtoincreasedprotectionagainstbleomycin[82].
ThuselevatedlevelsofAPE1incancercellshavebeenpostulatedtobeareasonforchemo‐therapeuticresistance[81,83,84].
InhibitionofAPE1hasbeenshowntoincreasecellkillingandapoptosisandalsotosensitizecancercellstochemotherapeuticagents,andthusAPE1isconsideredasamoleculartargetintherapeutics[85,86].
APE1endonucleaseactivityisindirectlyinhibitedbyblockedAPsitesthatresultfromthebindingofthesmallmoleculemethoxyamine(MX)totheDNA.
WiththeAPE1'ssubstrateunavailable,BERcannotproceedandthecytotoxicabasicsitesaccumulateinthecell,eventuallyleadingtocelldeath.
ThepromisingresultsfrominvitroandinvivoexperimentsshowingMXsensitizationtothecytotoxiceffectofTMZ[87-90],carmustine[91],pemetrexed[92]and5-iodo-2'-deoxyuridine(IdUrd)aswellasapotentiationofIdUrd-mediatedradiosensitization[93,94],inmultiplesolidtumoursmodels,providedtheproof-of-concepttoconductclinicaltrialswithMXasadjuvanttherapyofanticanceragents.
APhaseIclinicaltrialofpemetrexedandoralmethoxyaminehydrochloride(TRC102)inpatientswithadvancedrefractorycancerisalreadycompleted[95].
Accord‐ingtotheauthors,thisdrugiswelltoleratedafterdailyoraladministrationandpotenti‐atestheactivityofchemotherapy.
Safety,pharmacokineticandpharmacodynamicprofileofMXwasalsoevaluatedincombinationwithTMZinaPhaseIclinicaltrialforpa‐tientswithadvancedsolidtumours[96].
Currently,twoclinicaltrials(PhaseI)arere‐cruitingpatientstostudythesideeffectsandthebestdoseofMXtobeadministeredincombinationwithTMZandfludarabinephosphateinpatientswithadvancedsolidtu‐moursandrelapsedorrefractoryhematologicmalignancies,respectively.
InviewoftheemergingrolesofAPE1,manyeffortshavebeenmadetodevelopsmallmole‐culeinhibitorsthatcanbetranslatedtotheclinic.
Insilicobasedapproacheswithdesignofpharmacophoremodels[97,98]andhigh-throughputscreeningofseveralcommerciallyDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952497availablelibrariesofcompoundshavebeenperformedtoidentifyapharmacologicallyac‐tiveinhibitorforAPE1[86,99-102].
LucanthoneactsasadirectinhibitorofAPE1butalsointeractswithothercellulartargetsandtheassociatedtoxicityhinderstheirtherapeuticuse[103,104].
CRT0044876wasidentifiedbyafluorescence-basedhigh-throughputassayandshowedpromisingresultsininvitrostudies[105].
However,someauthorswerenotabletoreproducethereportedeffectsofthiscompound[85].
HypersensitivityofDNApolβ-nullcellstomethylmethanesulfonate(MMS),aDNA-meth‐ylatingagent,displayedanotherpotentialtargetinBER[106].
Severalsmall-moleculeinhibi‐torsofDNApolβhavebeenidentifiedandmanyofthesecompoundsarenaturalproducts,suchaskoetjapicacid(KJA),atriterpenoid.
PamoicacidwasoneofthefirstsyntheticsmallmoleculeinhibitorsofDNApolβtobecharacterizedandismoreactivethantheformercompound[107].
Nevertheless,theactuallyknowninhibitorsofDNApolβhavelowpoten‐cyandspecificitythatmakethemweakcandidatestodrugdevelopment(foracomprehen‐sivereviewsee[108]).
InviewofthepreclinicaldatathatsuggestanimportantroleofDNAPolβintherepairofchemotherapeutic-inducedDNAdamage,thedesignofeffectiveDNAPolβinhibitorsisanattractiveresearcharea.
InwhatconcernsPARP1,thisenzymeisaDNAdamagesensorthatbindstoDNAbreakstoactivatetherepairpathways.
PARP1isnotdirectlyinvolvedintherepairofthelesionsbutisessentialtosignalthedamageandtocoordinatethefunctionsofsever‐alBERandDSBrepairproteins.
PARPinhibitorshavebeenthoroughlydevelopedandseveralreviewspaperspublishedunderthistopic.
ForarecentcomprehensivereviewonPARPinhibitorsseeJavleetal[109].
PARPinhibitorswerefirstevaluatedinclinicaltri‐alsaschemosensitizers.
AfterAG014699combinationwithTMZ[110],otherPARPinhibi‐tors,specificallyINO-1001,ABT-888andAZD2281werealsotestedasadjuvanttherapyofmultipleanticanceragentssuchasgemcitabine,carboplatin,TMZorchemotherapeuticcombinations(e.
g.
cisplatinplusgemcitabine)[111].
Currently,severalPARPinhibitorsarebeingevaluatedinclinicaltrials,eitherincombinationwithchemotherapeuticdrugsorinmonotherapy[28,109,112-117].
Someofthesechemicalsshowedanenhancementofthetoxicityinnormaltissuesthatre‐quireddoseadjustmentsandoptimizationofthetherapeuticschedule.
Interestingly,pre‐clinicalandclinicaldatarevealedthatPARPinhibitorsassingleagentscouldbelesstoxictothenormalcellsandaremoreeffectiveinkillingBRCA1-andBRCA2-mutatedcancercellssincethesecellsaredefectiveinHR,thebackuppathwayresponsiblefortherepairofDSBsgeneratedafterPARPchemicalinhibition.
Similarly,mutationsinotherproteinsrelatedtotheDNAdamageresponse,suchasATMandPTENhavealsobeenassociatedtodefectsinDSBrepairandmaybeinvolvedinanincreasedsensitivitytoPARPinhibitors[118-120].
ThesefindingsledtoanovelpotentialtherapeuticindicationoftheDNArepairinhibitorsassingleagentsincancertherapywhichiscurrentlybeingevaluatedinclinicaltrials[121].
ThissyntheticlethalapproachwasalsoreportedinaninvitrostudywithAPE1inhibitorsinBRCAandATMdeficientcells[116,122].
Recently,negativeresultsfromthefirstphaseIIIclinicaltrialinbreastcancerpatientswithacombinationofiniparib(BSI-201)andgemcitabine/carboplatinwerereported[123].
TheNewResearchDirectionsinDNARepair498mechanismofactionofthisinhibitorisnotfullyunderstood,anissuethatshouldbefurtherclarified.
Nonetheless,promisingpositiveoutcomeshavealreadybeensuggestedwithotherPARPinhibitors[124,125].
AfurtherunderstandingofthecomplexPARPinteractome,thediscoveryofPARP1specificsmallmoleculeinhibitorsandanaccurateselectionofthebestcandidatestothetreatmentisstillneededtoimprovethequalityofinformationobtainedfrompreclinicalandclinicaltrialsandtopromotethedevelopmentofcurrentlyknownPARPinhibitorsaswelltodiscovernovelcompounds.
6.
TargetingNERindrugresistanceNERrepairsDNAlesionswhichalterthehelicalstructureoftheDNAmoleculeandin‐terferewithDNAreplicationandtranscription,suchasbulkyadductsandcross-linkingagents[2].
Briefly,NERconsistsoftherecognitionofDNAdamageanddemarcationofthespecificareaaffected,followedbytheformationofacomplextounwindthedam‐agedportionandexcisea24-32oligonucleotidesectionthatcontainsthelesion.
Finally,theexcisednucleotidesareresynthesizedandligated.
TwoNERsub-pathwaysexistwithpartlydistinctsubstratespecificity:globalgenomenucleotideexcisionrepair(GGR)sur‐veystheentiregenomefordistortinglesionsandtranscription-coupledrepair(TCR)fo‐cusesspecificallyinthetranscribedstrandofexpressedgenes,bytargetingdamagethatblockselongatingRNApolymerases.
Intotalmorethan30proteinsparticipateinNER[126].
ThegenesinvolvedinGGRareDNAdamagerecognitionbyXPC-HR23Bcom‐plex,lesiondemarcationandverificationbyaTFIIHcomplex,assemblyofapre-incisioncomplex(RPA,XPAandXPG),DNAopeningbyXPBandXPDhelicases,dualincisionbyERCC1-XPFandXPGendonucleases,releaseoftheexcisedoligomer,repairsynthesistofillintheresultinggap,andligationbyligaseI.
DefectsintheproteinsinvolvedinNERresultinthreeautosomalrecessivedisordersXP,CS,andTTD.
ThemostrelevantclassofchemotherapeuticsassociatedwithNERistheplatinum-basedgroupofagents.
Platinum-basedchemotherapyhasbeenusedforthetreatmentofawidevarietyofsolidtumoursincludinglung,headandneck,ovarian,cervical,andtes‐ticularcancerformanyyears[127].
TheseagentsinteractwithDNAtoformpredomi‐nantlyintra-strandcross-linkDNAadductsthattriggeraseriesofintracellulareventsthatultimatelyresultincelldeath.
Themoststudiedplatinumbasedcancertherapeuticsarecisplatinandthelesstoxiccarboplatinandoxaliplatin,buttherehasbeenaresur‐genceinthedevelopmentofplatinumbaseddrugs,andmoreplatinumbasedchemo‐therapeuticsareinclinicaltrials[128].
Thebasicmechanismofactionofcisplatin(andcarboplatin)involvescovalentbindingtopurineDNAbases:platinumbindingtotheN7positionoftheimidazoleringofthepu‐rinebasesofDNA—guanine(G)andadenine(A)—toformeithermonofunctionalorbifunctionaladducts.
Inthecaseofcisplatin,mostoccuronthesameDNAstrandandinvolvebasesadjacenttooneanother,andarethereforeknownasintra-strandadductsorcrosslinks,namelyGpG1,2intra-strand(60–65%ofalladducts)andApG1,2intra-DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952499strand(20–25%)whichprimarilyleadstocellularapoptosis[128].
TheseDNAlesionsarerepairedbytheNERpathway.
Cisplatinhasbeenusedsuccessfullyastherapytotreatmetastatictesticularcancerwith>90%curerate.
ThehighsensitivityoftesticulartumourcellsisattributedtoreducedDNA-re‐paircapacityinresponsetoplatinum–DNAadducts[129].
ExtractsfromtesticularcancercellshadlowconstitutiveNERcapacityand,inparticular,lowlevelsoftheproteinXPA[130].
FurtherstudieshaveshownlowlevelsofXPAandotherNERproteins(XPFandERCC1),intesticularcancers.
ThissuggestedthatreducingNERcapacityinacancerholdsthepotentialtosensitizethecancertocisplatin.
ParallelstudiesrevealedthatincreasedDNArepaircapacitywasacommonfunctionincancersthatwereinherentlyresistanttocis‐platinorthatacquiredresistancefollowingtreatment[130].
Clinicalstudiesinovariancancerpatientshavecorrelatedincreasedexcisionrepaircross-complementationgroup1–(ERCC1)mRNAlevelswithclinicalresistancetoplatinumbasedchemotherapy[131,132].
Inmetastaticcolorectalcancerpatients,higherERCC1ex‐pressionlevelswereconsideredaspredictiveforlowersurvivalrateswhentreatedwithox‐aliplatinincombinationwith5-fluorouracil,suggestingthatenhancedDNArepairdecreasestheefficacyofplatinum-basedtreatment[133].
Inanotherstudyasubgroupof761patientswithmetastaticlungcancertreatedwithaplatinumbasedcompoundwereretro‐spectivelyevaluatedbyimmunohistochemicalanalysisofERCC1.
Thisstudyshowedastat‐isticallysignificantsurvivalbenefitinpatientswithlowlevelsofERCC1whohadreceivedplatinumbasedchemotherapy,comparedtopatientswithlowlevelsofERCC1whodidnotreceivechemotherapyandpatientswithhighlevelsofERCC1whoreceivedcisplatinche‐motherapy[134].
Also,lowERCC1expressioncorrelatedwithprolongedsurvivalaftercis‐platinplusgemcitabinechemotherapyinnon-smallcelllungcancer(NSCLC)[135].
Hence,itishypothesizedthathighexpressionoftheERCC1genemightbeapositiveprog‐nosticfactor,andcouldpredictdecreasedsensitivitytoplatinum-basedchemotherapy.
Ex‐pressionofERCC1hasbeenusedtostratifypatientstreatedwithplatinumbasedchemotherapeuticswithsomesuccess,andalsotopredictimprovedsurvivalinplatinumtreatedpatients[136].
Nonetheless,resultsfromthepublisheddataareinconsistent.
Tode‐riveamorepreciseestimationoftherelationshipbetweenERCC1andtheprognosisandpredictiveresponsetochemotherapyofNSCLC,ameta-analysiswasperformedandresultsindicatedthathighERCC1expressionmightindeedbeafavourableprognosticandadrugresistancepredictivefactorforNSCLC[137].
Otherstudieswithdifferenttumour/chemotherapyassociationshaveshownthatERCC1mRNAexpressionintumoursmaybeapredictivemarkerofsurvivalforIrinotecan-resist‐antmetastaticcolorectalcancerreceiving5-FUandOxaliplatincombinationchemotherapy[133].
InthisstudypatientswhosetumourshadlowERCC1mRNAexpressionhadasignifi‐cantlylongermediansurvivalthanthosewithhighERCC1expression.
OthergenesinvolvedinNERhavebeenshowntoinfluencedrugresistance.
Forexample,increasedexpressionofexcisionrepaircross-complementationgroup4(ERCC4orXPF)wasobservedinhydroxycamptothecin(HCPT)treatedbladdercancertissuecomparedtoun‐NewResearchDirectionsinDNARepair500treatedsamples.
ComplementaryinvitrostudiesshowedthatenhancedERCC4expressiondecreasedthesensitivityofbladderT24cellsand5637cellstoHCPT,whereasaftergenesi‐lencingofERCC4thechemotherapeuticresistanceofbladdercancercellstoHCPTwassig‐nificantlydecreased[138].
SincetheNERpathwayiscrucialfortherepairofbulkyadductsandcross-linkingagentsinnormalcells,thedevelopmentandapplicationofNERinhibitorsinclinicalsettingsisscarce,althoughpreclinicaldatashowthatthemanipulationofthispathwaycouldbearelevantstrategyincancerchemotherapy.
Forexample,preclinicalstudieshavedemonstratedthatthechemotherapeuticactionoftheplatinumagentoxaliplatinisimprovedwhencombinedwithcetuximab,achimericIgG1monoclonalantibodytargetingtheepidermalgrowthfac‐torreceptor.
ThisantibodyhasbeenshowntoreducetheexpressionofERCC4andERCC1.
Aconcomitantincreaseintheaccumulationofplatinumandapurinic/apyrimidinicsitesonDNAduringoxaliplatintreatmentwasobserved,thusleadingtoanincreaseinapoptosis[139,140].
Theseinterestingresultsaresuggestivethattargetingotherpathwaysthatregu‐lateexpressionofDNArepairgenescouldbeapromisingstrategy.
7.
HRanddrugresistanceHRrepairsDSBs,whichoccurthroughexposuretovariouschemotherapeuticagents,in‐cludingIR,topoisomeraseinhibitorsandDNAcrosslinkingagents(e.
g.
mitomycin,campto‐thecins,etoposide,doxorubicin,daunorubicinandbleomycin).
HRisalsorecruitedtorestartstalledreplicationforksandtorepairICL,therepairofwhichalsoinvolvestheFAproteincomplex.
HRensurestheaccuraterepairofDSBsbyusingahomologousundamagedDNAstrandfromanintactsisterchromatidasatemplateforDNApolymerasetoextendpastthebreak,andisthusrestrictedtolateSandG2ofthecellcycle.
ComponentsofHRincludetheRADgroupofproteins(includingRAD50,RAD51,RAD52,andRAD54),RPA,XRCC2,XRCC3,andtheBRCAproteins.
Briefly,HRoccursthroughpre-synapsis,preparationofarecombinationproficientDNAend;synapsis,formationofajointmoleculebetweenthere‐combinationproficientDNAendandadouble-strandedhomologoustemplateDNA;post-synapsisandresolution,repairofDNAstrandsandseparationoftherecombinedDNAmolecules[19].
DSBscanalsoberepairedbyNHEJthatdonotutilizesignificanthomologyatthebrokenends.
InNHEJ,DSBsarerecognizedbytheKuproteinthatthenbindsandac‐tivatestheproteinkinaseDNA-PKcs,leadingtorecruitmentandactivationofend-process‐ingenzymes,polymerasesandDNAligaseIV.
WhereasHRisrestrictedtolateSandG2,NHEJfunctionsinallphasesofthecellcycleandligatesbrokenDNAendswithouttheneedofanundamagedtemplate.
FollowingDNAlesionsinitialcheckpointsignallingisperformedbythekinasesATRandATM,twophosphatidylinositol3-kinasefamilymembers.
Activationofthesekinasesleadstoactivationoftheeffectorkinases,checkpointkinases1and2(Chk1andChk2;serine/threoninekinases).
TheactivatedeffectorkinasesarethenabletotransientlydelaycellcycleprogressionthroughtheG1,S,ortheG2phasessothatDNAcanbeefficientlyrepaired.
TheDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952501ATM/Chk2pathwaypredominantlyregulatestheG1checkpointandtheATR/Chk1path‐waytheSandG2checkpoints.
However,thereiscross-talkbetweenthepathwaysimplyingaroleforbothATRandATMpathwaysinallcellcyclecheckpoints.
Inadditiontodirectlyregulatingthecellcycle,thepathwaysalsoaffectDNArepair,transcription,chromatinreg‐ulation,andcelldeath.
Manydetailsofthesepathwaysarenotfullyknown.
OneconsequenceofDSBsisthelocalizedalterationofchromatinadjacenttoDSBsinordertofacilitaterecruitmentofrepairproteins.
Forexamples,ATMnotonlyphosphorylatesDNArepairproteinsrecruitedtoDNAendsbutalsothehistonevariantH2AXinnucleo‐somesadjacenttoDSBs,whichisalsophosphorylatedbyDNA-dependentproteinkinase(DNA-PK),anotherproteinkinaseactivatedbyDSBs.
PhosphorylatedH2AX(knownasγ-H2AX)aroundDSBsfacilitatestherecruitmentofanumberofDNArepairproteinsandchromatinmodulatingfactors.
Thepresenceoflargepatchesofγ-H2AXaroundaDSBhasmadeitsdetectionbyfluorescenttaggedantibodiesabiomarkerforDSBs[141,142].
ThereisaccumulatingevidencefortheexistenceofHRdefectsnotonlyinfamilialcancersbutalsoinsporadiccancers.
Mutationsorepigeneticalterationshavebeenobservedinsev‐eralgenesknowntobeinvolvedinHRregulationandrepair,suchasBRCA1andBRCA2.
FunctionalanalysisofhumancancertissuesandcancercelllineshasrevealedHRdeficien‐cy,chromatid-typechromosomalaberrations,severeICLhypersensitivity,andimpairedfor‐mationofdamage-inducedRAD51foci.
Forexample,althoughgeneticmutationsinBRCA1orBRCA2areonlyrarelyfoundinsporadictumors,incontrasttofamilialbreastandovari‐ancancers,epigeneticgeneinactivationoftheBRCA1promoterisafairlycommoneventinsporadicbreastcancers,withaberrantmethylationbeingdetectedin11to14%ofcases[143].
Non-triple-negativesporadicbreastcancersmayalsoharborHRdefects.
Ithasbeensuggestedthat~20%ofthesecancersaredefectiveinHRasmeasuredbyanimpairedabilitytomountRAD51fociinresponsetochemotherapy[144].
Thereisemergingevidencethatapproximatelyuptoonefifthofnon-familialbreastcancersharbourHRdefectsthatmaybeusefultargetsfortherapy.
TheBRCA1andBRCA2proteinsareinvolvedinHR,inassociationwithFAproteins,form‐ingacomplexDNAdamageresponsenetwork[145].
BRCA1expressionlevelshavebeendemonstratedtobeabiomarkerofsurvivalfollowingcisplatin-basedchemotherapyforNSCLCandovariancancer,suggestingthatthisgenecouldbeinvolvedinresponsetoplati‐numtherapy[146,147].
InvitrostudiesindicatethatlossofBRCA1orBRCA2increasessen‐sitivitytoagentsthatcauseDSBssuchasbleomycinand/orICLsincludingplatinumagents.
Conversely,lossofBRCA1orBRCA2mayincreaseresistancetomicrotubuleinterferingagentssuchastaxanesandvincristine[148,149].
Incontrast,BRCA1mayincreasesensitivitytospindlepoisonsbyactivatingthemitoticspindlecheckpointandsignallingthroughaproapoptoticpathway.
ThisdualroleofincreasingapoptosisandthereforesensitivitytospindlepoisonsandalsopromotingDNArepairandcellsurvivalaftertreatmentwithDNA-damagingdrugsmayinfluencetheresponseofbreastandovariancancercellstotreatment[150].
Chemotherapyinbreastandovariancancersisattainedbytreatmentwithplatinumbasedcompoundsandanthracyclinesandalsotaxanes,allofwhichinducebothNewResearchDirectionsinDNARepair502SSBsandDSBs.
EffortsareunderwaytouseBCRA1asapredictivemarkerforchemothera‐pycustomizationandresponse[151].
Regardingothertypesofcancer,BRCA1promoterhypermethylationisalsofoundinap‐proximately5-30%ofsporadicovariancancers.
Also,mutationsinBRCA1andBRCA2haverecentlybeenfoundinupto20%ofunselectedovariancancers[152].
Thus,theseHRdefi‐cientcancersareviabletargetsforsyntheticlethalityapproacheswithPARPinhibitors.
De‐fectsintheFA/BRCApathwayaswellasATMdefectshavebeendescribedinavarietyofothermalignancies,suchasprostaticadenocarcinoma,colorectalcancer,leukaemia,lym‐phoma,andmedulloblastoma[153,154].
However,itremainstobeseenwhetherthesede‐fectscanbetargetedeffectivelyintheclinic.
Single-agentchemotherapywithanitrogenmustard,usuallyChlorambucil,isthestandardinitialtherapyforChroniclymphocyticleukaemia(CLL)andatleast60–80%ofpatientsre‐spondbuteventuallyallpatientsbecomeresistanttotheseagents.
XRCC3proteinlevelsandDNA-damageinducedRAD51focicorrelateswithchlorambucildrugresistanceinlympho‐cytesfromCLLpatientsandwithmelphalanandcisplatinresistanceinepithelialtumorcelllines,indicatingthatincreasedHRcanbeinvolvedindrugresistancetotheseagents[155].
AnothercomponentoftheHRpathway,RAD51,hasbeenfoundtobeincreasedinex‐pressioninawiderangeofhumantumors,mostlikelycontributingtodrugresistanceofthesetumors.
Over-expressionofRAD51indifferentcelltypesleadstoincreasedhomol‐ogousrecombinationandincreasedresistancetoDNAdamagingagentstodisruptionofthecellcycleandapoptoticcelldeath.
RAD51expressionisincreasedinp53-negativecells,andsinceTP53isoftenmutatedintumorcells,thereisatendencyforRAD51tobeoverexpressedintumorcells,leadingtoincreasedresistancetoDNAdamageanddrugsusedinchemotherapies[156].
Chronicmyeloidleukaemia(CML)celllinesexpressingthefusionproteinBCR-ABL1uti‐lizeanalternativenon-homologousend-joiningpathway(ALTNHEJ)torepairDSBs.
TheexpressionlevelsofPARP1andDNAligaseIIIαservedasbiomarkerstoidentifyasubgroupofCMLpatientswhomaybecandidatesfortherapiesthattargettheALTNHEJpathwaywhentreatmentwithTKIshasfailed[157].
Tamoxifen-andaromatase-re‐sistantderivativesofMCF7cellsandEstrogenReceptor-/ProgesteroneReceptor-(ER-/PR-)cellshavehighersteady-statelevelsofDNAligaseIIIαandincreasedlevelsofPARP1,anotherALTNHEJcomponent.
Notably,therapy-resistantderivativesofMCF7cellsandER-/PR-cellsexhibitedsignificantlyincreasedsensitivitytoacombinationofPARPandDNAligaseIIIinhibitorsthatincreasedthenumberofDSBs.
Thus,ALTNHEJmaybeanoveltherapeutictargetinbreastcancersthatareresistanttofrontlinetherapiesandchangesinNHEJproteinlevelsmayserveasbiomarkerstoidentifytumorsthatarecan‐didatesforthistherapeuticapproach[158].
AnotherinterestingapproachinthisfieldistotargetcomponentsoftheDNAdamageresponse,namelyDNAdamagesignallingandcell-cyclecheckpoints[34].
Themembersofthephosphatidylinositol(PI)3-kinase-like(PIKK)familyperformcrucialrolesintheactivationofDSBrepairpathways,namelyinHRandNHEJ.
ATM,aPIKKfamilymem‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952503ber,isaDSBsignallingproteinmainlyimplicatedinthephosphorylationofeffectorpro‐teinsfromHR.
ATMhasbeenalsoinvolvedintheregulationofNHEJ.
KU55933,2-morpholin-4-yl-6-thianthren-1-yl-pyran-4-oneisaspecificandpotentsmall-moleculeinhibitorofATMidentifiedbyscreeningofacombinatoriallibrary.
Preclinicalstudieshaveshownanincreaseinthecytotoxicityofmultiplechemotherapeuticdrugsasdoxor‐ubicin,etoposide,camptothecinandionizingradiation[159,160]whiletheUV-inducedcellulareffectswerenotmodified.
Morerecently,KU60019,animprovedanalogueofKU55933,wasdeveloped.
Besidesitsradiosensitizingproperties,invitrostudiesrevealedthatKU60019mayalsoimpairthemigrationandinvasionoftumorcellsbyinhibitingATM-mediatedAKTphosphorylation[161].
DNA-PKisalsoatargettothedevelopmentofchemo-andradiosensitizers[162].
Infact,theidentificationofspecificsmallmoleculemodulatorsofDNA-PK[163-165],namelyNU7441andNU7026,wasshowntopotentiatetheeffectsofionizingradiationaswellaschemother‐apeuticagentsinhumantumorcelllinesandininvivoxenograftmodels.
AnotherexampleisthedevelopmentofAZD7762,whichpotentlyinhibitsChk1andChk2,abrogatesDNAdamage-inducedSandG2checkpoints,enhancestheefficacyofgemcita‐bineandtopotecan,andmodulatesdownstreamcheckpointpathwayproteins[166].
Thisagenthasbeenevaluatedinclinicaltrials,howeverduetoaninadequateresponsethedrughasbeendiscontinuedin2011(http://www.
astrazenecaclinicaltrials.
com).
8.
MicroRNAsandchemotherapyresistanceMicroRNAs(miRs)aresmallnon-codingRNAs(19to25nucleotides)thatregulategeneexpressionbybindingto3'untranslatedregion(UTR)ofseveralmRNAs,thusblockingtranslation.
Recently,itwasalsoshownthatmiRscanactbybindingtoopenreadingframesor5'UTRofmRNAs,asrevisedbyIorioandCroce[167].
DuetosmallsizeandincompletecomplementaritytomRNA,onemiRcanhaveawidespreadeffectonthetranscriptomeofacell,actingasahallmarkofseveraldiseases,includingcancer.
Nu‐merousstudieshavebeenperformedregardingbiogenesisandfunctionofmiRs,beingrevisedelsewhere[168-170].
InvitroandinvivostudieshavesuggestedthatmiRNAsmightbeusefulasdiagnosticandprognosticmarkers,andrecentdatasuggestthatmiR‐NAprofilingcanbeusedfortumortyping.
AlthoughitiswellestablishedthatmiRshaveanimportantroleincancer,thecomplexityoftheiractionremainstobeunderstoodandquestionsregardingtheiruseascancertherapyneedfurtherinvestigation.
ThestrongpleiotropyofmiRsinderegulatingnormalcellularhomeostasisduetomisexpression,hasledinvestigatorstobelievethattheyarevaluabletar‐getsforcancertherapyandconsequentlyfordrugresistance.
Twomajorapproachesforus‐ingmiRsastherapeuticscanbedescribed.
First,miRscanbeusedassinglemoleculesorcombinedinordertotargetoneormultipletranscripts.
Inthisapproach,amiRorasetofmiRsareantagonizedormimickedtoaltermiRlevelsandconsequentlychangetheproteinNewResearchDirectionsinDNARepair504outcomeinacancercell.
Second,miRscanactasmodulatorsofcellsensitivityforcancertherapy[167,171].
Thissecondapproachwillbeourfocus.
ManystudiesregardingmiRsexpressionpatternsincancercellshavebeenperformed.
ThesestudiesnotonlyallowinvestigatorstodeterminenovelbiomarkersforabetterandeasilyprognosticationofseveraltypesofcancerbutalsothefunctionalroleofthesamemiRs.
ThesecangiveustheknowledgeifthelossorgainofmiRfunctioninter‐fereswiththeoriginalbalanceofproteinlevelswhichmaybeimportant,butnotonly,indrugresponseandconsequentlyleadtodrugresistance.
SincemiRsexpressionseemstobetissue,gradeandstagespecific,theectopicexpressionorrepressionofmiRsinconjugationwithcancertherapyseemspromising.
Forthatreason,recentstudiesthatevaluatemiRexpressionprofilesofsensitiveandresistantcelllineshavebeenmadeinordertofindthekeymiRsignaturesrelatedtodrugresponse,whichnotonlypromotefurtheranalysisofthemechanismsofcancerdrugresistance,butalsoallowthediscov‐eryofnewdrugtargetsandindividualizedmedicine.
AlthoughthestudyofthetherapeuticpotentialofmiRsisstillrecent,severalstudieshavebeenpublishedandcompiled.
Forexample,Tianetal.
[172]andKutanzietal.
[173],publish‐edcompilationsofseveralstudiesreportinginfluenceofmiRsinmechanismsofdrugresist‐anceandhowtheycanmodulatedrugresponseinbreastcancer.
WithregardtomiRsandmodulationofdrugresistancethroughregulationofDNAdamageandrepairgenes,studiesarescarce.
ItisknownthatmiRshaveanimportantroleinDNAdamageresponse,whichincludesDNArepair[174,175].
OneexamplehowmiRscaninflu‐encedrugresistancethroughDNArepairisdemonstratedbyValerieetal.
[73].
TheauthorsshowedthatmiR-21targetsMSH2andconsequentlyinducesresistanceto5-FUincolorectalcancer.
SincemiR-21hasapleiotropiceffect,itispossiblethatitcouldregulateothergenesassociatedwithdrugresistance.
However,theimpactofMSH2seemstobeofextremeim‐portanceonacquired5-FUresistancesincewhenknockedoutcellsforMSH2aretransfectedwithmiR-21,cell-cyclearrestorapoptosisisnotaltered.
Theseresultsshowthattheinhibi‐tionofmiR-21actionmightrepresentanimportanttreatmenttoovercome5-FUresistance.
AcorrelationbetweenmiR-21andMSH2inbreastcancerwasalsofound[176].
Itisrecog‐nizedthatTGF-βisapromoterofmiR-21processingthroughtheinteractionwiththeSMADandDROSHAcomplex.
Ontheotherhand,MSH2isaproventargetofmiR-21.
Thus,TGF-βinhibitsMSH2geneexpressionandconsequentlyincreasesdrugresistance.
Indeed,tofindoutifTGF-βcontributestodrugresistancethroughMSH2,theauthorstestedtheresponseofbreastcancerMDA-MB-231celllinetocisplatin,methylmethanesulfonate(MMS)anddoxorubicininthepresenceandabsenceofTGF-β.
ExposuretoTGF-βfor24hincreasedcellviabilityupontreatmentwiththeseDNAdamagingagentsandknockdownofMSH2in‐ducedresistancetobothcisplatinanddoxorubicin.
Incontrast,transfectionoftheanti-miR-21enhancedtheeffectofcisplatininMDA-MB-231cells.
AnotherexampleofmiRinfluenceinDNArepairandconsequentdrugresponseismiR-182thattargetsBRCA1.
MoskwaandcolleaguesshowedthatectopicexpressionofmiR-182re‐pressesBRCA1proteinexpressionandsensitizesbreastcancercellstoPARPinhibitors[177].
However,PARPinhibitorsaremostlyusedinpatientswithBRCA1inheritedmuta‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952505tions.
Therefore,thequestionifPARPinhibitorsareusefultherapeuticdrugsinsporadicbreastcancerrises.
Theoretically,ifadministratedwithBRCA1repressorssuchasmiR-182,PARPinhibitorscanhavethesameeffectasininheritedbreastcancer.
Furtherstudiesneedtobedoneinordertoclarifythisissue.
Asdescribedpreviously,MGMThasDNArepairactivityinsofarasitcanremovemutagen‐icO6-alkylguanineinducedbyalkylatingagents.
AlthoughTMZhasbeenwidelyusedinglioblastomamultiforme(GBM),manypatientsbecomeorareresistanttothischemothera‐pyagent,sinceMGMTcanrepairtheDNAdamageinducedbyTMZ.
Epigeneticregulationmechanisms,suchasmethylationoftheMGMTgenepromotercansensitizecancercellstoalkylatingchemotherapeuticdrugs.
GlioblastomapatientswithpositivemethylationstatusofMGMTgenepromoterhavebeenreportedtopresentabetterresponsetoTMZtreatment[44],buttheseresultshavenotbeenconfirmedbyotherstudies,andthereforeresultsareambiguous[178].
Indeed,somepatientswithunmethylatedstatusofMGMTpromotergenealsohavegoodresponsetoTMZ,whichpointsouttootherregulatorymechanismsofMGMTexpression[179].
Thus,miRsappearasgoodalternativeregulationcandidatesofMGMTexpressionlevels.
RecentevidencealsosuggeststhatthemiR-181familymightbeassociatedtodrugresponse[180].
Theauthorsfoundthatglioblastomapatientswithlowex‐pressionofmiR-181bandmiR-181chaveabetterresponsetoTMZ.
Onthecontrary,miR-181dseemstopost-transcriptionallyregulateMGMTsincebothdirectlyinteractandin‐verselycorrelateinrelationtoexpressionlevels[181].
ThisfactisimportantbecauseitcouldbeapredictivebiomarkerforchemotherapyresponseinGBM.
LakomyandcollaboratorsfoundthathighexpressionofmiR-195andmiR-196bissignificantlyassociatedwithlongersurvivalofGBMpatientsandmiR-21andmiR-181cwithhighriskGBMpatients[182].
HowevernoneofthesemiRswereassociatedwithMGMTgenepromoterstatus.
AltogetherthepotentialforuseofmiRsincancertherapyishigh,soarethechallenges,sinceeachmiRcantargetuptohundredsofmRNAtargets.
Therapidelucidationoftheroletheyplayincancersuggestthattranslationofthisknowledgewillrapidlyreachtheclinic.
9.
PhytochemicalsasalternativetherapiesagainstdrugresistanceAsdiscussedpreviously,frequentlynoveltherapeuticsthatshowpromisingresultsinpre‐clinicalassaysrevealunacceptabletoxicityinclinicaltrials.
Sincecancercellsfrequentlypresentderegulationofmultiplecellularpathways,targetingmultiplepathwaysseemsmorepromisingthanusingsingleagentsthattargetsinglepathways.
Inrecentyearsnaturaldietarycompoundssuchascurcumin,resveratrolandsoyisoflavonessuchasgenistein,havereceivedattentionduetothefactthattheyfrequentlytargetmultiplecellsignallingpathways,includingthecellcycle,apoptosis,proliferation,survival,invasion,angiogenesis,metastasisandinflammation.
Thustheiruseinchemopreventionhasgainedattention[183,184].
Additionally,sincemostofthecancerdrugsdevelopedhavebeendeliberatelydirectedtowardspecificmoleculartargetsthatareinvolvedinonewayoranotherinenablingpartic‐ularcellularfunctions,inresponsetomonotherapycancercellsmayreducetheirdepend‐NewResearchDirectionsinDNARepair506enceonaparticularproficiency(e.
g.
asinglerepairpathway),becomingmoredependentonanother,thuscontributingtoacquiredrugresistance.
Thus,asanalternativeapproach,se‐lectiveco-targetingofmultiplecoreandemerginghallmarkproficienciesinmechanism-guidedcombinationscouldresultinmoreeffectiveanddurabletherapiesforhumancancer[185].
Phytochemicalscanbehighlypleiotropic,modulatingnumeroustargets,includingtheactivationoftranscriptionfactors,receptors,kinases,cytokines,enzymes,andgrowthfac‐tors[186].
Thereforecurrenteffortsarehighlyengagedindiscoveringnaturalplant-basedchemicalsthatcouldassistinthefightagainstdrugresistance.
ForexamplesoyisoflavonesinhibitedAPE1expressioninprostatecancercellsinatime-anddose-dependentmanner,whereasIRup-regulatedexpressionofthisBERgene,inre‐sponsetoDNAdamage[187-190].
PretreatmentofcancercellswithsoyisoflavonesinhibitedtheincreaseinexpressionofAPE1,andenhancedtheefficacyofchemotherapyandradiationtherapyofmultiplecancersmodelsinvitroandinvivo,possiblythroughdown-regulationofthisDNArepairgene[188].
Anotherphytochemical,resveratrol,wasal‐soshowntoinhibitAPE1endonucleaseactivityandrendermelanomacellsmoresensitivetotreatmentwiththealkylatingagentdacarbazine[191].
Thusbothresveratrolandisofla‐vonessuchasgenisteincanhavetherapeuticpotentialasanAPEinhibitor.
Aseriesofana‐logsofresveratrolhavebeengeneratedinrecentyears,whichexhibitincreasedpotencyand/orarangeofselectiveactivitiescomparedtotheparentalcompoundresveratrol,andpossiblyimprovedpharmacokineticproperties[192].
Aclinicaltrialofresveratrolincoloncancerhasrecentlybeencompleted(http://www.
clinicaltrials.
gov).
ResveratrolcanalsoincreaseBRCA1andBRCA2expression,althoughnoeffectisseenattheproteinlevel[193].
AnincreaseinBRAC1expressioncanleadtoincreasedarrestofcellsintheG2phase,thusmakingthemmuchmoresensitivetoconventionaltherapy.
Onecommonche‐motherapeuticdrugisdoxorubicin,whichpredominantlyinducesDNAdamageinG2phasecells[194].
Resveratrol,curcuminandthenaturallyoccurringflavolignandeoxypodophyllo‐toxin[195]caninduceG2/Mcellcyclearrest,andaltertheexpressionofcellcycleregulatoryproteins,thusallowingdoxorubicintoinducelesionsandasaconsequenceenhancetheapop‐toticeffect[186,196,197].
LeCorreetal.
,alsodemonstratedthatresveratrolhasaneffectontheexpressionofgenesimplicatedintheregulationofBRCA1proteinfunctionsandinmultiplenuclearprocessesmodulatedbyBRCA1inhumanbreastcancerandfibrocysticbreastcells[198].
OneofthemechanismsbywhichresveratrolcanenhanceBRAC1expressionisbyassoci‐ationwithBRCA1,repressingthearomatichydrocarbonreceptor(AhR).
AhRbindsmanynat‐uraldietarybioactivecompoundsthereforecombinationdietswithAhRantagonistsmayoffertheadvantageofhighercancerpreventionefficacies[199].
InHR-deficienttumours,patientswithheterozygousmutationsintheHRgenesBRCA1andBRCA2developbreastandovariantumourswithfunctionallossofHRactivity,anddeficiencyinthispathwaymaydictatethesensitivityoftumourstocertainDNA-damagingagentsandthismaybeanotherpossibleap‐proachtotestnaturalcompoundstoovercomeresistance,andoncemoreenhancecombinato‐rystrategiestooptimizetreatmentoutcome[32].
Recentlyanextractofneemleaveswascharacterizedandasignificantup-regulationofgenesassociatedwithmetabolism,inflammationandangiogenesis,suchasHMOX1andDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952507AKRwasobserved.
Howevergenesassociatedwithcellcycle,DNAreplication,recombina‐tion,andrepairfunctionsweredown-regulated[200].
Onestudyanalysed531compoundsderivedfromplantsandfoundnocorrelationwithgenesinvolvedinNER(ERCC1,XPA,XPC,DDB2,ERCC4,ERCC5)orBER(MPG,APE1,OGG1,XRCC1,LIG3,POLB).
Itispossiblethatnaturalcompoundsmaytargetdifferentmolecularpathwaysfromthoseofstandardanti-tumordrugs,henceifDNArepairisinvolvedinthedevelopmentofresistancetoestab‐lishedanticancerdrugs,naturalcompoundsmaybeattractivesourcesofnoveldrugssuita‐bletotreatdrugresistanttumours,withtheadvantageofhavingreducedsideeffects[201].
Likewise,mostplantderivativescanactasantioxidantsandsomeofthemcanincreasehu‐manMGMTexpression(e.
g.
curcumin,silymarin,sulforaphaneandresveratrol)beyonditssteady-statelevels,havingaroleincancerchemoprevention[202].
Additionally,bothBRCA1andMGMTgenesaresusceptibletohypermethylation,andgreenteapolyphenolsandbioflavonoidshavebeenshowntoreversetheeffectsofDNAhypermethylation[203].
Theseresultssuggestthatsomedietarycompoundsmayhaveapotentialdemethylat‐ingeffect,andcouldbepromisingadjuvantstochemotherapyindrugresistantsettings.
Anotherissueincancerchemotherapyistheuseofmonotherapyvscombinedtherapy,andseveralstudieshavebeenperformedregardingpossiblecombinatorychemotherapywithnat‐uralcompounds(lessaggressivethanthemajorityofchemotherapeuticdrugs),albeitinpre‐clinicalsettings,e.
g.
silibininextract[204],ixabepilone[205]andcurcumin[206].
Someoftheseagentsarebeingevaluatedinclinicaltrials.
Silibininstronglysynergizedthegrowth-inhibito‐ryeffectofdoxorubicininprostatecarcinomacells,whichwasassociatedwithastrongG2-Marrestfollowedbyapoptosis[204].
Ixabepilone,ananalogueofthenaturalproductepothiloneB,isalreadyindicatedforthetreatmentoflocallyadvancedormetastaticbreastcancerintheUS.
InaphaseIIItrialinwomenwithlocallyadvancedormetastaticbreastcancerthatwerepretreatedwith,orresistantto,anthracyclines(e.
g.
doxorubicin)andresistanttotaxanes,pro‐gression-freesurvivalwassignificantlylongerinixabepilonepluscapecitabinerecipientscom‐paredwithrecipientsofcapecitabinemonotherapy[205].
Combinationtherapyusingcurcuminwithgemcitabine-basedchemotherapy,inaphaseI/IIstudy,inpatientswithpancre‐aticcancerwarrantsfurtherinvestigationintoitsefficacy[206].
Finally,aninterestingrecentdevelopmentconcernstheobservationthatmiRscouldberegu‐latedbynaturalagents,leadingtotheinhibitionofcancercellgrowth,epithelialtomesenchy‐maltransition(EMT),drugresistance,andmetastasis[207].
Formostepithelialtumors,progressiontowardmalignancyisaccompaniedbyalossofepithelialdifferentiationandashifttowardmesenchymalphenotype[185].
DuringtheacquisitionofEMTcharacteristics,cancercellslosetheexpressionofproteinsthatpromotecell-cellcontact,suchasE-cadherinandγ-catenin,andgaintheexpressionofmesenchymalmarkers,suchasvimentin,fibronectin,andN-cadherin,leadingtoenhancedcancercellmigrationandinvasion.
Ithasbeenshownthatdown-regulationorthelossintheexpressionofthemiR-200familyisassociatedwithEMT.
Gemcitabine-resistantpancreaticcellshavingEMTcharacteristicsshowedlowexpres‐sionofthemiR-200familyandmiR-200islostininvasivebreastcancercelllineswithmesen‐chymalphenotype.
HencetheinterestingobservationthatisoflavonecouldinducemiR-200expressioningemcitabine-resistantpancreaticcells,resultinginalteredcellularmorphologyNewResearchDirectionsinDNARepair508frommesenchymal-to-epithelialappearanceandinducedE-cadherindistributionthatismoresimilartoepithelial-likecells.
Likewise,let-7hasbeenfoundtoregulatecellproliferationanddifferentiation,andinhibittheexpressionofmultipleoncogenes,includingrasandmyc,andagainitwasobservedthatisoflavonecouldsignificantlyup-regulatetheexpressionoflet-7family,suggestingthatthisphytochemicalcouldreverseEMTcharacteristicsinpartduetotheup-regulationoflet-7[207].
Otherreportshaveshownthatcurcumin,isoflavone,indole-3-car‐binol(I3C),3,3′-diindolylmethane(DIM),()-epigallocatechin-3-gallate(EGCG)orresveratrol,canaltermiRNAexpressionprofiles,leadingtotheinhibitionofcancergrowth,inductionofapoptosis,reversalofEMTphenotype,andincreasingdrugsensitivity[208].
ItremainstobeseenifphytochemicalscanaffectmiRsthatregulateDNArepairpathways,butsinceanygivenmiRcantargetseveraltranscripts,thisregulationishighlylikely.
Over‐all,naturalcompounds,mayhaveanimportantroleinchemopreventionandincombinedtherapy,andmaypreventresistancetochemotherapy[188,189,208-210].
10.
ConclusionandfuturedirectionsAsdiscussedinthischapter,theultimatetargetofchemotherapyandradiotherapyisthecancercell,anduseofDNAdamagingagentsisjustifiablesincemostofthesecellsarehigh‐lycyclingcells.
ThetargetingofDNArepairpathwaysisbutoneofthemanystrategiesde‐velopedinthefightagainstcancer.
CancercellsfrequentlypossessalteredDNArepaircapacities,andthiscanbeputtouseintheclinic.
ThusthequestforspecifictherapiesthattargetDNArepairhasproducedmanypotentiallyusefulagents(Table1).
Usingsuchagentscantheoreticallyincreasetheefficacyofexistingchemotherapyand/orradiotherapy.
Nevertheless,thesamedifficultiesencounteredbyallotheralternativestrategiesarealsoarisingwhenwedisruptDNArepairprocesses.
ThesuccessoftheseagentsultimatelywilldependonourbasicknowledgeofthevariousDNArepairprocessespresentinagivencelltypeortissue.
NotallDNArepairpathwaysarepresentinalltissues,asevidencedbythefactthatmutationsinspecificpathwaysgiverisepreferentiallytocertaintumourtypesandnotothers.
Secondly,thesuccesswillalsode‐pendonthespecificgenomicandgeneticlandscapeofeachtumour,implyingthatdifferentcombinationsofinhibitorsandchemicalagentsshallhavetobetailoredtoeachtumour.
Wearestillfarfromachievingthisgoal,butgreatstrideshavebeentakeninthepastyears.
Thirdly,weshallhavetoredirectthestrategytodiscovera"cureforcancer"andinsteadfollowstrategiesthatallowustoaccompanytheinevitableandinexorableevolutionofthecancercellandconsistentlyfindandimplementmoreandmoretargetedtherapies,evenifthesestrategiesleadustoreturntoabandonedtherapies.
Theresurgenceofdrugholidays,inwhichatherapyisabandonedtemporarilytobetakenupafteracertainperiod,notun‐likewhatcanbeadoptedwithantibiotics,isonesuchstrategy.
Inthiscasetheabsenceofaselectivepressureimposedbyaspecificagentmayleadcancercellstoloseresistancetothisagent,makingthemagainvulnerabletothesameagent.
Thisstrategyhasbeenfollowedincertaincancersandcouldbeadaptedinothers,withtheadvantageofofferingreducedtimeonchemotherapy,reducedcumulativetoxiceffects,andimprovedqualityoflife[211,212].
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952509TargetDrugConditionortumorCombinationtherapyagent(s)Phaseofclinicaltrialplanned,ongoingorrecentlycompleted*ReferenceMGMTO6-BenzylguanineMultipleMyelomaandPlasmaCellNeoplasmGlioblastoma,GliosarcomaMelanomaColorectalCancerCarmustineTemodarCarmustineCarmustinePhaseIIcompletedPhaseIIcompletedPhaseIIcompletedPhaseIIcompletedwww.
cancer.
govPARP1AZD-2281/KU59436(Olaparib)TripleNegativeBreastCancerTripleNegativeMetastaticBreastCancerKnownBRCAOvarianCancerorKnownBRCA/TripleNeg.
BreastCancerCisplatinPaclitaxelPhaseI/IIactivePhaseI/IIcompletedwww.
astrazeneca.
comAG014699/PF-01367338(Rucaparib)SolidtumorsMelanomaTemozolomideVariousagentsPhaseIcompletedPhaseIIongoingwww.
pfizer.
comINO-1001MelanomaTemozolomidePhaseIterminatedwww.
inotekcorp.
comBSI-201/(Iniparib)UterineCarcinosarcomaCarboplatin,Paclitaxel,PhaseIIactivewww.
biparsciences.
comwww.
sanofi.
comBreastCancerGemcitabine/CarboplatinPhaseIIcompletedPhaseIIIactiveABT-888/(Veliparib)BreastcancerCarboplatinTemozolomidePhaseIIactivewww.
abbott.
comProstateCancerTemozolomidePhaseIactiveMelanomaTemozolomidePhaseIIactiveVariouscancersVariousagentsPhaseI/IIactiveMK4827SolidBRCAOvarianSingleagentVariousagentsPhaseIongoingwww.
merck.
comCEP-9722SolidtumoursTMZVariousagentsPhaseIwww.
cephalon.
comwww.
tevapharm.
comGPI1016/E7016SolidtumoursTMZVariousagentsPhaseIwww.
eisai.
comLT673HematologicalcancersSolidtumoursVariousagentsPhaseIongoingwww.
bmrn.
comNMS-P118Preclinical;highlyselectiveagainstPARP-5(tankyrase)www.
nervianoms.
comBERMethoxyamine/TRC-102AdvancedrefractorysolidcancersHematologicalcancersPemetrexedTMZFludarabinePhaseIactivePhaseIongoingwww.
traconpharma.
comATMKinaseKU55933Preclinicalwww.
astrazeneca.
comCHK1AZD7762www.
astrazeneca.
comPF-00477736www.
pfizer.
comXL844www.
exelixis.
comFACurcuminGastrointestinalcancersPhaseIINewResearchDirectionsinDNARepair510TargetDrugConditionortumorCombinationtherapyagent(s)Phaseofclinicaltrialplanned,ongoingorrecentlycompleted*ReferencePathwayc-ABLImatinibVarioussolidtumoursPhaseIIIwww.
novartis.
comEGFRErlotinibNSCLCMonotherapyorcombinationPhaseII/IIIwww.
gene.
comGefinitibwww.
astrazeneca.
com*Asof10September2012,http://clinicaltrials.
govTable1.
Targetedtherapeuticsindevelopment,inclinicaluseorinclinicaltrials*.
ThisleadstothefinalandperhapsmostchallengingprobleminthedevelopmentofagentsthatmodulateDNArepair,whichistoxicitytonormalcells,inparticulartothehematopoieticsystemandthegastrointestinalepithelia.
Variousstrategiesarebeingfol‐lowedtominimizetoxicity,whichincludetheintermittentadministrationduringthera‐py,mentionedabove,alternatingwithothertherapies,usinghighlylocalizedradiotherapytogetherwithinhibitorstominimizecollateraldamage,andusinginhibitorsassingleagents[213,214].
Altogether,thecombineduseofthevariousweaponsatourdisposalinacoordinated,comprehensivefashioncouldeffectivelyleadtoimprovedpa‐tienttreatment.
AcknowledgementsThisworkwassupportedbygrantsPTDC/SAUGMG/71720/2006fromFundaodeCiênciaeTecnologia(FCT),andPEst-OE/SAU/UI0009/2011-12fromFCT.
M.
G.
wassupportedbyCIENCIA2008(FCT).
CIGMHissupportedbyFCT.
B.
G.
(SFRH/BD/64131/2009),P.
G.
(SFRH/BD/70293/2010)andC.
M.
(SFRH/BD/81097/2011)aresupportedbyPh.
D.
grantsfromFCT.
AuthordetailsAntónioS.
Rodrigues1*,BrunoCostaGomes1,CéliaMartins1,MartaGromicho1,NunoG.
Oliveira2,PatríciaS.
Guerreiro2andJoséRueff1*Addressallcorrespondenceto:sebastiao.
rodrigues@fcm.
unl.
pt1CIGMH–DepartmentofGenetics,FacultyofMedicalSciences,UniversidadeNovadeLis‐boa,Lisboa,Portugal2ResearchInstituteforMedicinesandPharmaceuticalSciences(iMed.
UL),UL,FacultyofPharmacy,UniversidadedeLisboa,Lisboa,PortugalDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952511References[1]FriedbergEC.
DNARepairAndMutagenesis:ASMPress;2006.
[2]HoeijmakersJ.
Genomemaintenancemechanismsforpreventingcancer.
Nature.
2001;411:366-74.
[3]HarperJW,ElledgeSJ.
TheDNADamageResponse:TenYearsAfter.
Molecularcell.
2007;28(5):739-45.
[4]LinZ,NeiM,MaH.
TheoriginsandearlyevolutionofDNAmismatchrepairgenes—multiplehorizontalgenetransfersandco-evolution.
NucleicAcidsResearch.
2007;35(22):7591-603.
[5]LehmannA,McGibbonD,StefaniniM.
Xerodermapigmentosum.
OrphanetJournalofRareDiseases.
2011;6(1):70.
[6]ParadisoA,FormentiS.
Hereditarybreastcancer:clinicalfeaturesandriskreductionstrategies.
AnnalsofOncology.
2011;22(suppl1):i31-i6.
[7]HoeijmakersJHJ.
DNADamage,Aging,andCancer.
NewEnglandJournalofMedi‐cine.
2009;361(15):1475-85.
[8]LengauerC,KinzlerKW,VogelsteinB.
Geneticinstabilitiesinhumancancers.
Na‐ture.
1998;396(6712):643-9.
[9]LoebLA.
AMutatorPhenotypeinCancer.
CancerResearch.
2001;61(8):3230-9.
[10]LagerwerfS,VrouweMG,OvermeerRM,FousteriMI,MullendersLHF.
DNAdam‐ageresponseandtranscription.
DNARepair.
2011;10(7):743-50.
[11]RodriguesAS,Dinis,J.
,Gromicho,M.
,Martins,M.
,Laires,A.
andRueff,J.
.
GenomicsandCancerDrugResistance.
CurrentPharmaceuticalBiotechnology.
2012;13(5):651-73.
[12]GilletJ-P,GottesmanMM.
MechanismsofMultidrugResistanceinCancerMulti-DrugResistanceinCancer.
In:ZhouJ,editor.
:HumanaPress;2010.
p.
47-76.
[13]O'ConnorMJ,MartinNMB,SmithGCM.
Targetedcancertherapiesbasedonthein‐hibitionofDNAstrandbreakrepair.
Oncogene.
2007;26(56):7816-24.
[14]Al-EjehF,KumarR,WiegmansA,LakhaniSR,BrownMP,KhannaKK.
HarnessingthecomplexityofDNA-damageresponsepathwaystoimprovecancertreatmentoutcomes.
Oncogene.
2010;29(46):6085-98.
[15]HurleyLH.
DNAanditsassociatedprocessesastargetsforcancertherapy.
NatRevCancer.
2002;2(3):188-200.
[16]KokkinakisDM,AhmedMM,DelgadoR,FruitwalaMM,MohiuddinM,Albores-SaavedraJ.
RoleofO6-Methylguanine-DNAMethyltransferaseintheResistanceofPancreaticTumorstoDNAAlkylatingAgents.
CancerResearch.
1997;57(23):5360-8.
NewResearchDirectionsinDNARepair512[17]SancarA,Lindsey-BoltzLA,nsal-KamazK,LinnS.
MolecularMechanismsofMammalianDNArepairandtheDNADamageCheckpoints.
AnnualReviewofBio‐chemistry.
2004;73(1):39-85.
[18]LiebermanHB.
DNADamageRepairandResponseProteinsasTargetsforCancerTherapy.
CurrentMedicinalChemistry.
2008;15(4):360-7.
[19]JacksonSP,BartekJ.
TheDNA-damageresponseinhumanbiologyanddisease.
Na‐ture.
2009;461(7267):1071-8.
[20]SchofieldM,HsiehP.
DNAmismatchrepair:molecularmechanismsandbiologicalfunction.
AnnuRevMicrobiol.
2003;57:579-608.
[21]PeltomkiP.
RoleofDNAMismatchRepairDefectsinthePathogenesisofHumanCancer.
JournalofClinicalOncology.
2003;21(6):1174-9.
[22]NguewaPA,FuertesMA,ValladaresB,AlonsoC,PérezJM.
Poly(ADP-Ribose)Poly‐merases:Homology,StructuralDomainsandFunctions.
NovelTherapeuticalAppli‐cations.
ProgressinBiophysicsandMolecularBiology.
2005;88(1):143-72.
[23]KassEM,JasinM.
CollaborationandcompetitionbetweenDNAdouble-strandbreakrepairpathways.
FEBSLetters.
2010;584(17):3703-8.
[24]LiSX,SjolundA,HarrisL,SweasyJB.
DNArepairandpersonalizedbreastcancertherapy.
EnvironmentalandMolecularMutagenesis.
2010;51(8-9):897-908.
[25]HelledayT.
Homologousrecombinationincancerdevelopment,treatmentandde‐velopmentofdrugresistance.
Carcinogenesis.
2010;31(6):955-60.
[26]BryantHE,SchultzN,ThomasHD,ParkerKM,FlowerD,LopezE,etal.
SpecifickillingofBRCA2-deficienttumourswithinhibitorsofpoly(ADP-ribose)polymerase.
Nature.
2005;434(7035):913-7.
[27]FarmerH,McCabeN,LordCJ,TuttANJ,JohnsonDA,RichardsonTB,etal.
Target‐ingtheDNArepairdefectinBRCAmutantcellsasatherapeuticstrategy.
Nature.
2005;434(7035):917-21.
[28]ChiarugiA.
AsnapshotofchemoresistancetoPARPinhibitors.
TrendsinPharmaco‐logicalSciences.
2012;33(1):42-8.
[29]DavarD,BeumerJH,HamiehL,TawbiH.
RoleofPARPInhibitorsinCancerBiologyandTherapy.
CurrMedChem.
2012;19(23):3907-21.
Epub2012/07/14.
[30]FongPC,BossDS,YapTA,TuttA,WuP,Mergui-RoelvinkM,etal.
InhibitionofPoly(ADP-Ribose)PolymeraseinTumorsfromBRCAMutationCarriers.
NewEng‐landJournalofMedicine.
2009;361(2):123-34.
[31]KelleyMR,FishelML.
DNArepairproteinsasmoleculartargetsforcancertherapeu‐tics.
Anti-CancerAgentsinMedicinalChemistry.
2008;8(4):417-25.
[32]EversB,HelledayT,JonkersJ.
Targetinghomologousrecombinationrepairdefectsincancer.
TrendsinPharmacologicalSciences.
2010;31(8):372-80.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952513[33]HelledayT,PetermannE,LundinC,HodgsonB,SharmaRA.
DNArepairpathwaysastargetsforcancertherapy.
NatureReviewsCancer.
2008;8(3):193-204.
[34]BouwmanP,JonkersJ.
TheeffectsofderegulatedDNAdamagesignallingoncancerchemotherapyresponseandresistance.
NatRevCancer.
2012;12(9):587-98.
[35]LongleyDB,JohnstonPG.
Molecularmechanismsofdrugresistance.
TheJournalofPathology.
2005;205(2):275-92.
[36]StrattonMR,CampbellPJ,FutrealPA.
Thecancergenome.
Nature.
2009;458(7239):719-24.
[37]DrablsF,FeyziE,AasPA,VaagbCB,KavliB,BratlieMS,etal.
AlkylationdamageinDNAandRNA—repairmechanismsandmedicalsignificance.
DNARepair.
2004;3(11):1389-407.
[38]KainaB,ChristmannM,NaumannS,RoosWP.
MGMT:Keynodeinthebattleagainstgenotoxicity,carcinogenicityandapoptosisinducedbyalkylatingagents.
DNARepair.
2007;6(8):1079-99.
[39]JacintoFV,EstellerM.
MGMThypermethylation:Aprognosticfoe,apredictivefriend.
DNARepair.
2007;6(8):1155-60.
[40]MargisonGP,SantibáezKorefMF,PoveyAC.
Mechanismsofcarcinogenicity/chemotherapybyO6-methylguanine.
Mutagenesis.
2002;17(6):483-7.
[41]ZaidiNH,LiuL,GersonSL.
QuantitativeimmunohistochemicalestimatesofO6-al‐kylguanine-DNAalkyltransferaseexpressioninnormalandmalignanthumancolon.
ClinicalCancerResearch.
1996;2(3):577-84.
[42]LeeSM,RaffertyJA,ElderRH,FanCY,BromleyM,HarrisM,etal.
Immunohistolog‐icalexaminationoftheinter-andintracellulardistributionofO6-alkylguanineDNA-alkyltransferaseinhumanliverandmelanoma.
BrJCancer.
1992;66(2):355-60.
[43]AugustineCK,YooJS,PottiA,YoshimotoY,ZipfelPA,FriedmanHS,etal.
GenomicandMolecularProfilingPredictsResponsetoTemozolomideinMelanoma.
ClinicalCancerResearch.
2009;15(2):502-10.
[44]HegiME,LiuL,HermanJG,StuppR,WickW,WellerM,etal.
CorrelationofO6-MethylguanineMethyltransferase(MGMT)PromoterMethylationWithClinicalOut‐comesinGlioblastomaandClinicalStrategiestoModulateMGMTActivity.
JournalofClinicalOncology.
2008;26(25):4189-99.
[45]HegiME,DiserensA-C,GorliaT,HamouM-F,deTriboletN,WellerM,etal.
MGMTGeneSilencingandBenefitfromTemozolomideinGlioblastoma.
NewEnglandJour‐nalofMedicine.
2005;352(10):997-1003.
[46]HegiME,DiserensA-C,GodardS,DietrichP-Y,RegliL,OstermannS,etal.
ClinicalTrialSubstantiatesthePredictiveValueofO-6-Methylguanine-DNAMethyltransfer‐asePromoterMethylationinGlioblastomaPatientsTreatedwithTemozolomide.
ClinicalCancerResearch.
2004;10(6):1871-4.
NewResearchDirectionsinDNARepair514[47]HegiME,SciuscioD,MuratA,LevivierM,StuppR.
EpigeneticDeregulationofDNARepairandItsPotentialforTherapy.
ClinicalCancerResearch.
2009;15(16):5026-31.
[48]SuzukiT,NakadaM,YoshidaY,NambuE,FuruyamaN,KitaD,etal.
TheCorrela‐tionbetweenPromoterMethylationStatusandtheExpressionLevelofO6-Methyl‐guanine-DNAMethyltransferaseinRecurrentGlioma.
JapaneseJournalofClinicalOncology.
2011;41(2):190-6.
[49]EstellerM,HamiltonSR,BurgerPC,BaylinSB,HermanJG.
InactivationoftheDNArepairgeneO6-methylguanine-DNAmethyltransferasebypromoterhypermethyla‐tionisacommoneventinprimaryhumanneoplasia.
CancerRes.
1999;59(4):793-7.
Epub1999/02/24.
[50]NakadaM,FurutaT,HayashiY,MinamotoT,HamadaJ-i.
Thestrategyforenhanc‐ingtemozolomideagainstmalignantglioma.
FrontiersinOncology.
2012;2.
[51]QuinnJA,DesjardinsA,WeingartJ,BremH,DolanME,DelaneySM,etal.
PhaseITrialofTemozolomidePlusO6-BenzylguanineforPatientsWithRecurrentorPro‐gressiveMalignantGlioma.
JournalofClinicalOncology.
2005;23(28):7178-87.
[52]MakiY,MurakamiJ,AsaumiJ-i,TsujigiwaH,NagatsukaH,KokeguchiS,etal.
RoleofO6-methylguanine–DNAmethyltransferaseandeffectofO6-benzylguanineontheanti-tumoractivityofcis-diaminedichloroplatinum(II)inoralcancercelllines.
Oraloncology.
2005;41(10):984-93.
[53]BattsE,MaiselC,KaneD,LiuL,FuP,O'BrienT,etal.
O6-benzylguanineandBCNUinmultiplemyeloma:aphaseIItrial.
CancerChemotherapyandPharmacology.
2007;60(3):415-21.
[54]RansonM,HerseyP,ThompsonD,BeithJ,McArthurGA,HaydonA,etal.
Random‐izedTrialoftheCombinationofLomeguatribandTemozolomideComparedWithTemozolomideAloneinChemotherapyNaivePatientsWithMetastaticCutaneousMelanoma.
JournalofClinicalOncology.
2007;25(18):2540-5.
[55]KhanOA,RansonM,MichaelM,OlverI,LevittNC,MortimerP,etal.
AphaseIItrialoflomeguatribandtemozolomideinmetastaticcolorectalcancer.
BrJCancer.
2008;98(10):1614-8.
[56]TawbiHA,VillaruzL,TarhiniA,MoschosS,SuleckiM,ViveretteF,etal.
InhibitionofDNArepairwithMGMTpseudosubstrates:phaseIstudyoflomeguatribincom‐binationwithdacarbazineinpatientswithadvancedmelanomaandothersolidtu‐mours.
BrJCancer.
2011;105(6):773-7.
[57]RansonM,MiddletonMR,BridgewaterJ,LeeSM,DawsonM,JowleD,etal.
Lome‐guatrib,apotentinhibitorofO6-alkylguanine-DNA-alkyltransferase:phaseIsafety,pharmacodynamic,andpharmacokinetictrialandevaluationincombinationwithte‐mozolomideinpatientswithadvancedsolidtumors.
ClinCancerRes.
2006;12(5):1577-84.
Epub2006/03/15.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952515[58]CaporasoP,TurrizianiM,VendittiA,MarchesiF,BuccisanoF,TirindelliMC,etal.
Novelroleoftriazenesinhaematologicalmalignancies:PilotstudyofTemozolo‐mide,LomeguatribandIL-2inthechemo-immunotherapyofacuteleukaemia.
DNARepair.
2007;6(8):1179-86.
[59]SabharwalA,CorriePG,MidgleyRS,PalmerC,BradyJ,MortimerP,etal.
AphaseItrialoflomeguatribandirinotecaninmetastaticcolorectalcancer.
CancerChemotherPharmacol.
2010;66(5):829-35.
Epub2009/12/30.
[60]KainaB,MargisonGP,ChristmannM.
TargetingO(6)-methylguanine-DNAmethyl‐transferasewithspecificinhibitorsasastrategyincancertherapy.
CellMolLifeSci.
2010;67(21):3663-81.
Epub2010/08/19.
[61]KochD,HundsbergerT,BoorS,KainaB.
LocalintracerebraladministrationofO6-benzylguaninecombinedwithsystemicchemotherapywithtemozolomideofapa‐tientsufferingfromarecurrentglioblastoma.
JournalofNeuro-Oncology.
2007;82(1):85-9.
[62]JiricnyJ.
Themultifacetedmismatch-repairsystem.
NatRevMolCellBiol.
2006;7:335-46.
[63]LiG.
MechanismsandfunctionsofDNAmismatchrepair.
CellRes.
2008;18:85-98.
[64]AaltonenL,PeltomakiP,LeachF,SistonenP,PylkkanenL,MecklinJ,etal.
Cluestothepathogenesisoffamilialcolorectalcancer.
Science.
1993;260(5109):812-6.
[65]BolandCR,ThibodeauSN,HamiltonSR,SidranskyD,EshlemanJR,BurtRW,etal.
ANationalCancerInstituteWorkshoponMicrosatelliteInstabilityforCancerDetec‐tionandFamilialPredisposition:DevelopmentofInternationalCriteriafortheDeter‐minationofMicrosatelliteInstabilityinColorectalCancer.
CancerResearch.
1998;58(22):5248-57.
[66]AebiS,Kurdi-HaidarB,GordonR,CenniB,ZhengH,FinkD,etal.
LossofDNAMismatchRepairinAcquiredResistancetoCisplatin.
CancerResearch.
1996;56(13):3087-90.
[67]HawnMT,UmarA,CarethersJM,MarraG,KunkelTA,BolandCR,etal.
EvidenceforaConnectionbetweentheMismatchRepairSystemandtheG2CellCycleCheck‐point.
CancerResearch.
1995;55(17):3721-5.
[68]LageH,DietelM.
InvolvementoftheDNAmismatchrepairsysteminantineoplasticdrugresistance.
Journalofcancerresearchandclinicaloncology.
1999;125(3):156-65.
[69]DioufB,ChengQ,KrynetskaiaNF,YangW,CheokM,PeiD,etal.
SomaticdeletionsofgenesregulatingMSH2proteinstabilitycauseDNAmismatchrepairdeficiencyanddrugresistanceinhumanleukemiacells.
NatMed.
2011;17(10):1298-303.
[70]KaplanE,GunduzU.
ExpressionanalysisofTOP2A,MSH2andMLH1genesinMCF7cellsatdifferentlevelsofetoposideresistance.
BiomedPharmacother.
2012;66(1):29-35.
Epub2012/01/31.
NewResearchDirectionsinDNARepair516[71]PoveyAC,BadawiAF,CooperDP,HallCN,HarrisonKL,JacksonPE,etal.
DNAAlkylationandRepairintheLargeBowel:AnimalandHumanStudies.
TheJournalofNutrition.
2002;132(11):3518S-21S.
[72]MaxwellJA,JohnsonSP,McLendonRE,ListerDW,HorneKS,RasheedA,etal.
Mis‐matchRepairDeficiencyDoesNotMediateClinicalResistancetoTemozolomideinMalignantGlioma.
ClinicalCancerResearch.
2008;14(15):4859-68.
[73]ValeriN,GaspariniP,BraconiC,PaoneA,LovatF,FabbriM,etal.
MicroRNA-21inducesresistanceto5-fluorouracilbydown-regulatinghumanDNAMutShomolog2(hMSH2).
ProceedingsoftheNationalAcademyofSciences.
2010;107(49):21098-103.
[74]RobertsonA,KlunglandA,RognesT,LeirosI.
DNARepairinMammalianCells.
CellularandMolecularLifeSciences.
2009;66(6):981-93.
[75]WallaceSS,MurphyDL,SweasyJB.
Baseexcisionrepairandcancer.
CancerLetters.
2012(0).
[76]SrivastavaDK,HusainI,ArteagaCL,WilsonSH.
DNApolymeraseβexpressiondif‐ferencesinselectedhumantumorsandcelllines.
Carcinogenesis.
1999;20(6):1049-54.
[77]TangJ-b,SvilarD,TrivediRN,WangX-h,GoellnerEM,MooreB,etal.
N-methylpur‐ineDNAglycosylaseandDNApolymeraseβmodulateBERinhibitorpotentiationofgliomacellstotemozolomide.
Neuro-Oncology.
2011;13(5):471-86.
[78]DinisJ,SilvaV,GromichoM,MartinsC,LairesA,TavaresP,etal.
DNAdamagere‐sponseinimatinibresistantchronicmyeloidleukemiaK562cells.
LeukLymphoma.
2012;53(10):2004-14.
Epub2012/04/06.
[79]MooreDH,MichaelH,TrittR,ParsonsSH,KelleyMR.
AlterationsintheExpressionoftheDNARepair/RedoxEnzymeAPE/ref-1inEpithelialOvarianCancers.
ClinicalCancerResearch.
2000;6(2):602-9.
[80]KelleyMR,ChengL,FosterR,TrittR,JiangJ,BroshearsJ,etal.
ElevatedandAlteredExpressionoftheMultifunctionalDNABaseExcisionRepairandRedoxEnzymeApe1/ref-1inProstateCancer.
ClinicalCancerResearch.
2001;7(4):824-30.
[81]WangD,LuoM,KelleyMR.
Humanapurinicendonuclease1(APE1)expressionandprognosticsignificanceinosteosarcoma:enhancedsensitivityofosteosarcomatoDNAdamagingagentsusingsilencingRNAAPE1expressioninhibition.
MolCancerTher.
2004;3(6):679-86.
Epub2004/06/24.
[82]RobertsonKA,BullockHA,XuY,TrittR,ZimmermanE,UlbrightTM,etal.
AlteredExpressionofApe1/ref-1inGermCellTumorsandOverexpressioninNT2CellsConfersResistancetoBleomycinandRadiation.
CancerResearch.
2001;61(5):2220-5.
[83]BobolaMS,FinnLS,EllenbogenRG,GeyerJR,BergerMS,BragaJM,etal.
Apurinic/ApyrimidinicEndonucleaseActivityIsAssociatedwithResponsetoRadiationandDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952517ChemotherapyinMedulloblastomaandPrimitiveNeuroectodermalTumors.
Clini‐calCancerResearch.
2005;11(20):7405-14.
[84]SilberJR,BobolaMS,BlankA,SchoelerKD,HaroldsonPD,HuynhMB,etal.
TheApurinic/ApyrimidinicEndonucleaseActivityofApe1/Ref-1ContributestoHumanGliomaCellResistancetoAlkylatingAgentsandIsElevatedbyOxidativeStress.
ClinicalCancerResearch.
2002;8(9):3008-18.
[85]BapatA,FishelML,KelleyMR.
Goingapeasanapproachtocancertherapeutics.
Antioxidants&redoxsignaling.
2009;11(3):651-68.
Epub2008/08/22.
[86]BapatA,GlassLS,LuoM,FishelML,LongEC,GeorgiadisMM,etal.
Novelsmall-moleculeinhibitorofapurinic/apyrimidinicendonuclease1blocksproliferationandreducesviabilityofglioblastomacells.
JPharmacolExpTher.
2010;334(3):988-98.
Epub2010/05/28.
[87]TavernaP,LiuL,HwangHS,HansonAJ,KinsellaTJ,GersonSL.
Methoxyaminepo‐tentiatesDNAsinglestrandbreaksanddoublestrandbreaksinducedbytemozolo‐mideincoloncancercells.
MutatRes.
2001;485(4):269-81.
Epub2001/10/05.
[88]RinneM,CaldwellD,KelleyMR.
TransientadenoviralN-methylpurineDNAglyco‐sylaseoverexpressionimpartschemotherapeuticsensitivitytohumanbreastcancercells.
MolCancerTher.
2004;3(8):955-67.
Epub2004/08/10.
[89]YanL,BulgarA,MiaoY,MahajanV,DonzeJR,GersonSL,etal.
Combinedtreat‐mentwithtemozolomideandmethoxyamine:blockingapurininc/pyrimidinicsitere‐paircoupledwithtargetingtopoisomeraseIIalpha.
ClinCancerRes.
2007;13(5):1532-9.
Epub2007/03/03.
[90]FishelML,HeY,SmithML,KelleyMR.
Manipulationofbaseexcisionrepairtosen‐sitizeovariancancercellstoalkylatingagenttemozolomide.
ClinCancerRes.
2007;13(1):260-7.
Epub2007/01/04.
[91]LiuL,YanL,DonzeJR,GersonSL.
Blockageofabasicsiterepairenhancesantitumorefficacyof1,3-bis-(2-chloroethyl)-1-nitrosoureaincolontumorxenografts.
MolCan‐cerTher.
2003;2(10):1061-6.
Epub2003/10/28.
[92]BulgarAD,WeeksLD,MiaoY,YangS,XuY,GuoC,etal.
Removalofuracilbyura‐cilDNAglycosylaselimitspemetrexedcytotoxicity:overridingthelimitwithme‐thoxyaminetoinhibitbaseexcisionrepair.
CellDeathDis.
2012;3:e252.
Epub2012/01/13.
[93]TavernaP,HwangHS,SchuppJE,RadivoyevitchT,SessionNN,ReddyG,etal.
In‐hibitionofbaseexcisionrepairpotentiatesiododeoxyuridine-inducedcytotoxicityandradiosensitization.
CancerResearch.
2003;63(4):838-46.
[94]YanT,SeoY,SchuppJE,ZengXH,DesaiAB,KinsellaTJ.
Methoxyaminepotentiatesiododeoxyuridine-inducedradiosensitizationbyalteringcellcyclekineticsanden‐hancingsenescence.
MolecularCancerTherapeutics.
2006;5(4):893-902.
NewResearchDirectionsinDNARepair518[95]WeissG,GordonM,RosenL,SavvidesP,AdamsB,AlvarezD,etal.
FinalresultsfromaphaseIstudyoforalTRC102(methoxyamineHCl),aninhibitorofbase-exci‐sionrepair,topotentiatetheactivityofpemetrexedinpatientswithrefractorycan‐cer.
[abstract].
JClinOncol.
2010;28(15s):abstract2576.
[96]SawidesP,XuY,LiuL,BokarJ,SilvermanP,DowlatiA,etal.
Pharmacokineticpro‐fileofthebase-excisionrepairinhibitormethoxyamine-HCl(TRC102;MX)givenasanone-hourintravenousinfusionwithtemozolomide(TMZ)inthefirst-in-humanphaseIclinicaltrial.
[abstract].
JClinOncol2010;28(15s):abstracte13662.
[97]MohammedMZ,VyjayantiVN,LaughtonCA,DekkerLV,FischerPM,WilsonDM,3rd,etal.
DevelopmentandevaluationofhumanAPendonucleaseinhibitorsinmel‐anomaandgliomacelllines.
BrJCancer.
2011;104(4):653-63.
Epub2011/01/27.
[98]ZawahirZ,DayamR,DengJ,PereiraC,NeamatiN.
Pharmacophoreguideddiscov‐eryofsmall-moleculehumanapurinic/apyrimidinicendonuclease1inhibitors.
JMedChem.
2009;52(1):20-32.
Epub2008/12/17.
[99]SimeonovA,KulkarniA,DorjsurenD,JadhavA,ShenM,McNeillDR,etal.
Identifi‐cationandcharacterizationofinhibitorsofhumanapurinic/apyrimidinicendonu‐cleaseAPE1.
PLoSOne.
2009;4(6):e5740.
Epub2009/06/02.
[100]SeipleLA,CardellinaJH,2nd,AkeeR,StiversJT.
Potentinhibitionofhumanapurin‐ic/apyrimidinicendonuclease1byarylstibonicacids.
MolPharmacol.
2008;73(3):669-77.
Epub2007/11/29.
[101]RaiG,VyjayantiVN,DorjsurenD,SimeonovA,JadhavA,WilsonDM,etal.
Synthe‐sis,BiologicalEvaluation,andStructure-ActivityRelationshipsofaNovelClassofApurinic/ApyrimidinicEndonuclease1Inhibitors.
JournalofMedicinalChemistry.
2012;55(7):3101-12.
[102]SrinivasanA,WangL,ClineC,XieZ,SobolRW,XieX,etal.
IdentificationandChar‐acterizationofHumanApurinic/ApyrimidinicEndonuclease-1Inhibitors.
Biochemis‐try.
2012;[Epubaheadofprint].
[103]LuoM,KelleyMR.
Inhibitionofthehumanapurinic/apyrimidinicendonuclease(APE1)repairactivityandsensitizationofbreastcancercellstoDNAalkylatingagentswithlucanthone.
AnticancerRes.
2004;24(4):2127-34.
Epub2004/08/28.
[104]NaiduMD,AgarwalR,PenaLA,CunhaL,MezeiM,ShenM,etal.
Lucanthoneanditsderivativehycanthoneinhibitapurinicendonuclease-1(APE1)bydirectproteinbinding.
PLoSOne.
2011;6(9):e23679.
Epub2011/09/22.
[105]MadhusudanS,SmartF,ShrimptonP,ParsonsJL,GardinerL,HoulbrookS,etal.
IsolationofasmallmoleculeinhibitorofDNAbaseexcisionrepair.
NucleicAcidsRes.
2005;33(15):4711-24.
Epub2005/08/23.
[106]HortonJK,Joyce-GrayDF,PachkowskiBF,SwenbergJA,WilsonSH.
Hypersensitivi‐tyofDNApolymerasebetanullmousefibroblastsreflectsaccumulationofcytotoxicDNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952519repairintermediatesfromsite-specificalkylDNAlesions.
DNARepair.
2003;2(1):27-48.
[107]HuHY,HortonJK,GrykMR,PrasadR,NaronJM,SunDA,etal.
IdentificationofsmallmoleculesyntheticinhibitorsofDNApolymerasebetabyNMRchemicalshiftmapping.
JBiolChem.
2004;279(38):39736-44.
Epub2004/07/20.
[108]BarakatK,GajewskiM,TuszynskiJA.
DNARepairInhibitors:TheNextMajorSteptoImproveCancerTherapy.
CurrTopMedChem.
2012;12(12):1376-90.
[109]JavleM,CurtinNJ.
TheroleofPARPinDNArepairanditstherapeuticexploitation.
BritJCancer.
2011;105(8):1114-22.
[110]PlummerR,JonesC,MiddletonM,WilsonR,EvansJ,OlsenA,etal.
PhaseIStudyofthePoly(ADP-Ribose)PolymeraseInhibitor,AG014699,inCombinationwithTemo‐zolomideinPatientswithAdvancedSolidTumors.
ClinCancerRes.
2008;14(23):7917-23.
[111]UnderhillC,ToulmondeM,BonnefoiH.
AreviewofPARPinhibitors:frombenchtobedside.
AnnalsofOncology.
2011;22(2):268-79.
[112]AshworthA.
ASyntheticLethalTherapeuticApproach:Poly(ADP)RibosePolymer‐aseInhibitorsfortheTreatmentofCancersDeficientinDNADouble-StrandBreakRepair.
JournalofClinicalOncology.
2008;26(22):3785-90.
[113]deBonoJS,AshworthA.
Translatingcancerresearchintotargetedtherapeutics.
Na‐ture.
2010;467(7315):543-9.
[114]RouleauM,PatelA,HendzelMJ,KaufmannSH,PoirierGG.
PARPinhibition:PARP1andbeyond.
NatRevCancer.
2010;10(4):293-301.
[115]CalvertH,AzzaritiA.
Theclinicaldevelopmentofinhibitorsofpoly(ADP-ribose)polymerase.
AnnalsofOncology.
2011;22(suppl1):i53-i9.
[116]YapTA,SandhuSK,CardenCP,deBonoJS.
Poly(ADP-Ribose)polymerase(PARP)inhibitors:Exploitingasyntheticlethalstrategyintheclinic.
CA:ACancerJournalforClinicians.
2011;61(1):31-49.
[117]KummarS,ChenA,ParchmentR,KindersR,JiJ,TomaszewskiJ,etal.
AdvancesinusingPARPinhibitorstotreatcancer.
BMCmedicine.
2012;10(1):25.
[118]BryantHE,HelledayT.
Inhibitionofpoly(ADP-ribose)polymeraseactivatesATMwhichisrequiredforsubsequenthomologousrecombinationrepair.
NucleicAcidsRes.
2006;34(6):1685-91.
Epub2006/03/25.
[119]Mendes-PereiraAM,MartinSA,BroughR,McCarthyA,TaylorJR,KimJS,etal.
SyntheticlethaltargetingofPTENmutantcellswithPARPinhibitors.
EMBOMolMed.
2009;1(6-7):315-22.
Epub2010/01/06.
NewResearchDirectionsinDNARepair520[120]LeungM,RosenD,FieldsS,CesanoA,BudmanDR.
Poly(ADP-ribose)polymerase-1inhibition:preclinicalandclinicaldevelopmentofsyntheticlethality.
MolMed.
2011;17(7-8):854-62.
Epub2011/03/23.
[121]TuttA,RobsonM,GarberJE,DomchekSM,AudehMW,WeitzelJN,etal.
Oralpoly(ADP-ribose)polymeraseinhibitorolaparibinpatientswithBRCA1orBRCA2mutationsandadvancedbreastcancer:aproof-of-concepttrial.
Lancet.
2010;376(9737):235-44.
Epub2010/07/09.
[122]SultanaR,McNeillDR,AbbottsR,MohammedMZ,ZdzienickaMZ,QutobH,etal.
SyntheticlethaltargetingofDNAdouble-strandbreakrepairdeficientcellsbyhu‐manapurinic/apyrimidinicendonucleaseinhibitors.
IntJCancer.
2012.
Epub2012/03/02.
[123]GuhaM.
PARPinhibitorsstumbleinbreastcancer.
NatBiotechnol.
2011;29(5):373-4.
[124]DentR,LindemanG,ClemonsM,WildiersH,ChanA,McCarthyN,etal.
SafetyandefficacyoftheoralPARPinhibitorolaparib(AZD2281)incombinationwithpaclitax‐elforthefirst-orsecond-linetreatmentofpatientswithmetastatictriple-negativebreastcancer:ResultsfromthesafetycohortofaphaseI/IImulticentertrial[ab‐stract].
JClinOncol2010;28(15s):abstr1018.
[125]GelmonKA,TischkowitzM,MackayH,SwenertonK,RobidouxA,TonkinK,etal.
Olaparibinpatientswithrecurrenthigh-gradeserousorpoorlydifferentiatedovari‐ancarcinomaortriple-negativebreastcancer:aphase2,multicentre,open-label,non-randomisedstudy.
TheLancetOncology.
2011;12(9):852-61.
[126]WoodRD,MitchellM,LindahlT.
HumanDNArepairgenes,2005.
MutationRe‐search/FundamentalandMolecularMechanismsofMutagenesis.
2005;577(1–2):275-83.
[127]RabikCA,DolanME.
Molecularmechanismsofresistanceandtoxicityassociatedwithplatinatingagents.
CancerTreatmentReviews.
2007;33(1):9-23.
[128]KellandL.
Theresurgenceofplatinum-basedcancerchemotherapy.
NatRevCancer.
2007;7(8):573-84.
[129]KberleB,GrimaldiKA,SuntersA,HartleyJA,KellandLR,MastersJRW.
DNARe‐paircapacityandcisplatinsensitivityofhumantestistumourcells.
InternationalJournalofCancer.
1997;70(5):551-5.
[130]MastersJRW,KoberleB.
Curingmetastaticcancer:lessonsfromtesticulargerm-celltumours.
NatRevCancer.
2003;3(7):517-25.
[131]DabholkarM,Bostick-BrutonF,WeberC,BohrVA,EgwuaguC,ReedE.
ERCC1andERCC2ExpressioninMalignantTissuesFromOvarianCancerPatients.
JournaloftheNationalCancerInstitute.
1992;84(19):1512-7.
[132]ReedE.
ERCC1andClinicalResistancetoPlatinum-BasedTherapy.
ClinicalCancerResearch.
2005;11(17):6100-2.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952521[133]ShirotaY,StoehlmacherJ,BrabenderJ,XiongY-P,UetakeH,DanenbergKD,etal.
ERCC1andThymidylateSynthasemRNALevelsPredictSurvivalforColorectalCancerPatientsReceivingCombinationOxaliplatinandFluorouracilChemotherapy.
JournalofClinicalOncology.
2001;19(23):4298-304.
[134]OlaussenKA,DunantA,FouretP,BrambillaE,AndréF,HaddadV,etal.
DNARe‐pairbyERCC1inNon–Small-CellLungCancerandCisplatin-BasedAdjuvantChe‐motherapy.
NewEnglandJournalofMedicine.
2006;355(10):983-91.
[135]LordRVN,BrabenderJ,GandaraD,AlberolaV,CampsC,DomineM,etal.
LowERCC1ExpressionCorrelateswithProlongedSurvivalafterCisplatinplusGemcita‐bineChemotherapyinNon-SmallCellLungCancer.
ClinicalCancerResearch.
2002;8(7):2286-91.
[136]WeberpalsJ,GarbuioK,O'BrienA,Clark-KnowlesK,DoucetteS,AntonioukO,etal.
TheDNArepairproteinsBRCA1andERCC1aspredictivemarkersinsporadicovar‐iancancer.
InternationalJournalofCancer.
2009;124(4):806-15.
[137]JiangJ,LiangX,ZhouX,HuangR,ChuZ,ZhanQ.
ERCC1expressionasaprognos‐ticandpredictivefactorinpatientswithnon-smallcelllungcancer:ameta-analysis.
MolecularBiologyReports.
2012;39(6):6933-42.
[138]LiJ,ZhangJ,LiuY,YeG.
IncreasedexpressionofDNArepairgeneXPFenhancesresistancetohydroxycamptothecininbladdercancer.
Medicalsciencemonitor:in‐ternationalmedicaljournalofexperimentalandclinicalresearch.
2012;18(4):BR156-62.
Epub2012/03/31.
[139]PrewettM,DeeviDS,BassiR,FanF,EllisLM,HicklinDJ,etal.
TumorsEstablishedwithCellLinesSelectedforOxaliplatinResistanceRespondtoOxaliplatinifCom‐binedwithCetuximab.
ClinicalCancerResearch.
2007;13(24):7432-40.
[140]Balin-GauthierD,DelordJP,PillaireMJ,RochaixP,HoffmanJS,BugatR,etal.
Ce‐tuximabpotentiatesoxaliplatincytotoxiceffectthroughadefectinNERandDNAreplicationinitiation.
BrJCancer.
2008;98(1):120-8.
[141]RogakouEP,PilchDR,OrrAH,IvanovaVS,BonnerWM.
DNADouble-strandedBreaksInduceHistoneH2AXPhosphorylationonSerine139.
JournalofBiologicalChemistry.
1998;273(10):5858-68.
[142]PaullTT,RogakouEP,YamazakiV,KirchgessnerCU,GellertM,BonnerWM.
Acrit‐icalroleforhistoneH2AXinrecruitmentofrepairfactorstonuclearfociafterDNAdamage.
Currentbiology:CB.
2000;10(15):886-95.
[143]EstellerM,SilvaJM,DominguezG,BonillaF,Matias-GuiuX,LermaE,etal.
Promot‐erHypermethylationandBRCA1InactivationinSporadicBreastandOvarianTu‐mors.
JournaloftheNationalCancerInstitute.
2000;92(7):564-9.
[144]GraeserM,McCarthyA,LordCJ,SavageK,HillsM,SalterJ,etal.
AMarkerofHo‐mologousRecombinationPredictsPathologicCompleteResponsetoNeoadjuvantNewResearchDirectionsinDNARepair522ChemotherapyinPrimaryBreastCancer.
ClinicalCancerResearch.
2010;16(24):6159-68.
[145]WangW.
EmergenceofaDNA-damageresponsenetworkconsistingofFanconianaemiaandBRCAproteins.
NatRevGenet.
2007;8(10):735-48.
[146]TaronM,RosellR,FelipE,MendezP,SouglakosJ,RoncoMS,etal.
BRCA1mRNAexpressionlevelsasanindicatorofchemoresistanceinlungcancer.
HumanMolecu‐larGenetics.
2004;13(20):2443-9.
[147]QuinnJE,CarserJE,JamesCR,KennedyRD,HarkinDP.
BRCA1andimplicationsforresponsetochemotherapyinovariancancer.
GynecologicOncology.
2009;113(1):134-42.
[148]QuinnJE,KennedyRD,MullanPB,GilmorePM,CartyM,JohnstonPG,etal.
BRCA1FunctionsasaDifferentialModulatorofChemotherapy-inducedApoptosis.
CancerResearch.
2003;63(19):6221-8.
[149]HusainA,HeG,VenkatramanES,SpriggsDR.
BRCA1Up-RegulationIsAssociatedwithRepair-mediatedResistancetocis-Diamminedichloroplatinum(II).
CancerRe‐search.
1998;58(6):1120-3.
[150]KennedyRD,QuinnJE,MullanPB,JohnstonPG,HarkinDP.
TheRoleofBRCA1intheCellularResponsetoChemotherapy.
JournaloftheNationalCancerInstitute.
2004;96(22):1659-68.
[151]MargeliM,CirauquiB,CastellaE,TapiaG,CostaC,Gimenez-CapitanA,etal.
ThePrognosticValueofBRCA1mRNAExpressionLevelsFollowingNeoadjuvantChe‐motherapyinBreastCancer.
PLoSONE.
2010;5(3):e9499.
[152]HennessyBTJ,TimmsKM,CareyMS,GutinA,MeyerLA,FlakeDD,etal.
SomaticMutationsinBRCA1andBRCA2CouldExpandtheNumberofPatientsThatBenefitFromPoly(ADPRibose)PolymeraseInhibitorsinOvarianCancer.
JournalofClini‐calOncology.
2010;28(22):3570-6.
[153]WestonVJ,OldreiveCE,SkowronskaA,OscierDG,PrattG,DyerMJS,etal.
ThePARPinhibitorolaparibinducessignificantkillingofATM-deficientlymphoidtu‐morcellsinvitroandinvivo.
Blood.
2010;116(22):4578-87.
[154]OffitK,LevranO,MullaneyB,MahK,NafaK,BatishSD,etal.
SharedGeneticSus‐ceptibilitytoBreastCancer,BrainTumors,andFanconiAnemia.
JournaloftheNa‐tionalCancerInstitute.
2003;95(20):1548-51.
[155]PanasciL,PaiementJ-P,ChristodoulopoulosG,BelenkovA,MalapetsaA,AloyzR.
ChlorambucilDrugResistanceinChronicLymphocyticLeukemia.
ClinicalCancerResearch.
2001;7(3):454-61.
[156]KleinHL.
TheconsequencesofRad51overexpressionfornormalandtumorcells.
DNARepair.
2008;7(5):686-93.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952523[157]TobinLA,RobertC,RapoportAP,GojoI,BaerMR,TomkinsonAE,etal.
TargetingabnormalDNAdouble-strandbreakrepairintyrosinekinaseinhibitor-resistantchronicmyeloidleukemias.
Oncogene.
2012.
Epub2012/05/30.
[158]TobinLA,RobertC,NagariaP,ChumsriS,TwaddellW,IoffeOB,etal.
TargetingabnormalDNArepairintherapy-resistantbreastcancers.
Molecularcancerresearch:MCR.
2012;10(1):96-107.
Epub2011/11/25.
[159]HicksonI,ZhaoY,RichardsonCJ,GreenSJ,MartinNMB,OrrAI,etal.
IdentificationandCharacterizationofaNovelandSpecificInhibitoroftheAtaxia-TelangiectasiaMutatedKinaseATM.
CancerResearch.
2004;64(24):9152-9.
[160]CowellIG,DurkaczBW,TilbyMJ.
SensitizationofbreastcarcinomacellstoionizingradiationbysmallmoleculeinhibitorsofDNA-dependentproteinkinaseandataxiatelangiectsiamutated.
BiochemicalPharmacology.
2005;71(1–2):13-20.
[161]GoldingSE,RosenbergE,ValerieN,HussainiI,FrigerioM,CockcroftXF,etal.
Im‐provedATMkinaseinhibitorKU-60019radiosensitizesgliomacells,compromisesin‐sulin,AKTandERKprosurvivalsignaling,andinhibitsmigrationandinvasion.
MolecularCancerTherapeutics.
2009;8(10):2894-902.
[162]ShinoharaET,GengL,TanJ,ChenH,ShirY,EdwardsE,etal.
DNA-DependentPro‐teinKinaseIsaMolecularTargetfortheDevelopmentofNoncytotoxicRadiation–SensitizingDrugs.
CancerResearch.
2005;65(12):4987-92.
[163]LeahyJJJ,GoldingBT,GriffinRJ,HardcastleIR,RichardsonC,RigoreauL,etal.
IdentificationofahighlypotentandselectiveDNA-dependentproteinkinase(DNA-PK)inhibitor(NU7441)byscreeningofchromenonelibraries.
Bioorganic&Me‐dicinalChemistryLetters.
2004;14(24):6083-7.
[164]CollisSJ,DeWeeseTL,JeggoPA,ParkerAR.
ThelifeanddeathofDNA-PK.
Onco‐gene.
2004;24(6):949-61.
[165]HardcastleIR,CockcroftX,CurtinNJ,El-MurrMD,LeahyJJJ,StockleyM,etal.
Dis‐coveryofPotentChromen-4-oneInhibitorsoftheDNA-DependentProteinKinase(DNA-PK)UsingaSmall-MoleculeLibraryApproach.
JournalofMedicinalChemis‐try.
2005;48(24):7829-46.
[166]ZabludoffSD,DengC,GrondineMR,SheehyAM,AshwellS,CalebBL,etal.
AZD7762,anovelcheckpointkinaseinhibitor,drivescheckpointabrogationandpo‐tentiatesDNA-targetedtherapies.
MolecularCancerTherapeutics.
2008;7(9):2955-66.
[167]IorioMV,CroceCM.
MicroRNAdysregulationincancer:diagnostics,monitoringandtherapeutics.
Acomprehensivereview.
EMBOMolecularMedicine.
2012;4(3):143-59.
[168]BartelD.
MicroRNAs:genomics,biogenesis,mechanism,andfunction.
Cell.
2004;116(2):281-97.
NewResearchDirectionsinDNARepair524[169]BartelD.
MicroRNAs:targetrecognitionandregulatoryfunctions.
Cell.
2009;136:215-33.
[170]GarzonR,CalinGA,CroceCM.
MicroRNAsinCancer.
AnnualReviewofMedicine.
2009;60(1):167-79.
[171]DiLevaG,BriskinD,CroceCM.
MicroRNAincancer:Newhopesforantineoplasticchemotherapy.
UpsalaJournalofMedicalSciences.
2012;117(2):202-16.
[172]TianW,ChenJ,HeH,DengY.
MicroRNAsanddrugresistanceofbreastcancer:ba‐sicevidenceandclinicalapplications.
ClinicalandTranslationalOncology.
2012:1-8.
[173]KutanziKR,YurchenkoOV,BelandFA,CheckhunVF,PogribnyIP.
MicroRNA-mediateddrugresistanceinbreastcancer.
ClinEpigenetics.
2011;2(2):171-85.
Epub2011/09/29.
[174]HuH,GattiRA.
MicroRNAs:newplayersintheDNAdamageresponse.
JournalofMolecularCellBiology.
2010.
[175]WoutersMD,vanGentDC,HoeijmakersJHJ,PothofJ.
MicroRNAs,theDNAdam‐ageresponseandcancer.
MutationResearch/FundamentalandMolecularMecha‐nismsofMutagenesis.
2011;717(1–2):54-66.
[176]YuY,WangY,RenX,TsuyadaA,LiA,LiuLJ,etal.
Context-DependentBidirection‐alRegulationoftheMutSHomolog2byTransformingGrowthFactorβContributestoChemoresistanceinBreastCancerCells.
MolecularCancerResearch.
2010;8(12):1633-42.
[177]MoskwaP,BuffaFM,PanY,PanchakshariR,GottipatiP,MuschelRJ,etal.
miR-182-MediatedDownregulationofBRCA1ImpactsDNARepairandSensitivitytoPARPInhibitors.
Molecularcell.
2011;41(2):210-20.
[178]SadonesJ,MichotteA,VeldP,ChaskisC,SciotR,MentenJ,etal.
MGMTpromoterhypermethylationcorrelateswithasurvivalbenefitfromtemozolomideinpatientswithrecurrentanaplasticastrocytomabutnotglioblastoma.
EuropeanJournalofCancer.
2009;45(1):146-53.
[179]StuppR,HegiME,MasonWP,vandenBentMJ,TaphoornMJB,JanzerRC,etal.
Ef‐fectsofradiotherapywithconcomitantandadjuvanttemozolomideversusradio‐therapyaloneonsurvivalinglioblastomainarandomisedphaseIIIstudy:5-yearanalysisoftheEORTC-NCICtrial.
TheLancetOncology.
2009;10(5):459-66.
[180]SlabyO,LakomyR,FadrusP,HrstkaR,KrenL,LzicarovaE,etal.
MicroRNA-181familypredictsresponsetoconcomitantchemoradiotherapywithtemozolomideinglioblastomapatients.
Neoplasma.
2010;57(3):264-9.
Epub2010/04/01.
[181]ZhangW,ZhangJ,HoadleyK,KushwahaD,RamakrishnanV,LiS,etal.
miR-181d:apredictiveglioblastomabiomarkerthatdownregulatesMGMTexpression.
Neuro-Oncology.
2012;14(6):712-9.
DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952525[182]LakomyR,SanaJ,HankeovaS,FadrusP,KrenL,LzicarovaE,etal.
MiR-195,miR-196b,miR-181c,miR-21expressionlevelsandO-6-methylguanine-DNAmethyl‐transferasemethylationstatusareassociatedwithclinicaloutcomeinglioblastomapatients.
CancerScience.
2011;102(12):2186-90.
[183]SurhY-J.
Cancerchemopreventionwithdietaryphytochemicals.
NatRevCancer.
2003;3(10):768-80.
[184]KhanN,AfaqF,MukhtarH.
Apoptosisbydietaryfactors:thesuicidesolutionfordelayingcancergrowth.
Carcinogenesis.
2006;28(2):233-9.
[185]HanahanD,WeinbergRobertA.
HallmarksofCancer:TheNextGeneration.
Cell.
2011;144(5):646-74.
[186]AnandP,SundaramC,JhuraniS,KunnumakkaraAB,AggarwalBB.
Curcuminandcancer:An"old-age"diseasewithan"age-old"solution.
CancerLetters.
2008;267(1):133-64.
[187]RaffoulJJ,BanerjeeS,CheM,KnollZE,DoergeDR,AbramsJ,etal.
Soyisoflavonesenhanceradiotherapyinametastaticprostatecancermodel.
IntJCancer.
2007;120(11):2491-8.
Epub2007/02/17.
[188]RaffoulJJ,BanerjeeS,Singh-GuptaV,KnollZE,FiteA,ZhangH,etal.
Down-regula‐tionofApurinic/ApyrimidinicEndonuclease1/RedoxFactor-1ExpressionbySoyIsoflavonesEnhancesProstateCancerRadiotherapyInvitroandInvivo.
CancerRe‐search.
2007;67(5):2141-9.
[189]RaffoulJJ,HeydariAR,HillmanGG.
DNARepairandCancerTherapy:TargetingAPE1/Ref-1UsingDietaryAgents.
Journalofoncology.
2012;2012:11.
[190]RaffoulJJ,SarkarFH,HillmanGG.
Radiosensitizationofprostatecancerbysoyiso‐flavones.
CurrCancerDrugTargets.
2007;7(8):759-65.
Epub2008/01/29.
[191]YangS,IraniK,HeffronSE,JurnakF,MeyskensFL.
Alterationsintheexpressionoftheapurinic/apyrimidinicendonuclease-1/redoxfactor-1(APE/Ref-1)inhumanmel‐anomaandidentificationofthetherapeuticpotentialofresveratrolasanAPE/Ref-1inhibitor.
MolecularCancerTherapeutics.
2005;4(12):1923-35.
[192]FuldaS.
Resveratrolandderivativesforthepreventionandtreatmentofcancer.
DrugDiscoveryToday.
2010;15(17–18):757-65.
[193]FustierP,LeCorreL,ChalabiN,Vissac-SabatierC,CommunalY,BignonYJ,etal.
ResveratrolincreasesBRCA1andBRCA2mRNAexpressioninbreasttumourcelllines.
BrJCancer.
2003;89(1):168-72.
[194]PotterAJ,GollahonKA,PalancaBJA,HarbertMJ,ChoiYM,MoskovitzAH,etal.
FlowcytometricanalysisofthecellcyclephasespecificityofDNAdamageinducedbyradiation,hydrogenperoxideanddoxorubicin.
Carcinogenesis.
2002;23(3):389-401.
NewResearchDirectionsinDNARepair526[195]ShinSY,YongY,KimCG,LeeYH,LimY.
DeoxypodophyllotoxininducesG2/McellcyclearrestandapoptosisinHeLacells.
CancerLetters.
2010;287(2):231-9.
[196]ParkC,KimGY,KimGD,ChoiBT,ParkYM,ChoiYH.
InductionofG2/Marrestandinhibitionofcyclooxygenase-2activitybycurcumininhumanbladdercancerT24cells.
OncolRep.
2006;15(5):1225-31.
Epub2006/04/06.
[197]SaG,DasT.
Anticancereffectsofcurcumin:cycleoflifeanddeath.
CellDivision.
2008;3(1):14.
[198]LeCorreL,FustierP,ChalabiN,BignonY-J,Bernard-GallonD.
EffectsofresveratrolontheexpressionofapanelofgenesinteractingwiththeBRCA1oncosuppressorinhumanbreastcelllines.
ClinicaChimicaActa.
2004;344(1–2):115-21.
[199]PapoutsisAJ,LamoreSD,WondrakGT,SelminOI,RomagnoloDF.
ResveratrolPre‐ventsEpigeneticSilencingofBRCA-1bytheAromaticHydrocarbonReceptorinHu‐manBreastCancerCells.
TheJournalofNutrition.
2010;140(9):1607-14.
[200]MahapatraS,KarnesR,HolmesM,YoungC,ChevilleJ,KohliM,etal.
NovelMolec‐ularTargetsof<i>AzadirachtaindicaAssociatedwithInhibitionofTumorGrowthinProstateCancer.
TheAAPSJournal.
2011;13(3):365-77.
[201]KonkimallaVSB,WangG,KainaB,EfferthT.
Microarray-basedExpressionofDNARepairGenesDoesnotCorrelatewithGrowthInhibitionofCancerCellsbyNaturalProductsDerivedfromTraditionalChineseMedicine.
CancerGenomics-Proteo‐mics.
2008;5(2):79-83.
[202]NitureSK,VeluCS,SmithQR,BhatGJ,SrivenugopalKS.
IncreasedexpressionoftheMGMTrepairproteinmediatedbycysteineprodrugsandchemopreventativenatu‐ralproductsinhumanlymphocytesandtumorcelllines.
Carcinogenesis.
2006;28(2):378-89.
[203]AggarwalBB,ShishodiaS.
Moleculartargetsofdietaryagentsforpreventionandtherapyofcancer.
BiochemicalPharmacology.
2006;71(10):1397-421.
[204]TyagiAK,SinghRP,AgarwalC,ChanDCF,AgarwalR.
SilibininStronglySynergiz‐esHumanProstateCarcinomaDU145CellstoDoxorubicin-inducedGrowthInhibi‐tion,G2-MArrest,andApoptosis.
ClinicalCancerResearch.
2002;8(11):3512-9.
[205]MoenMD.
Ixabepilone:InLocallyAdvancedorMetastaticBreastCancer.
Drugs.
2009;69(11):1471-8110.
2165/00003495-200969110-00006.
[206]KanaiM,YoshimuraK,AsadaM,ImaizumiA,SuzukiC,MatsumotoS,etal.
AphaseI/IIstudyofgemcitabine-basedchemotherapypluscurcuminforpatientswithgemcitabine-resistantpancreaticcancer.
CancerChemotherapyandPharmacology.
2011;68(1):157-64.
[207]LiY,VandenBoomTG,KongD,WangZ,AliS,PhilipPA,etal.
Up-regulationofmiR-200andlet-7byNaturalAgentsLeadstotheReversalofEpithelial-to-Mesen‐DNARepairandResistancetoCancerTherapyhttp://dx.
doi.
org/10.
5772/53952527chymalTransitioninGemcitabine-ResistantPancreaticCancerCells.
CancerRe‐search.
2009;69(16):6704-12.
[208]LiY,KongD,WangZ,SarkarF.
RegulationofmicroRNAsbyNaturalAgents:AnEmergingFieldinChemopreventionandChemotherapyResearch.
Pharmaceuticalresearch.
2010;27(6):1027-41.
[209]SarkarFH,LiY.
Harnessingthefruitsofnatureforthedevelopmentofmulti-target‐edcancertherapeutics.
CancerTreatmentReviews.
2009;35(7):597-607.
[210]SarkarFH,LiY,WangZ,KongD,AliS.
ImplicationofmicroRNAsindrugresist‐ancefordesigningnovelcancertherapy.
Drugresistanceupdates:reviewsandcom‐mentariesinantimicrobialandanticancerchemotherapy.
2010;13(3):57-66.
[211]AdamsRA,MeadeAM,SeymourMT,WilsonRH,MadiA,FisherD,etal.
Intermit‐tentversuscontinuousoxaliplatinandfluoropyrimidinecombinationchemotherapyforfirst-linetreatmentofadvancedcolorectalcancer:resultsoftherandomisedphase3MRCCOINtrial.
TheLancetOncology.
2011;12(7):642-53.
[212]BeckerA,CrombagL,HeidemanDAM,ThunnissenFB,vanWijkAW,PostmusPE,etal.
Retreatmentwitherlotinib:RegainofTKIsensitivityfollowingadrugholidayforpatientswithNSCLCwhoinitiallyrespondedtoEGFR-TKItreatment.
Europeanjournalofcancer(Oxford,England:1990).
2011;47(17):2603-6.
[213]KelleyMR.
Chapter14-FutureDirectionswithDNARepairInhibitors:ARoadmapforDisruptiveApproachestoCancerTherapy.
In:MarkRK,editor.
DNARepairinCancerTherapy.
SanDiego:AcademicPress;2012.
p.
301-10.
[214]KelleyMR.
DNArepairinhibitors:wheredowegofromhereDNARepair(Amst).
2011;10(11):1183-5.
Epub2011/10/04.
NewResearchDirectionsinDNARepair528
- opening科比凯拉相关文档
- Elmadawy科比凯拉
- Diala科比凯拉
- 2017年浙江省"亩产效益"综合评价第一档企业名单
- 军控与安全新闻汇集2014第53周-2015第1周(2014/12/28-2015/1/3)
- "港口代码表-对原报检代码",,,
- 英国科比凯拉
BuyVM迈阿密KVM上线,AMD Ryzen 3900X+NVMe硬盘$2/月起
BuyVM在昨天宣布上线了第四个数据中心产品:迈阿密,基于KVM架构的VPS主机,采用AMD Ryzen 3900X CPU,DDR4内存,NVMe硬盘,1Gbps带宽,不限制流量方式,最低$2/月起,支持Linux或者Windows操作系统。这是一家成立于2010年的国外主机商,提供基于KVM架构的VPS产品,数据中心除了新上的迈阿密外还包括美国拉斯维加斯、新泽西和卢森堡等,主机均为1Gbps带...
宝塔面板企业版和专业版618年中活动 永久授权仅1888元+
我们一般的站长或者企业服务器配置WEB环境会用到免费版本的宝塔面板。但是如果我们需要较多的付费插件扩展,或者是有需要企业功能应用的,短期来说我们可能选择按件按月付费的比较好,但是如果我们长期使用的话,有些网友认为选择宝塔面板企业版或者专业版是比较划算的。这样在年中大促618的时候,我们也可以看到宝塔面板也有发布促销活动。企业版年付899元,专业版永久授权1888元起步。对于有需要的网友来说,还是值...

A2Hosting三年付$1.99/月,庆祝18周年/WordPress共享主机最高优惠81%/100GB SSD空间/无限流量
A2Hosting主机,A2Hosting怎么样?A2Hosting是UK2集团下属公司,成立于2003年的老牌国外主机商,产品包括虚拟主机、VPS和独立服务器等,数据中心提供包括美国、新加坡softlayer和荷兰三个地区机房。A2Hosting在国外是一家非常大非常有名气的终合型主机商,拥有几百万的客户,非常值得信赖,国外主机论坛对它家的虚拟主机评价非常不错,当前,A2Hosting主机庆祝1...
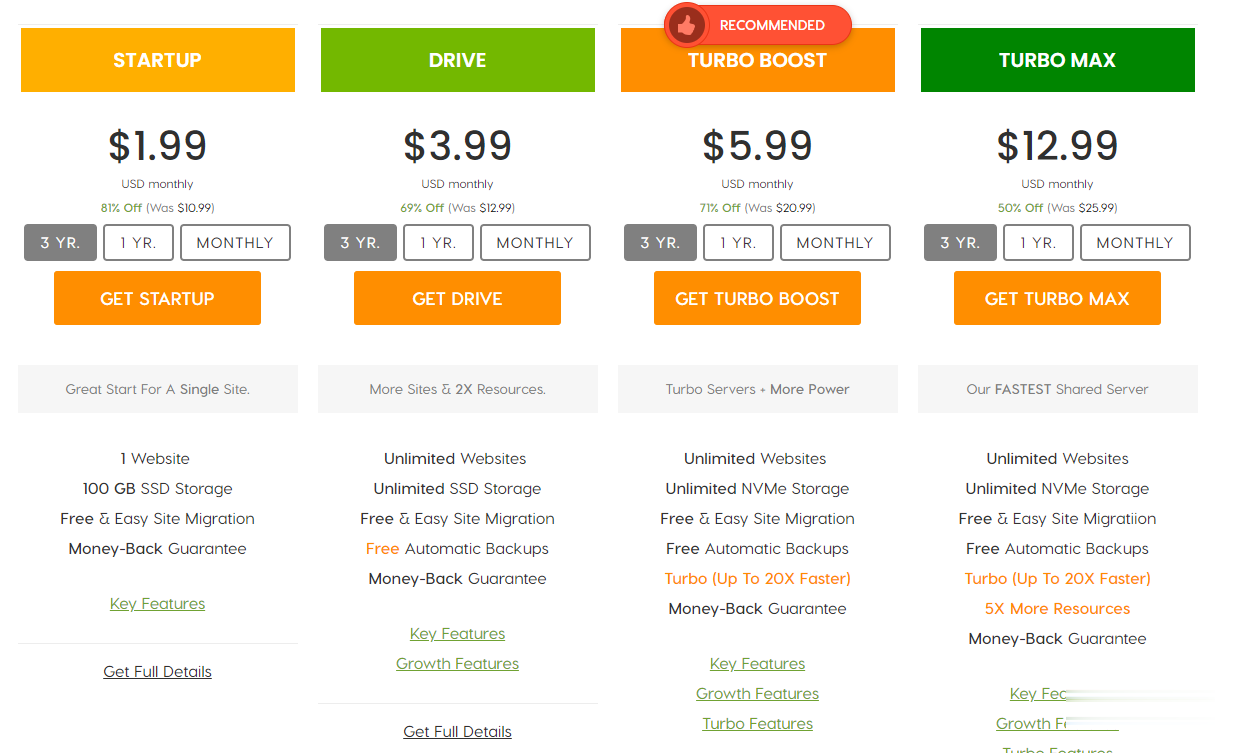
科比凯拉为你推荐
-
急救知识纳入考试急救证容易拿到么?蓝色骨头手机宠物的一个蓝色骨头代表多少级,灰色又代表多少级,另外假如有骨头又代表多少级广东GDP破10万亿中国GDP10万亿,广东3万亿多。占了中国三分之一的经纪。如果,我是说如果。广东独立了。中国会有什www.hao360.cn主页设置为http://hao.360.cn/,但打开360浏览器先显示www.yes125.com后转换为www.2345.com,搜索注册表和百度关键词价格查询百度推广关键词怎么扣费?百度关键词价格查询百度推广里怎么查指定的关键字参与竞价的价位呢陈嘉垣大家觉得陈嘉桓漂亮还是钟嘉欣漂亮?www.99cycy.com谁在这个http://www.sifangmall.com网站上买过东西?www.yahoo.com.hk香港的常用网站javmoo.comjavbus上不去.怎么办