enteredjp.ady9.info
jp.ady9.info 时间:2021-04-09 阅读:()
Maternalandfetalriskfactorsforstillbirth:populationbasedstudyOPENACCESSJasonGardosidirector1professorofmaternalandperinatalhealth2,VichithranieMadurasingheepidemiologist1,MandyWilliamsresearchmidwife1,AsadMalikdataanalyst1,AndréFrancisstatistician11WestMidlandsPerinatalInstitute,BirminghamB65RQ,UK;2UniversityofWarwickMedicalSchool,CoventryCV47AL,UKAbstractObjectiveToassessthemainriskfactorsassociatedwithstillbirthinamultiethnicEnglishmaternitypopulation.
DesignCohortstudy.
SettingNationalHealthServiceregioninEngland.
Population92218normallyformedsingletonsincluding389stillbirthsfrom24weeksofgestation,deliveredduring2009-11.
MainoutcomemeasureRiskofstillbirth.
ResultsMultivariableanalysisidentifiedasignificantriskofstillbirthforparity(para0andpara≥3),ethnicity(African,African-Caribbean,Indian,andPakistani),maternalobesity(bodymassindex≥30),smoking,pre-existingdiabetes,andhistoryofmentalhealthproblems,antepartumhaemorrhage,andfetalgrowthrestriction(birthweightbelow10thcustomisedbirthweightcentile).
Aspotentiallymodifiableriskfactors,maternalobesity,smokinginpregnancy,andfetalgrowthrestrictiontogetheraccountedfor56.
1%ofthestillbirths.
Presenceoffetalgrowthrestrictionconstitutedthehighestrisk,andthisappliedtopregnancieswheremothersdidnotsmoke(adjustedrelativerisk7.
8,95%confidenceinterval6.
6to10.
9),didsmoke(5.
7,3.
6to10.
9),andwereexposedtopassivesmokeonly(10.
0,6.
6to15.
8).
Fetalgrowthrestrictionalsohadthelargestpopulationattributableriskforstillbirthandwasfivefoldgreaterifitwasnotdetectedantenatallythanwhenitwas(32.
0%v6.
2%).
Intotal,195ofthe389stillbirthsinthiscohorthadfetalgrowthrestriction,butin160(82%)ithadnotbeendetectedantenatally.
Antenatalrecognitionoffetalgrowthrestrictionresultedindelivery10daysearlierthanwhenitwasnotdetected:median270(interquartilerange261-279)daysv280(interquartilerange273-287)days.
Theoverallstillbirthrate(per1000births)was4.
2,butonly2.
4inpregnancieswithoutfetalgrowthrestriction,increasingto9.
7withantenatallydetectedfetalgrowthrestrictionand19.
8whenitwasnotdetected.
ConclusionMostnormallyformedsingletonstillbirthsarepotentiallyavoidable.
Thesinglelargestriskfactorisunrecognisedfetalgrowthrestriction,andpreventivestrategiesneedtofocusonimprovingantenataldetection.
IntroductionStillbirthsrepresentadevastatingpregnancyoutcome,andtheneedforincreasedeffortsinpreventionhasbeenhighlightedbySANDS(StillbirthandNeonatalDeathCharity)1andotherparentledcampaigns.
StillbirthratesintheUnitedKingdomareamongthehighestinhighincomecountries2andhaveshownlittleimprovementsincetheearly1990s.
3DespitefreeavailabilityofpostmorteminvestigationsintheEnglishNationalHealthServiceasmanyas50-70%ofstillbirthshaveuntilrecentlybeencategorisedasunclassifiedorunexplained4andare,byimplication,oftenconsideredunavoidable.
5Furtherinvestigationfoundthatmanystillbornfetuseshadfailedtoreachtheirgrowthpotential,6-8andinclusionoffetalgrowthrestrictionasacategoryinstillbirthclassificationsresultedinasubstantialdroptoaround15%intheproportionofcasesconsideredunexplained.
89Thisencouragedarenewedfocusonunderstandingtheunderlying,mostlyplacentaldiseaserelated,causesoffetalgrowthrestriction.
Recentreportsoflaboratoryinvestigations10andpostmortemstudies11haveconfirmedthelargecontributionofplacentalfailureinthecauseofstillbirth.
Theclinicalrelevanceofsuchfindingsisthatalthoughtherearelimitedmeansbywhichtotreatfetalgrowthrestrictioninutero,recognitionthatthefetusisatriskafterappropriatematernal-fetalinvestigationscanleadtowelltimeddeliveryandimprovedperinataloutcome.
1213However,therearecurrentlynoestablishedandroutinelyusedmeanstopredictCorrespondenceto:JGardosijason.
gardosi@pi.
nhs.
ukExtramaterialsuppliedbytheauthor(seehttp://www.
bmj.
com/content/346/bmj.
f108tab=related#webextra)Sensitivityanalysisofexcludednon-significantriskfactorsSensitivityanalysiswithvarianceestimatesadjustedforclusteringmaternityunitsNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page1of14ResearchRESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfromstillbirth,andriskfactorsknownatthebeginningofpregnancyareconsideredweakpredictorsofoutcome.
14Weinvestigatedtheroleofdemographic,social,andmedicalriskfactorsthatcanbeascertainedatthebeginningofpregnancytogetherwiththosethatbecomeapparentaspregnancyprogresses,andtheirrespectivecontributionstotheincidenceofstillbirthsinanNHSregioninEnglandwithamultiethnicpopulation.
15Tofocusonpotentiallyavoidablefactorsweexcludedcongenitalanomalies,astheircontributiontostillbirthiscontingentonincidenceaswellasculturalchoicesonantenatalscreening,prenataldiagnosis,anddecisionsinresponsetopositiveresults.
Wethereforeexploredtheriskfactorsinpregnancieswithnormallyformedsingletonsandestimatedtherespectivecontributionofthesefactorstotheoverallburdenofstillbirthinourpopulation.
MethodsMaternitydataThedatabasewasderivedfromtheregional,NHSnetbasedperinatalepisodeelectronicrecord(PEER)hostedandmanagedbytheWestMidlandsPerinatalInstitute.
16ThiselectronicrecordwasfirstimplementedinApril2009inthe19maternityunitsintheWestMidlands.
Forthisstudyweusedthedatacollectedoveratwoyearperiod,representingbirthsbetweenJune2009andMay2011.
Thedataoriginatedfromprospectiverecordscreatedinthestandardisedhandheldmaternitynotesduringpregnancybythemidwivesanddoctors.
17Traineddataclerksintherespectivehospitalstransferinformationfromthenotesontotheperinatalepisodeelectronicrecordattheendofpregnancy.
Qualitywasassuredbycentralprojectstaffthroughtrainingworkshopsandregularon-sitedataqualityaudits.
Thedatasetcontained87regionallyagreedanddefineddataitems,18withinformationaboutmaternalcharacteristics,includingage,parity,ethnicorigin,andmaternalheightandweight(expressedasbodymassindex);socialfactors,includingemploymentstatusofthemotherandherpartner,consanguinitywiththepartner,andindexofmultipledeprivation;historyofmentalhealthproblems,pre-existingdiabetesorhypertensivedisease,orpreviousstillbirth;smokingstatus,alcoholconsumption,non-prescriptiondrugs,folicacidintake,andtimeoffirstvisitinpregnancy(theinformationforallthesepreviousvariableswasusuallyrecordedattheearlypregnancybookingvisit);complicationsinpregnancy,includinggestationaldiabetes,antepartumhaemorrhage,pregnancyinducedhypertension,andpre-eclampsia(definedaspregnancyinducedhypertensionwithproteinuria);andfetalorneonatalcharacteristics,includingsex,gestationalageandweightatbirth,andestimatedweightduringpregnancy.
Gestationalagewasdeterminedonthebasisofroutinelyoffereddatingscans,whichwerecarriedoutinthefirstorsecondtrimester(0.
05,potentialclusteringbymaternityunit,andtheeffectofrepeatpregnanciesfromthesamemother.
Toassesstheproportionofstillbirthsthatcouldbepotentiallypreventedifriskfactorswereremoved,wecalculatedadjustedpopulationattributableriskestimatesusingstandardmethods25:populationattributablerisk=expectednumberofcasesinthepopulationexpectednumberofcasesifnobodyinthepopulationhastheriskfactorofinterest/expectednumberofcasesinthepopulation*100TheanalysesweredoneusingstatisticalpackageSTATAversion11.
ResultsAtotalof105476caseswereenteredduringthetwoyearcollectionperiod.
Ofthese,13258wereexcludedbecauseofcongenitalanomalyormultiplepregnancy,whichleft92218normallyformedsingletonpregnanciesleadingto91829livebirthsand389stillbirths.
Thisrepresentedastillbirthrateof4.
2/1000birthsandcompareswithnationallyreportedstillbirthratesofnormallyformedsingletonsof3.
9-4.
1/1000overthesameperiod.
26Theanalysisincluded841(0.
9%)repeatpregnanciesduringthetwoyearperiodofthe92218mothersinthecohort.
UnivariateanalysisTable1liststhevariables,groupedaccordingtomaternalandfetalcharacteristics,socialfactors,medicalhistory,andcomplicationsduringpregnancy.
Analysiswasforcompletecasesonly.
Thestillbirthrateispresentedforsubgroups,togetherwithrelativerisksand95%confidenceintervalsinrelationtotherespectivereferencevalues.
Formaternalcharacteristics,stillbirthrateswereincreasedinfirstaswellasthirdandsubsequentpregnanciescomparedwithsecondpregnancies,andinmothersofAfrican,African-Caribbean,andSouthAsianethnicorigincomparedwiththeirEuropeancounterparts.
Firstgenerationmigrantshadanoverallhigherriskofstillbirth.
Maternalageindicatedaslightincreaseinyounger(0.
05inunivariateanalysis),ofclusteringofbirthswithinmaternityunits(seesupplementaryappendices1and2),andofrepeatpregnanciesbythesamemother(resultsnotshown)indicatedonlyminordifferencesinconfidenceintervalsandresultedinnochangesinrelativerisks.
First,third,andhigherorderpregnanciesweresignificantlyassociatedwithstillbirthaswerepregnanciesinAfrican,African-Caribbean,andIndianmothersandfirstgenerationmigrantsfromPakistan.
Obesity(bodymassindex>30),pre-existingdiabetes,historyofmentalhealthproblems,andantepartumhaemorrhageintheindexpregnancywereassociatedwithanincreasedriskofstillbirth.
Interactionsbetweenallvariablesweretestedandwerefoundtobenon-significant,withtheexceptionofastronginteractionbetweensmokingandfetalgrowthrestriction.
Thereforetheresultsarepresentedseparatelyforsmokerswithpregnanciesthatdidordidnothavefetalgrowthrestriction.
Activesmokingwasassociatedwithanincreasedriskofstillbirth(adjustedrelativerisk2.
5,95%confidenceinterval1.
7to3.
6),buttheassociationbecamesubstantiallystronger(5.
7,3.
6to8.
9)forNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page3of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrompregnancieswherethefetuswasalsogrowthrestricted.
Therewasnoassociationbetweenpassivesmokingandstillbirthunlessfetalgrowthrestrictionwasalsopresent,inwhichcasetherelativeriskwasevenhigherthanwithactivesmoking(10.
0,6.
6to15.
8).
Theriskofstillbirthwasincreasedforallpregnancieswithfetalgrowthrestriction,butwashighestwhenthemotherdidnotsmoke(7.
8,5.
6to10.
9).
Table3alsoliststhepopulationattributableriskderivedfromprevalenceandrelativeriskofeachsignificantfactor.
Themodelwasabletoattributeriskfactorsto80.
6%ofthestillbirthsinthiscohort.
Thehighestpopulationattributableriskswereassociatedwithfetalgrowthrestriction,primiparity,andantepartumhaemorrhage.
Inpregnancieswithfetalgrowthrestriction,theadjustedriskofstillbirthwas3.
4(2.
2to5.
2)iffetalgrowthrestrictionwasdetectedantenatally.
Theriskincreasedto6.
5(4.
9to8.
4)iffetalgrowthrestrictionwasnotdetected,and32%ofthestillbirthscouldbeattributedtothisgroup.
Pregnancieswithfetalgrowthrestrictiondetectedantenatallyweredeliveredonaverage10daysearlierthanthosenotdetectedantenatally(table4).
Justoverhalfofthestillbirths(203/389,52%)occurredafter34weeksofgestation.
Table5presentsthesignificantpathologicalfactorsofthemodel,adjustedformaternalcharacteristics,forstillbirthsbeforeandafter34weeksofgestation.
Forstillbirthsbetween24and33weeksofgestation,theonlysignificantfactorwasfetalgrowthrestriction(adjustedrelativerisk4.
0,2.
9to5.
6),whichaccountedforjustunderhalfofthestillbirths(populationattributablerisk49.
5%).
Atthesametime,pre-eclampsiaemergedasasignificantprotectivefactor.
From34weeksofgestation,fetalgrowthrestrictionagainrepresentedthestrongestrisk,andwashighestinpregnancieswherethemotherdidnotsmoke.
DiscussionOurstudyshowsthatwhilethereareseveralriskfactorsforstillbirththatcanbeascertainedfromtheoutsetofpregnancy,thesinglelargestfactorisfetalgrowthrestriction,whichiscurrentlynotwellpredictedandnotrecognisedantenatallyinmostpregnancies.
Consideringthatmostinstancesaremissed,aretrospectivedefinitionoffetalgrowthrestrictionusinggrowthpotential19appliedtobirthweightwasimportanttobeabletoquantifythelinkwithstillbirth.
Thefindingsindicatetheimportanceofimprovingcurrentstrategiesandprotocolsforimprovedsurveillanceoffetalgrowththroughouttheantenatalperiod.
13EarlypregnancyriskfactorsThepopulationbaseddataderivedfromawholeNHSregionallowedustoassessseveralknownaswellasnewriskfactorsthatwillrequirefurtherinvestigationinfuturestudies.
Thesefactorshavevaryingclinicalimplications.
Parity,ethnicity,andpreviousmentalhealthproblemsareindicatorsofriskelicitedatthebeginningofpregnancy.
Theassociationbetweennulliparityandstillbirthreflectsotherreports,14butwealsoobserveda60%increaseinriskformotherswithaparityof3orhigher,suggestingaU-shapedrelationbetweenparityandriskofstillbirth(table2),aspreviouslyreported.
27Contrarytoasystematicreview,28wefoundnosignificantincreaseinriskofstillbirthwitholdermaternalage(table1).
Thismaybebecauseweexcludedcongenitalanomaliesfromourcohort,whichareknowntobeincreasedinoldermothers.
29Thisisconsistentwitharecentreportwhichfoundthattheassociationbetweenstillbirthandmaternalagedisappearswhencongenitalanomaliesareexcluded.
14Motherslivinginthemostdeprivedareashadanincreasedriskofstillbirth,asdidwomenwhowereorhadapartnerwhowasunemployed.
Ethnicorracialdisparitiesinstillbirthrateshavebeenhighlighted1430andwerealsoindependentriskfactorsinourstudy.
Eachofthemainethnicminoritygroupsinourpopulationhadanincreasedriskofstillbirth(table3).
Furtherworkisrequiredtohelpunderstandthereasonsfortheincreasedriskinthesegroups.
Alimitationofourstudyisthatconsentratesforpostmortemexaminationsarelowinsomeethnicgroups,asaresultofwhichsomecaseswithundiagnosedcongenitalanomaliesmayhavebeeninadvertentlyincludedinourcohort.
Amongpre-existingconditions,diabetesisaknownriskfactor31andhadahigherrisk(adjustedrelativerisk3.
9,1.
7to8.
9),butapopulationattributableriskofonly2.
0%becauseofthelowprevalenceinthiscohort.
Ahistoryofmentalhealthproblemswasalsoasignificantriskfactor(adjustedrelativerisk1.
4,1.
0to1.
9),reportedby11.
7%ofmothers.
Ithasbeensuggestedthatthelinkbetweenmentalillnessandadverseoutcomecouldbemediatedthroughgeneralfactorssuchasinsufficientattendanceatantenatalclinicsorunhealthylifestyles.
32Antenatalhaemorrhageincludingplacentalabruptionhasaknownassociationwithstillbirth28;ourresultsconfirmthislinkandemphasisetheneedforimmediate,thoroughinvestigationofanyantepartumbleeding.
Bodymassindexcategoriesof30-34.
9and35ormorerepresenteda40%and60%increasedriskofstillbirth,respectively,andtogetherwereprevalentinjustunder20%ofthiscohort,resultinginapopulationattributableriskof8.
7%.
Contrarytosomereports,14wefoundnoincreaseinriskofstillbirthassociatedwithoverweightmothers(bodymassindex25-29.
9)inourpopulation.
ActiveandpassivesmokingMaternalsmokinginearlypregnancyisassociatedwithstillbirth,withanaverageriskof1.
36basedonfourstudies.
28Wefoundtherisktobehigher(relativerisk1.
8,95%confidenceinterval1.
4to2.
3,table1),possiblyasaresultofhighlevelsofsocialdeprivationinourpopulation,whichisstronglylinkedtosmoking.
33However,thedatabasealsoallowedustoexaminetheinteractionbetweensmokingandfetalgrowth,andtheeffectonstillbirthriskwhenfetalgrowthrestrictionisdetectedantenatally.
Theincreasedriskofsmokingworksmostlythroughfetalgrowthrestriction,andtherateofstillbirthinpregnanciesofmotherswhosmokedbuthadnofetalgrowthrestrictionwassimilar(3.
7)tothatofmotherswhowerenon-smokers(3.
8,table2).
Thishighlightstheimportanceofearlypregnancysmokingcessationprogrammes,whichhavebeenfoundtoreducesmallnessforgestationalageandprematurity.
34Interestingly,thehigheststillbirthratewasinnon-smokingpregnantwomenwithfetalgrowthrestriction,whichcouldbebecausethesepregnanciesareconsideredlowriskandfetalgrowthrestrictionislesslikelytobedetectedantenatally.
Wewerealsoabletoquantifytheeffectofpassiveorenvironmentalsmoking,andfoundittobeassociatedwithanincreaseinriskofstillbirthby30%(table1)—aneffectcorrespondingtothe23%reportedinarecentmetaanalysisoffourtrials.
35Howeverinthemultivariablemodelthisfactorwassignificantonlywhentherewasfetalgrowthrestriction,inwhichcasetheriskevenexceededthatassociatedwiththemotherNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page4of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrombeingasmoker(adjustedrelativerisk10.
0,95%confidenceinterval6.
6to15.
8;table3).
Thisobservationneedsconfirmationinfuturestudiesbutcouldhaveseveralplausibleexplanations.
Passivesmoking,resultingfromthe"sidestream"effectofsmokeproducedbetweenpuffs,hasbeenshowninanimalstudiestobefourtimesastoxicas"mainstream"smoke,36andthismayextendtofetusesduringpregnancy.
Also,thatanon-smokingmotherlivesinasmokingenvironmentmaybemissed,resultinginthepregnancynotbeingaffordedthesameclinicalattention,includingconcernaboutfetalgrowth.
ModifiablefactorsOverall,thelargestpopulationattributablerisk(37.
4%)wasassociatedwithfetalgrowthrestrictionwithandwithoutsmoking,followedbymaternalsmokingwithoutfetalgrowthrestriction(9.
4%)andobesity(bodymassindex≥30;populationattributablerisk8.
7%,table3).
Thesethreevariablescouldbeconsideredasthepotentiallymostmodifiablefactorsand,allowingforoverlap,togetheraccountedfor55.
5%ofstillbirthsinourcohort.
Howevertheyhavedifferentimplicationsforprevention.
Reductionofsmokingandobesityrequireconcertedpublichealtheffortsandeducationprogrammesforwomenofchildbearingage,aswellasthemothers'cooperationwithsmokingcessationprogrammesduringpregnancy.
Theeffectivenessofsuchprogrammesisnotalwaysclear.
Ontheotherhand,theriskofstillbirthasaresultoffetalgrowthrestrictioncanbereducedbyearlyidentificationoftheconditionandreferralforinvestigationsbyultrasoundandDopplerimaging.
12FetalgrowthrestrictionandantenataldetectionTheoveralldetectionrateoffetalgrowthrestrictionwasonly31%,lowerthanthatachievedinourcontrolledstudyinNottinghamusingcustomisedcharts(48%)37andarecentreportfromAustralia(51%).
38However,wefoundthatthedetectionrateinourpopulationrangedwidelybetweenmaternityunits(12.
5-50.
0%),39varyingwiththeamountofstafftrainingandadherencetoprotocols.
Thishighlightstheimportanceofastandardisedandqualityassuredapproachtotheantenatalsurveillanceoffetalgrowthinroutineclinicalpractice.
Amongthecohortof389stillbirths,thedetectionratewasevenlower:195(50.
1%)ofthecaseshadfetalgrowthrestrictionandin160(82.
1%)fetalgrowthrestrictionwasnotdetectedantenatally(table1).
Thepotentialpreventabilityofstillbirthsassociatedwithfetalgrowthrestrictionisillustratedbythereducedriskafterantenataldetection(fig1andtable1).
Althoughpregnancieswithfetalgrowthrestrictionhaveaneighttimeshigherrateofstillbirth(16.
7v2.
1,fig1),thisriskisreducedwhenfetalgrowthrestrictionisdetected(9.
7),althoughnottothesamelevelsasinnon-fetalgrowthrestrictedpregnancies.
Thisislikelytobebecausethebabyisoftennotdeliveredimmediately,eitherduetoinappropriatedelaysorbecauseofconcernsaboutneonatalimmaturity.
Conversely,theriskishigherstilliffetalgrowthrestrictionispresentbutnotdetected.
Theseassociationsarealsoshownwhenallotherfactorsareadjustedforinthemultivariableanalysis(table4):thepopulationattributableriskof32.
0%indicatesthatfivetimesasmanystillbirthsareassociatedwithundetectedantenatalfetalgrowthrestrictionthanwithdetectedfetalgrowthrestriction(6.
2).
Pregnancieswithfetalgrowthrestrictionweredeliveredonaverage10daysearlierthanthosewithout,butstillatrelativelymaturegestationswhendetectedthanwhennot(median270v280days;table4).
Basedontheprevalenceofundetectedfetalgrowthrestriction(9.
2%,table4)andthelowerriskofstillbirthwhenitisdetected(adjustedrelativerisk3.
4),18.
2%or71stillbirthsinourcohortcouldhavebeenavoidedthroughimprovedantenataldetection.
ExtrapolatedtotheUKpopulation,thiswouldrepresent600fewerstillbirthsperyear.
Thesubanalysisofthemultivariablemodelbyearlyandlategestationalagecategories(table5)showedfetalgrowthrestrictionagaintobethestrongestfactorforriskofstillbirthafter34weeksofgestation,withthehighestriskinpregnancieswherethemotherdidnotsmoke.
Before34weeksofgestation,fetalgrowthrestrictionwasthesinglesignificantfactorandaccountedforclosetohalfofallstillbirths(populationattributablerisk49.
5%).
Theseresultssupportthenotionofdifferingpatternsofplacentaldiseaseinearlyandlateonsetfetalgrowthrestriction.
1013Theprotectiveeffectofpre-eclampsia(table5)isinterestingbutnotsurprising:thediseaseisoftenassociatedwithfetalgrowthrestriction,butasthesepregnanciesareoftendeliveredearlyformaternalreasons,thebabyisremovedfromahighriskintrauterineenvironment.
ImplicationsforcliniciansandcommissionersTheincreasedriskofstillbirthafterundetectedfetalgrowthproblemsisconsistentwithanineyearreviewofdeliveriesinasingleunitinMalm40andarecentcase-controlstudyfromAuckland.
41InourdatabasefromalargeNHSregion,wewereabletoquantifytheimportanceofthisriskfactorandestablishitspre-eminentassociationwithstillbirthevenafteradjustmentformedical,social,anddemographicriskfactorsthatcanbeascertainedinearlypregnancy.
Mostcasesoffetalgrowthrestrictiondonotmanifestuntilthethirdtrimesterofpregnancy,andintheabsenceofeffectivescreeningtests,preventionstrategiesneedtoincludeanenhancedlevelofsurveillancethroughoutpregnancy.
Ourfindingssuggestthatearlydetectionoffetalgrowthproblemscansubstantiallyreducetheriskofstillbirth,andneedstobecomeacornerstoneandkeyindicatorofsafetyandeffectivenessinantenatalcare.
Wethankourregionalnetworkofbereavementmidwiveswhosubmitnotificationsonallperinataldeaths;AnnTonks,CatherineFranklin,andRobynCaleywhoruntheregionalperinatalmortalityregistersforensuringhighqualityascertainment;thenetworkofunitbaseddataclerkswhoentertheregionalmaternitydatasetforeachpregnancyonthePEERelectronicrecord(www.
pi.
nhs.
uk/peer);andMichelleSouthamandLorraineEcclestoneforensuringdataqualitythrougharollingprogrammeoftrainingandaccuracyaudits.
Contributors:Allauthorshadfullaccesstothedata,assistedwithitsanalysisandinterpretationoftheresults,andreviewedandapprovedthefinalmanuscript.
JGdevelopedthestudydesign,assistedwiththeanalysisandinterpretation,andwrotethepaper.
Hehasfinalresponsibilitytosubmitforpublication,andistheguarantor.
Funding:DatacollectionandanalyticalstaffwerefinanciallysupportedbyNHSWestMidlandsStrategicHealthAuthorityandallprimarycaretrusts.
Thefundershadnoinfluenceonthestudydesign,analysis,interpretation,writingupofthemanuscript,orthedecisiontosubmitforpublication.
Competinginterests:AllauthorshavecompletedtheICMJEuniformdisclosureformatwww.
icmje.
org/coi_disclosure.
pdf(availableonrequestfromthecorrespondingauthor)anddeclare:nosupportfromanyorganisationforthesubmittedwork;nofinancialrelationshipswithanyorganisationsthatmighthaveaninterestinthesubmittedworkinthepreviousthreeyears,andnootherrelationshipsoractivitiesthatcouldappeartohaveinfluencedthesubmittedwork.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page5of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromWhatisalreadyknownonthistopicStillbirthrateshavechangedlittleintheEnglishNationalHealthServiceoverthepasttwodecadesManyhaveconventionallybeenconsideredunexplainedandunavoidableRiskfactorshavegenerallybeenconsideredweakpredictorsofstillbirthWhatthisstudyaddsMaternalobesity,smoking,andfetalgrowthrestriction,potentiallymodifiableriskfactors,togetheraccountforthemajorityofnormallyformedstillbirthsComparedwithpregnancieswithnormalgrowth,thestillbirthrateinthosewithfetalgrowthrestrictionincreasedfourfold,andincreasedfurthertoeightfoldifgrowthrestrictionwasnotdetectedantenatallyFetalgrowthrestrictioniscurrentlymissedinmostpregnancies,andbetterantenataldetectionneedstobecomeacornerstoneandkeyindicatorofsafetyandeffectivenessinmaternitycareEthicalapproval:Notrequired;datawerecollectedwithpatientconsentandwerepseudonymisedbeforeanalysis.
Datasharing:Noadditionaldataavailable.
1SavingBabiesLivesReport.
StillbirthandNeonatalDeathCharity(SANDS),2009.
2012.
www.
why17.
org/fileadmin/content/About_Sands/03520_Saving_babies_lives_watermarked.
pdf.
2FlenadyV,MiddletonP,SmithGC,DukeW,ErwichJJ,YeeKhongT,etal.
Stillbirths:thewayforwardinhigh-incomecountries.
Lancet2011;377:1703-17.
3OfficeforNationalStatistics(2011).
Deathregistrationsummarytables,England&Wales,2010.
2012.
www.
ons.
gov.
uk/ons/publications/re-reference-tables.
htmledition=tcm%3A77-230730.
4ConfidentialEnquiryintoMaternalandChildHealth(CEMACH).
Perinatalmortality2006:England,WalesandNorthernIreland.
CEMACH,2008.
(Table4.
2).
5GardosiJ.
Clinicalimplicationsof'unexplained'stillbirths.
In:MaternalandChildHealthResearchConsortium,ed:CESDI8thannualreport.
ConfidentialEnquiryintoStillbirthsandDeathsinInfancy,2001:40-7.
6GardosiJ,MulT,MongelliM,FaganD.
Analysisofbirthweightandgestationalageinantepartumstillbirths.
BJOG1998;105:524-30.
7FroenJF,GardosiJ,ThurmannA,FrancisA,Stray-PedersenB.
Restrictedfetalgrowthinsuddenintrauterineunexplaineddeath.
ActaObstetGynecolScand2004;83:81-7.
8GardosiJ,KadySM,McGeownP,FrancisA,TonksA.
Classificationofstillbirthbyrelevantconditionatdeath(ReCoDe):populationbasedcohortstudy.
BMJ2005;331:1113-7.
9VerganiP,CozzolinoS,PozziE,CuttinMS,GrecoM,OrnaghiS,etal.
Identifyingthecausesofstillbirth:acomparisonoffourclassificationsystems.
AmJObstetGynecol2008;199:319.
e1-4.
10KortewegFJGordijnSJ,TimmerA,HolmJP,RaviseJM,ErwichJJ.
Aplacentalcauseofintra-uterinefetaldeathdependsontheperinatalmortalityclassificationsystemused.
Placenta2008;29:71-8.
11StillbirthCollaborativeResearchNetworkWritingGroup.
Causesofdeathamongstillbirths.
JAMA2011;306:2459-68.
12AlfirevicZ,NielsonJP.
Dopplerultrasonographyinhighriskpregnancies:systematicreviewwithmeta-analysis.
AmJObstetGynecol1995;172:1379-87.
13FiguerasF,GardosiJ:Intrauterinegrowthrestriction:newconceptsinantenatalsurveillance,diagnosis,andmanagement.
AmJObstetGynecol2010;doi:10.
1016/j.
ajog.
2010.
08.
05514StillbirthCollaborativeResearchNetworkWritingGroup.
Associationbetweenstillbirthandriskfactorsknownatpregnancyconfirmation.
JAMA2011;306:2469-79.
15KeyHealthDatafortheWestMidlands—2009.
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/pnm.
16PerinatalEpisodeElectronicRecord(PEER).
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/peer.
17Pregnancynotes.
NHSPerinatalInstitute.
2012.
www.
preg.
info.
18WestMidlandsCoreMaternityDatasetv1.
7,2009.
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/peer/WM_Maternity_Dataset_v1.
7.
pdf.
19GROW(GestationRelatedOptimalWeight)softwareversion6.
5(UK).
GestationNetwork.
2012.
www.
gestation.
net.
20GardosiJ,ChangA,KalyanB,SahotaD,SymondsEM.
Customisedantenatalgrowthcharts.
Lancet1992;339:283-7.
21GardosiJ,MongelliM,WilcoxM,ChangA.
Anadjustablefetalweightstandard.
UltrasoundObstetGynecol1995;6:168-74.
22GardosiJ.
Customisedassessmentoffetalgrowthpotential:implicationsforperinatalcare.
ArchDisChildFetalNeonatalEd2012;doi:10.
1136/fetalneonatal-2012-301708.
23DeJongCL,FrancisA,VanGeijnHP,GardosiJ.
Customizedfetalweightlimitsforantenataldetectionoffetalgrowthrestriction.
UltrasoundObstetGynecol2000;15:36-40.
24GenestDR,WilliamsMA,GreeneMF.
Estimatingthetimeofdeathinstillbornfetuses:I.
Histologicevaluationoffetalorgans;anautopsystudyof150stillborns.
ObstetGynecol1992;80:575-84.
25KooperbergC,PetittiDB.
Usinglogisticregressiontoestimatetheadjustedattributableriskoflowbirthweightinanunmatchedcase-controlstudy.
Epidemiology1991;2:363-6.
26ConfidentialEnquiryintoMaternalandChildHealth.
Perinatalmortality2007.
CEMACH,2009:21.
27BaiJ,WongFW,BaumanA,MohsinM.
Parityandpregnancyoutcomes.
AmJObstetGynecol2002;186:274-8.
28FlenadyV,KoopmansL,MiddletonP,FrenF,SmithGC,GibbonsK,etal.
Majorriskfactorsforstillbirthinhigh-incomecountries:asystematicreviewandmeta-analysis.
Lancet2011;377:1331-40.
29HollierLM,LevenoKJ,KellyMA,McIntireDD,CunninghamFG.
Maternalageandmalformationsinsingletonbirths.
ObstetGynecol2000;96:701-6.
30ReeskeA,KutschmannM,RazumO,SpallekJ.
Stillbirthdifferencesaccordingtoregionsoforigin:ananalysisoftheGermanperinataldatabase,2004-2007.
BMCPregnancyChildbirth2011;11:63.
31PerssonM,NormanM,HansonU.
Obstetricandperinataloutcomesintype1diabeticpregnancies:alarge,population-basedstudy.
DiabetesCare2009;32:2005-9.
32King-HeleS,WebbRT,MortensenPB,ApplebyL,PicklesA,AbelKM.
Riskofstillbirthandneonataldeathlinkedwithmaternalmentalillness:anationalKing-Helecohortstudy.
ArchDisChildFetalNeonatalEd.
2009;94:F105-10.
33GoyaJ,DoddL,RosenbergMWKingaWDHealth-riskbehaviours:examiningsocialdisparitiesintheoccurrenceofstillbirthPaediatrPerinatalEpidemiol2008;22:314-20.
34McCowanLM,DekkerGA,ChanE,StewartA,ChappellLC,HunterM,etal.
Spontaneouspretermbirthandsmallforgestationalageinfantsinwomenwhostopsmokingearlyinpregnancy:prospectivecohortstudy.
BMJ2009;26;338:b1081.
Erratumin:BMJ2009;338.
doi:10.
1136/bmj.
b1558.
35Leonardi-BeeJ,BrittonJ,VennA.
Secondhandsmokeandadversefetaloutcomesinnonsmokingpregnantwomen:ameta-analysis.
Pediatrics2011;127:734-41.
36SchickS,GlantzS.
PhilipMorristoxicologicalexperimentswithfreshsidestreamsmoke:moretoxicthanmainstreamsmoke.
TobControl2005;14:396-404.
37GardosiJ,FrancisA.
Controlledtrialoffundalheightmeasurementplottedoncustomisedantenatalgrowthcharts.
BJOG1999;106:309-17.
38RoexA,NikpoorP,vanEerdE,HodylN,DekkerG.
Serialplottingoncustomisedfundalheightchartsresultsindoublingoftheantenataldetectionofsmallforgestationalagefetusesinnulliparouswomen.
AustNZJObstetGynaecol2012;52:78-82.
doi:10.
1111/j.
1479-828X.
2011.
01408.
x.
39WestMidlandsPerinatalKPIReport,Q22010/11.
PerinatalInstitute,2011.
2012.
www.
pi.
nhs.
uk/pnm/maternitydata/Q2_2010-11_Perinatal_KPI_report.
pdf.
40LindqvistPG,MolinJ.
Doesantenatalidentificationofsmall-for-gestationalagefetusessignificantlyimprovetheiroutcomeUltrasoundObstetGynecol2005;25:258-64.
41StaceyT,ThompsonJM,MitchellEA,ZuccolloJM,EkeromaAJ,McCowanLM.
Antenatalcare,identificationofsuboptimalfetalgrowthandriskoflatestillbirth:findingsfromtheAucklandStillbirthStudy.
AustNZJObstetGynaecol2012.
doi:10.
1111/j.
1479-828X.
2011.
01406.
Accepted:18December2012Citethisas:BMJ2013;346:f108Thisisanopen-accessarticledistributedunderthetermsoftheCreativeCommonsAttributionNon-commercialLicense,whichpermitsuse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited,theuseisnoncommercialandisotherwiseincompliancewiththelicense.
See:http://creativecommons.
org/licenses/by-nc/2.
0/andhttp://creativecommons.
org/licenses/by-nc/2.
0/legalcode.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page6of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTablesTable1|UnivariateanalysisofriskfactorsassociatedwithstillbirthscomparedwithlivebirthsRelativerisk(95%CI)Rate/1000birthsNo(%)ofstillbirthsNo(%)ofallbirthsRiskfactors—4.
2389(100)92218(100)TotalGeneralmaternalcharacteristicsn=389n=92208Age(years):1.
3(0.
9to1.
9)5.
133(8.
5)6456(7.
0)90n=380n=88053Fetalgrowthrestriction:Reference2.
4185(48.
7)76356(86.
7)NoYes4.
0(2.
8to5.
7)9.
735(9.
2)3601(4.
1)Detectedantenatally8.
0(6.
5to9.
9)19.
8160(42.
1)8096(9.
2)Notdetectedantenatally*Placeofbirthcombinedifeithersubgroup<1000women.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page9of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable2|Smokingandfetalgrowthrestriction(birthweight<10thgestationrelatedoptimalweightcentile)Stillbirthrate/1000birthsProportionoftotal(%)Variables4.
2100.
0All5.
818.
7Smokers:13.
04.
3Fetalgrowthrestriction3.
713.
7Nofetalgrowthrestriction3.
881.
3Non-smokers:18.
38.
3Fetalgrowthrestriction2.
168.
7NofetalgrowthrestrictionNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page10of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable3|Multivariableanalysisofsignificant(P<0.
1)riskfactorsintable1Populationattributablerisk(%)Prevalence(%)PvalueAdjustedrelativerisk(95%CI)VariablesParity:21.
343.
4<0.
011.
8(1.
3to2.
5)04.
69.
40.
051.
6(1.
0to2.
5)≥3Ethnicorigin,placeofbirth:2.
93.
00.
012.
4(1.
2to4.
6)African*2.
22.
00.
012.
3(1.
3to4.
1)African-Caribbean*3.
95.
2<0.
012.
1(1.
3to3.
5)Indian*6.
44.
6<0.
013.
0(1.
9to4.
8)Pakistani,non-UKBodymassindex:4.
512.
50.
071.
4(1.
0to2.
0)30-34.
94.
27.
30.
031.
6(1.
1to2.
4)≥354.
711.
70.
061.
4(1.
0to1.
9)Mentalhealthhistory2.
00.
7<0.
013.
9(1.
7to8.
9)Pre-existingdiabetes15.
58.
1<0.
013.
4(2.
6to4.
5)AntepartumhaemorrhageMaternalsmoking,nofetalgrowthrestriction9.
414.
9<0.
012.
5(1.
7to3.
6)Activesmoker—15.
70.
281.
3(0.
8to2.
0)PassivesmokerMaternalsmoking,fetalgrowthrestriction:6.
14.
6<0.
015.
7(3.
6to8.
9)Activesmoker9.
12.
1<0.
0110.
0(6.
6to15.
8)Passivesmoker22.
26.
5<0.
017.
8(5.
6to10.
9)Fetalgrowthrestriction,non-smokerReferencegroup:para1,UKborn,non-smokingEuropeanmother;bodymassindex18.
5-24.
9.
*UKandnon-UKgroupscombinedbecauseofsmallnumbers.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page11of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable4|Gestationalageatdeliveryandriskofstillbirthsinpregnancieswithfetalgrowthrestriction*,withandwithoutantenataldetectionPopulationattributablerisk(%)PvalueAdjustedrelativerisk(95%CI)Median(interquartilerange)gestationalageatdelivery(days)Prevalence(%)VariablesReference280(273-286)86.
8NofetalgrowthrestrictionFetalgrowthrestriction:6.
2<0.
013.
4(2.
2to5.
2)270(261-279)4.
0Detectedantenatally32.
0<0.
016.
5(4.
9to8.
4)280(273-287)9.
2Notdetectedantenatally*Adjustedforethnicity,parity,bodymassindex,pre-eclampsia,antepartumhaemorrhage,historyofmentalhealthproblems,andsmoking.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page12of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable5|Fetalgrowthrestrictionandotherpathologicalfactorsbeforeandafter34weeksofgestationPopulationattributablerisk(%)Prevalence(%)PvalueAdjustedrelativerisk*(95%CI)Variables24-33weeks13.
210.
5<0.
010.
3(0.
1to0.
6)Pre-eclampsia49.
514.
3<0.
014.
0(2.
9to5.
6)Fetalgrowthrestriction≥34weeksBodymassindex:9.
912.
0<0.
011.
9(1.
3to3.
0)30-345.
17.
30.
021.
8(1.
1to3.
0)≥357.
611.
30.
041.
7(1.
0to2.
7)Mentalhealthhistory9.
116.
60.
011.
6(1.
1to2.
3)Latebooking13.
07.
5<0.
013.
1(2.
0to4.
7)Antepartumhaemorrhage7.
314.
10.
021.
7(1.
1to2.
7)Smoker,nofetalgrowthrestriction2.
54.
30.
012.
5(1.
3to5.
1)Smoker,fetalgrowthrestriction22.
78.
0<0.
015.
1(3.
4to7.
6)Fetalgrowthrestriction,non-smoker*Adjustedforethnicity,maternalage,parity,andbodymassindex.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page13of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromFiguresFig1StillbirthratesinrelationtofetalgrowthrestrictionandwhetheritwasdetectedantenatallyFig2Stillbirthsandlivebirthswithandwithoutfetalgrowthrestriction:cumulativepercentagegraphofgestationalageatdeliveryNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page14of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrom
DesignCohortstudy.
SettingNationalHealthServiceregioninEngland.
Population92218normallyformedsingletonsincluding389stillbirthsfrom24weeksofgestation,deliveredduring2009-11.
MainoutcomemeasureRiskofstillbirth.
ResultsMultivariableanalysisidentifiedasignificantriskofstillbirthforparity(para0andpara≥3),ethnicity(African,African-Caribbean,Indian,andPakistani),maternalobesity(bodymassindex≥30),smoking,pre-existingdiabetes,andhistoryofmentalhealthproblems,antepartumhaemorrhage,andfetalgrowthrestriction(birthweightbelow10thcustomisedbirthweightcentile).
Aspotentiallymodifiableriskfactors,maternalobesity,smokinginpregnancy,andfetalgrowthrestrictiontogetheraccountedfor56.
1%ofthestillbirths.
Presenceoffetalgrowthrestrictionconstitutedthehighestrisk,andthisappliedtopregnancieswheremothersdidnotsmoke(adjustedrelativerisk7.
8,95%confidenceinterval6.
6to10.
9),didsmoke(5.
7,3.
6to10.
9),andwereexposedtopassivesmokeonly(10.
0,6.
6to15.
8).
Fetalgrowthrestrictionalsohadthelargestpopulationattributableriskforstillbirthandwasfivefoldgreaterifitwasnotdetectedantenatallythanwhenitwas(32.
0%v6.
2%).
Intotal,195ofthe389stillbirthsinthiscohorthadfetalgrowthrestriction,butin160(82%)ithadnotbeendetectedantenatally.
Antenatalrecognitionoffetalgrowthrestrictionresultedindelivery10daysearlierthanwhenitwasnotdetected:median270(interquartilerange261-279)daysv280(interquartilerange273-287)days.
Theoverallstillbirthrate(per1000births)was4.
2,butonly2.
4inpregnancieswithoutfetalgrowthrestriction,increasingto9.
7withantenatallydetectedfetalgrowthrestrictionand19.
8whenitwasnotdetected.
ConclusionMostnormallyformedsingletonstillbirthsarepotentiallyavoidable.
Thesinglelargestriskfactorisunrecognisedfetalgrowthrestriction,andpreventivestrategiesneedtofocusonimprovingantenataldetection.
IntroductionStillbirthsrepresentadevastatingpregnancyoutcome,andtheneedforincreasedeffortsinpreventionhasbeenhighlightedbySANDS(StillbirthandNeonatalDeathCharity)1andotherparentledcampaigns.
StillbirthratesintheUnitedKingdomareamongthehighestinhighincomecountries2andhaveshownlittleimprovementsincetheearly1990s.
3DespitefreeavailabilityofpostmorteminvestigationsintheEnglishNationalHealthServiceasmanyas50-70%ofstillbirthshaveuntilrecentlybeencategorisedasunclassifiedorunexplained4andare,byimplication,oftenconsideredunavoidable.
5Furtherinvestigationfoundthatmanystillbornfetuseshadfailedtoreachtheirgrowthpotential,6-8andinclusionoffetalgrowthrestrictionasacategoryinstillbirthclassificationsresultedinasubstantialdroptoaround15%intheproportionofcasesconsideredunexplained.
89Thisencouragedarenewedfocusonunderstandingtheunderlying,mostlyplacentaldiseaserelated,causesoffetalgrowthrestriction.
Recentreportsoflaboratoryinvestigations10andpostmortemstudies11haveconfirmedthelargecontributionofplacentalfailureinthecauseofstillbirth.
Theclinicalrelevanceofsuchfindingsisthatalthoughtherearelimitedmeansbywhichtotreatfetalgrowthrestrictioninutero,recognitionthatthefetusisatriskafterappropriatematernal-fetalinvestigationscanleadtowelltimeddeliveryandimprovedperinataloutcome.
1213However,therearecurrentlynoestablishedandroutinelyusedmeanstopredictCorrespondenceto:JGardosijason.
gardosi@pi.
nhs.
ukExtramaterialsuppliedbytheauthor(seehttp://www.
bmj.
com/content/346/bmj.
f108tab=related#webextra)Sensitivityanalysisofexcludednon-significantriskfactorsSensitivityanalysiswithvarianceestimatesadjustedforclusteringmaternityunitsNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page1of14ResearchRESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfromstillbirth,andriskfactorsknownatthebeginningofpregnancyareconsideredweakpredictorsofoutcome.
14Weinvestigatedtheroleofdemographic,social,andmedicalriskfactorsthatcanbeascertainedatthebeginningofpregnancytogetherwiththosethatbecomeapparentaspregnancyprogresses,andtheirrespectivecontributionstotheincidenceofstillbirthsinanNHSregioninEnglandwithamultiethnicpopulation.
15Tofocusonpotentiallyavoidablefactorsweexcludedcongenitalanomalies,astheircontributiontostillbirthiscontingentonincidenceaswellasculturalchoicesonantenatalscreening,prenataldiagnosis,anddecisionsinresponsetopositiveresults.
Wethereforeexploredtheriskfactorsinpregnancieswithnormallyformedsingletonsandestimatedtherespectivecontributionofthesefactorstotheoverallburdenofstillbirthinourpopulation.
MethodsMaternitydataThedatabasewasderivedfromtheregional,NHSnetbasedperinatalepisodeelectronicrecord(PEER)hostedandmanagedbytheWestMidlandsPerinatalInstitute.
16ThiselectronicrecordwasfirstimplementedinApril2009inthe19maternityunitsintheWestMidlands.
Forthisstudyweusedthedatacollectedoveratwoyearperiod,representingbirthsbetweenJune2009andMay2011.
Thedataoriginatedfromprospectiverecordscreatedinthestandardisedhandheldmaternitynotesduringpregnancybythemidwivesanddoctors.
17Traineddataclerksintherespectivehospitalstransferinformationfromthenotesontotheperinatalepisodeelectronicrecordattheendofpregnancy.
Qualitywasassuredbycentralprojectstaffthroughtrainingworkshopsandregularon-sitedataqualityaudits.
Thedatasetcontained87regionallyagreedanddefineddataitems,18withinformationaboutmaternalcharacteristics,includingage,parity,ethnicorigin,andmaternalheightandweight(expressedasbodymassindex);socialfactors,includingemploymentstatusofthemotherandherpartner,consanguinitywiththepartner,andindexofmultipledeprivation;historyofmentalhealthproblems,pre-existingdiabetesorhypertensivedisease,orpreviousstillbirth;smokingstatus,alcoholconsumption,non-prescriptiondrugs,folicacidintake,andtimeoffirstvisitinpregnancy(theinformationforallthesepreviousvariableswasusuallyrecordedattheearlypregnancybookingvisit);complicationsinpregnancy,includinggestationaldiabetes,antepartumhaemorrhage,pregnancyinducedhypertension,andpre-eclampsia(definedaspregnancyinducedhypertensionwithproteinuria);andfetalorneonatalcharacteristics,includingsex,gestationalageandweightatbirth,andestimatedweightduringpregnancy.
Gestationalagewasdeterminedonthebasisofroutinelyoffereddatingscans,whichwerecarriedoutinthefirstorsecondtrimester(0.
05,potentialclusteringbymaternityunit,andtheeffectofrepeatpregnanciesfromthesamemother.
Toassesstheproportionofstillbirthsthatcouldbepotentiallypreventedifriskfactorswereremoved,wecalculatedadjustedpopulationattributableriskestimatesusingstandardmethods25:populationattributablerisk=expectednumberofcasesinthepopulationexpectednumberofcasesifnobodyinthepopulationhastheriskfactorofinterest/expectednumberofcasesinthepopulation*100TheanalysesweredoneusingstatisticalpackageSTATAversion11.
ResultsAtotalof105476caseswereenteredduringthetwoyearcollectionperiod.
Ofthese,13258wereexcludedbecauseofcongenitalanomalyormultiplepregnancy,whichleft92218normallyformedsingletonpregnanciesleadingto91829livebirthsand389stillbirths.
Thisrepresentedastillbirthrateof4.
2/1000birthsandcompareswithnationallyreportedstillbirthratesofnormallyformedsingletonsof3.
9-4.
1/1000overthesameperiod.
26Theanalysisincluded841(0.
9%)repeatpregnanciesduringthetwoyearperiodofthe92218mothersinthecohort.
UnivariateanalysisTable1liststhevariables,groupedaccordingtomaternalandfetalcharacteristics,socialfactors,medicalhistory,andcomplicationsduringpregnancy.
Analysiswasforcompletecasesonly.
Thestillbirthrateispresentedforsubgroups,togetherwithrelativerisksand95%confidenceintervalsinrelationtotherespectivereferencevalues.
Formaternalcharacteristics,stillbirthrateswereincreasedinfirstaswellasthirdandsubsequentpregnanciescomparedwithsecondpregnancies,andinmothersofAfrican,African-Caribbean,andSouthAsianethnicorigincomparedwiththeirEuropeancounterparts.
Firstgenerationmigrantshadanoverallhigherriskofstillbirth.
Maternalageindicatedaslightincreaseinyounger(0.
05inunivariateanalysis),ofclusteringofbirthswithinmaternityunits(seesupplementaryappendices1and2),andofrepeatpregnanciesbythesamemother(resultsnotshown)indicatedonlyminordifferencesinconfidenceintervalsandresultedinnochangesinrelativerisks.
First,third,andhigherorderpregnanciesweresignificantlyassociatedwithstillbirthaswerepregnanciesinAfrican,African-Caribbean,andIndianmothersandfirstgenerationmigrantsfromPakistan.
Obesity(bodymassindex>30),pre-existingdiabetes,historyofmentalhealthproblems,andantepartumhaemorrhageintheindexpregnancywereassociatedwithanincreasedriskofstillbirth.
Interactionsbetweenallvariablesweretestedandwerefoundtobenon-significant,withtheexceptionofastronginteractionbetweensmokingandfetalgrowthrestriction.
Thereforetheresultsarepresentedseparatelyforsmokerswithpregnanciesthatdidordidnothavefetalgrowthrestriction.
Activesmokingwasassociatedwithanincreasedriskofstillbirth(adjustedrelativerisk2.
5,95%confidenceinterval1.
7to3.
6),buttheassociationbecamesubstantiallystronger(5.
7,3.
6to8.
9)forNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page3of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrompregnancieswherethefetuswasalsogrowthrestricted.
Therewasnoassociationbetweenpassivesmokingandstillbirthunlessfetalgrowthrestrictionwasalsopresent,inwhichcasetherelativeriskwasevenhigherthanwithactivesmoking(10.
0,6.
6to15.
8).
Theriskofstillbirthwasincreasedforallpregnancieswithfetalgrowthrestriction,butwashighestwhenthemotherdidnotsmoke(7.
8,5.
6to10.
9).
Table3alsoliststhepopulationattributableriskderivedfromprevalenceandrelativeriskofeachsignificantfactor.
Themodelwasabletoattributeriskfactorsto80.
6%ofthestillbirthsinthiscohort.
Thehighestpopulationattributableriskswereassociatedwithfetalgrowthrestriction,primiparity,andantepartumhaemorrhage.
Inpregnancieswithfetalgrowthrestriction,theadjustedriskofstillbirthwas3.
4(2.
2to5.
2)iffetalgrowthrestrictionwasdetectedantenatally.
Theriskincreasedto6.
5(4.
9to8.
4)iffetalgrowthrestrictionwasnotdetected,and32%ofthestillbirthscouldbeattributedtothisgroup.
Pregnancieswithfetalgrowthrestrictiondetectedantenatallyweredeliveredonaverage10daysearlierthanthosenotdetectedantenatally(table4).
Justoverhalfofthestillbirths(203/389,52%)occurredafter34weeksofgestation.
Table5presentsthesignificantpathologicalfactorsofthemodel,adjustedformaternalcharacteristics,forstillbirthsbeforeandafter34weeksofgestation.
Forstillbirthsbetween24and33weeksofgestation,theonlysignificantfactorwasfetalgrowthrestriction(adjustedrelativerisk4.
0,2.
9to5.
6),whichaccountedforjustunderhalfofthestillbirths(populationattributablerisk49.
5%).
Atthesametime,pre-eclampsiaemergedasasignificantprotectivefactor.
From34weeksofgestation,fetalgrowthrestrictionagainrepresentedthestrongestrisk,andwashighestinpregnancieswherethemotherdidnotsmoke.
DiscussionOurstudyshowsthatwhilethereareseveralriskfactorsforstillbirththatcanbeascertainedfromtheoutsetofpregnancy,thesinglelargestfactorisfetalgrowthrestriction,whichiscurrentlynotwellpredictedandnotrecognisedantenatallyinmostpregnancies.
Consideringthatmostinstancesaremissed,aretrospectivedefinitionoffetalgrowthrestrictionusinggrowthpotential19appliedtobirthweightwasimportanttobeabletoquantifythelinkwithstillbirth.
Thefindingsindicatetheimportanceofimprovingcurrentstrategiesandprotocolsforimprovedsurveillanceoffetalgrowththroughouttheantenatalperiod.
13EarlypregnancyriskfactorsThepopulationbaseddataderivedfromawholeNHSregionallowedustoassessseveralknownaswellasnewriskfactorsthatwillrequirefurtherinvestigationinfuturestudies.
Thesefactorshavevaryingclinicalimplications.
Parity,ethnicity,andpreviousmentalhealthproblemsareindicatorsofriskelicitedatthebeginningofpregnancy.
Theassociationbetweennulliparityandstillbirthreflectsotherreports,14butwealsoobserveda60%increaseinriskformotherswithaparityof3orhigher,suggestingaU-shapedrelationbetweenparityandriskofstillbirth(table2),aspreviouslyreported.
27Contrarytoasystematicreview,28wefoundnosignificantincreaseinriskofstillbirthwitholdermaternalage(table1).
Thismaybebecauseweexcludedcongenitalanomaliesfromourcohort,whichareknowntobeincreasedinoldermothers.
29Thisisconsistentwitharecentreportwhichfoundthattheassociationbetweenstillbirthandmaternalagedisappearswhencongenitalanomaliesareexcluded.
14Motherslivinginthemostdeprivedareashadanincreasedriskofstillbirth,asdidwomenwhowereorhadapartnerwhowasunemployed.
Ethnicorracialdisparitiesinstillbirthrateshavebeenhighlighted1430andwerealsoindependentriskfactorsinourstudy.
Eachofthemainethnicminoritygroupsinourpopulationhadanincreasedriskofstillbirth(table3).
Furtherworkisrequiredtohelpunderstandthereasonsfortheincreasedriskinthesegroups.
Alimitationofourstudyisthatconsentratesforpostmortemexaminationsarelowinsomeethnicgroups,asaresultofwhichsomecaseswithundiagnosedcongenitalanomaliesmayhavebeeninadvertentlyincludedinourcohort.
Amongpre-existingconditions,diabetesisaknownriskfactor31andhadahigherrisk(adjustedrelativerisk3.
9,1.
7to8.
9),butapopulationattributableriskofonly2.
0%becauseofthelowprevalenceinthiscohort.
Ahistoryofmentalhealthproblemswasalsoasignificantriskfactor(adjustedrelativerisk1.
4,1.
0to1.
9),reportedby11.
7%ofmothers.
Ithasbeensuggestedthatthelinkbetweenmentalillnessandadverseoutcomecouldbemediatedthroughgeneralfactorssuchasinsufficientattendanceatantenatalclinicsorunhealthylifestyles.
32Antenatalhaemorrhageincludingplacentalabruptionhasaknownassociationwithstillbirth28;ourresultsconfirmthislinkandemphasisetheneedforimmediate,thoroughinvestigationofanyantepartumbleeding.
Bodymassindexcategoriesof30-34.
9and35ormorerepresenteda40%and60%increasedriskofstillbirth,respectively,andtogetherwereprevalentinjustunder20%ofthiscohort,resultinginapopulationattributableriskof8.
7%.
Contrarytosomereports,14wefoundnoincreaseinriskofstillbirthassociatedwithoverweightmothers(bodymassindex25-29.
9)inourpopulation.
ActiveandpassivesmokingMaternalsmokinginearlypregnancyisassociatedwithstillbirth,withanaverageriskof1.
36basedonfourstudies.
28Wefoundtherisktobehigher(relativerisk1.
8,95%confidenceinterval1.
4to2.
3,table1),possiblyasaresultofhighlevelsofsocialdeprivationinourpopulation,whichisstronglylinkedtosmoking.
33However,thedatabasealsoallowedustoexaminetheinteractionbetweensmokingandfetalgrowth,andtheeffectonstillbirthriskwhenfetalgrowthrestrictionisdetectedantenatally.
Theincreasedriskofsmokingworksmostlythroughfetalgrowthrestriction,andtherateofstillbirthinpregnanciesofmotherswhosmokedbuthadnofetalgrowthrestrictionwassimilar(3.
7)tothatofmotherswhowerenon-smokers(3.
8,table2).
Thishighlightstheimportanceofearlypregnancysmokingcessationprogrammes,whichhavebeenfoundtoreducesmallnessforgestationalageandprematurity.
34Interestingly,thehigheststillbirthratewasinnon-smokingpregnantwomenwithfetalgrowthrestriction,whichcouldbebecausethesepregnanciesareconsideredlowriskandfetalgrowthrestrictionislesslikelytobedetectedantenatally.
Wewerealsoabletoquantifytheeffectofpassiveorenvironmentalsmoking,andfoundittobeassociatedwithanincreaseinriskofstillbirthby30%(table1)—aneffectcorrespondingtothe23%reportedinarecentmetaanalysisoffourtrials.
35Howeverinthemultivariablemodelthisfactorwassignificantonlywhentherewasfetalgrowthrestriction,inwhichcasetheriskevenexceededthatassociatedwiththemotherNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page4of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrombeingasmoker(adjustedrelativerisk10.
0,95%confidenceinterval6.
6to15.
8;table3).
Thisobservationneedsconfirmationinfuturestudiesbutcouldhaveseveralplausibleexplanations.
Passivesmoking,resultingfromthe"sidestream"effectofsmokeproducedbetweenpuffs,hasbeenshowninanimalstudiestobefourtimesastoxicas"mainstream"smoke,36andthismayextendtofetusesduringpregnancy.
Also,thatanon-smokingmotherlivesinasmokingenvironmentmaybemissed,resultinginthepregnancynotbeingaffordedthesameclinicalattention,includingconcernaboutfetalgrowth.
ModifiablefactorsOverall,thelargestpopulationattributablerisk(37.
4%)wasassociatedwithfetalgrowthrestrictionwithandwithoutsmoking,followedbymaternalsmokingwithoutfetalgrowthrestriction(9.
4%)andobesity(bodymassindex≥30;populationattributablerisk8.
7%,table3).
Thesethreevariablescouldbeconsideredasthepotentiallymostmodifiablefactorsand,allowingforoverlap,togetheraccountedfor55.
5%ofstillbirthsinourcohort.
Howevertheyhavedifferentimplicationsforprevention.
Reductionofsmokingandobesityrequireconcertedpublichealtheffortsandeducationprogrammesforwomenofchildbearingage,aswellasthemothers'cooperationwithsmokingcessationprogrammesduringpregnancy.
Theeffectivenessofsuchprogrammesisnotalwaysclear.
Ontheotherhand,theriskofstillbirthasaresultoffetalgrowthrestrictioncanbereducedbyearlyidentificationoftheconditionandreferralforinvestigationsbyultrasoundandDopplerimaging.
12FetalgrowthrestrictionandantenataldetectionTheoveralldetectionrateoffetalgrowthrestrictionwasonly31%,lowerthanthatachievedinourcontrolledstudyinNottinghamusingcustomisedcharts(48%)37andarecentreportfromAustralia(51%).
38However,wefoundthatthedetectionrateinourpopulationrangedwidelybetweenmaternityunits(12.
5-50.
0%),39varyingwiththeamountofstafftrainingandadherencetoprotocols.
Thishighlightstheimportanceofastandardisedandqualityassuredapproachtotheantenatalsurveillanceoffetalgrowthinroutineclinicalpractice.
Amongthecohortof389stillbirths,thedetectionratewasevenlower:195(50.
1%)ofthecaseshadfetalgrowthrestrictionandin160(82.
1%)fetalgrowthrestrictionwasnotdetectedantenatally(table1).
Thepotentialpreventabilityofstillbirthsassociatedwithfetalgrowthrestrictionisillustratedbythereducedriskafterantenataldetection(fig1andtable1).
Althoughpregnancieswithfetalgrowthrestrictionhaveaneighttimeshigherrateofstillbirth(16.
7v2.
1,fig1),thisriskisreducedwhenfetalgrowthrestrictionisdetected(9.
7),althoughnottothesamelevelsasinnon-fetalgrowthrestrictedpregnancies.
Thisislikelytobebecausethebabyisoftennotdeliveredimmediately,eitherduetoinappropriatedelaysorbecauseofconcernsaboutneonatalimmaturity.
Conversely,theriskishigherstilliffetalgrowthrestrictionispresentbutnotdetected.
Theseassociationsarealsoshownwhenallotherfactorsareadjustedforinthemultivariableanalysis(table4):thepopulationattributableriskof32.
0%indicatesthatfivetimesasmanystillbirthsareassociatedwithundetectedantenatalfetalgrowthrestrictionthanwithdetectedfetalgrowthrestriction(6.
2).
Pregnancieswithfetalgrowthrestrictionweredeliveredonaverage10daysearlierthanthosewithout,butstillatrelativelymaturegestationswhendetectedthanwhennot(median270v280days;table4).
Basedontheprevalenceofundetectedfetalgrowthrestriction(9.
2%,table4)andthelowerriskofstillbirthwhenitisdetected(adjustedrelativerisk3.
4),18.
2%or71stillbirthsinourcohortcouldhavebeenavoidedthroughimprovedantenataldetection.
ExtrapolatedtotheUKpopulation,thiswouldrepresent600fewerstillbirthsperyear.
Thesubanalysisofthemultivariablemodelbyearlyandlategestationalagecategories(table5)showedfetalgrowthrestrictionagaintobethestrongestfactorforriskofstillbirthafter34weeksofgestation,withthehighestriskinpregnancieswherethemotherdidnotsmoke.
Before34weeksofgestation,fetalgrowthrestrictionwasthesinglesignificantfactorandaccountedforclosetohalfofallstillbirths(populationattributablerisk49.
5%).
Theseresultssupportthenotionofdifferingpatternsofplacentaldiseaseinearlyandlateonsetfetalgrowthrestriction.
1013Theprotectiveeffectofpre-eclampsia(table5)isinterestingbutnotsurprising:thediseaseisoftenassociatedwithfetalgrowthrestriction,butasthesepregnanciesareoftendeliveredearlyformaternalreasons,thebabyisremovedfromahighriskintrauterineenvironment.
ImplicationsforcliniciansandcommissionersTheincreasedriskofstillbirthafterundetectedfetalgrowthproblemsisconsistentwithanineyearreviewofdeliveriesinasingleunitinMalm40andarecentcase-controlstudyfromAuckland.
41InourdatabasefromalargeNHSregion,wewereabletoquantifytheimportanceofthisriskfactorandestablishitspre-eminentassociationwithstillbirthevenafteradjustmentformedical,social,anddemographicriskfactorsthatcanbeascertainedinearlypregnancy.
Mostcasesoffetalgrowthrestrictiondonotmanifestuntilthethirdtrimesterofpregnancy,andintheabsenceofeffectivescreeningtests,preventionstrategiesneedtoincludeanenhancedlevelofsurveillancethroughoutpregnancy.
Ourfindingssuggestthatearlydetectionoffetalgrowthproblemscansubstantiallyreducetheriskofstillbirth,andneedstobecomeacornerstoneandkeyindicatorofsafetyandeffectivenessinantenatalcare.
Wethankourregionalnetworkofbereavementmidwiveswhosubmitnotificationsonallperinataldeaths;AnnTonks,CatherineFranklin,andRobynCaleywhoruntheregionalperinatalmortalityregistersforensuringhighqualityascertainment;thenetworkofunitbaseddataclerkswhoentertheregionalmaternitydatasetforeachpregnancyonthePEERelectronicrecord(www.
pi.
nhs.
uk/peer);andMichelleSouthamandLorraineEcclestoneforensuringdataqualitythrougharollingprogrammeoftrainingandaccuracyaudits.
Contributors:Allauthorshadfullaccesstothedata,assistedwithitsanalysisandinterpretationoftheresults,andreviewedandapprovedthefinalmanuscript.
JGdevelopedthestudydesign,assistedwiththeanalysisandinterpretation,andwrotethepaper.
Hehasfinalresponsibilitytosubmitforpublication,andistheguarantor.
Funding:DatacollectionandanalyticalstaffwerefinanciallysupportedbyNHSWestMidlandsStrategicHealthAuthorityandallprimarycaretrusts.
Thefundershadnoinfluenceonthestudydesign,analysis,interpretation,writingupofthemanuscript,orthedecisiontosubmitforpublication.
Competinginterests:AllauthorshavecompletedtheICMJEuniformdisclosureformatwww.
icmje.
org/coi_disclosure.
pdf(availableonrequestfromthecorrespondingauthor)anddeclare:nosupportfromanyorganisationforthesubmittedwork;nofinancialrelationshipswithanyorganisationsthatmighthaveaninterestinthesubmittedworkinthepreviousthreeyears,andnootherrelationshipsoractivitiesthatcouldappeartohaveinfluencedthesubmittedwork.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page5of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromWhatisalreadyknownonthistopicStillbirthrateshavechangedlittleintheEnglishNationalHealthServiceoverthepasttwodecadesManyhaveconventionallybeenconsideredunexplainedandunavoidableRiskfactorshavegenerallybeenconsideredweakpredictorsofstillbirthWhatthisstudyaddsMaternalobesity,smoking,andfetalgrowthrestriction,potentiallymodifiableriskfactors,togetheraccountforthemajorityofnormallyformedstillbirthsComparedwithpregnancieswithnormalgrowth,thestillbirthrateinthosewithfetalgrowthrestrictionincreasedfourfold,andincreasedfurthertoeightfoldifgrowthrestrictionwasnotdetectedantenatallyFetalgrowthrestrictioniscurrentlymissedinmostpregnancies,andbetterantenataldetectionneedstobecomeacornerstoneandkeyindicatorofsafetyandeffectivenessinmaternitycareEthicalapproval:Notrequired;datawerecollectedwithpatientconsentandwerepseudonymisedbeforeanalysis.
Datasharing:Noadditionaldataavailable.
1SavingBabiesLivesReport.
StillbirthandNeonatalDeathCharity(SANDS),2009.
2012.
www.
why17.
org/fileadmin/content/About_Sands/03520_Saving_babies_lives_watermarked.
pdf.
2FlenadyV,MiddletonP,SmithGC,DukeW,ErwichJJ,YeeKhongT,etal.
Stillbirths:thewayforwardinhigh-incomecountries.
Lancet2011;377:1703-17.
3OfficeforNationalStatistics(2011).
Deathregistrationsummarytables,England&Wales,2010.
2012.
www.
ons.
gov.
uk/ons/publications/re-reference-tables.
htmledition=tcm%3A77-230730.
4ConfidentialEnquiryintoMaternalandChildHealth(CEMACH).
Perinatalmortality2006:England,WalesandNorthernIreland.
CEMACH,2008.
(Table4.
2).
5GardosiJ.
Clinicalimplicationsof'unexplained'stillbirths.
In:MaternalandChildHealthResearchConsortium,ed:CESDI8thannualreport.
ConfidentialEnquiryintoStillbirthsandDeathsinInfancy,2001:40-7.
6GardosiJ,MulT,MongelliM,FaganD.
Analysisofbirthweightandgestationalageinantepartumstillbirths.
BJOG1998;105:524-30.
7FroenJF,GardosiJ,ThurmannA,FrancisA,Stray-PedersenB.
Restrictedfetalgrowthinsuddenintrauterineunexplaineddeath.
ActaObstetGynecolScand2004;83:81-7.
8GardosiJ,KadySM,McGeownP,FrancisA,TonksA.
Classificationofstillbirthbyrelevantconditionatdeath(ReCoDe):populationbasedcohortstudy.
BMJ2005;331:1113-7.
9VerganiP,CozzolinoS,PozziE,CuttinMS,GrecoM,OrnaghiS,etal.
Identifyingthecausesofstillbirth:acomparisonoffourclassificationsystems.
AmJObstetGynecol2008;199:319.
e1-4.
10KortewegFJGordijnSJ,TimmerA,HolmJP,RaviseJM,ErwichJJ.
Aplacentalcauseofintra-uterinefetaldeathdependsontheperinatalmortalityclassificationsystemused.
Placenta2008;29:71-8.
11StillbirthCollaborativeResearchNetworkWritingGroup.
Causesofdeathamongstillbirths.
JAMA2011;306:2459-68.
12AlfirevicZ,NielsonJP.
Dopplerultrasonographyinhighriskpregnancies:systematicreviewwithmeta-analysis.
AmJObstetGynecol1995;172:1379-87.
13FiguerasF,GardosiJ:Intrauterinegrowthrestriction:newconceptsinantenatalsurveillance,diagnosis,andmanagement.
AmJObstetGynecol2010;doi:10.
1016/j.
ajog.
2010.
08.
05514StillbirthCollaborativeResearchNetworkWritingGroup.
Associationbetweenstillbirthandriskfactorsknownatpregnancyconfirmation.
JAMA2011;306:2469-79.
15KeyHealthDatafortheWestMidlands—2009.
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/pnm.
16PerinatalEpisodeElectronicRecord(PEER).
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/peer.
17Pregnancynotes.
NHSPerinatalInstitute.
2012.
www.
preg.
info.
18WestMidlandsCoreMaternityDatasetv1.
7,2009.
NHSPerinatalInstitute.
2012.
www.
pi.
nhs.
uk/peer/WM_Maternity_Dataset_v1.
7.
pdf.
19GROW(GestationRelatedOptimalWeight)softwareversion6.
5(UK).
GestationNetwork.
2012.
www.
gestation.
net.
20GardosiJ,ChangA,KalyanB,SahotaD,SymondsEM.
Customisedantenatalgrowthcharts.
Lancet1992;339:283-7.
21GardosiJ,MongelliM,WilcoxM,ChangA.
Anadjustablefetalweightstandard.
UltrasoundObstetGynecol1995;6:168-74.
22GardosiJ.
Customisedassessmentoffetalgrowthpotential:implicationsforperinatalcare.
ArchDisChildFetalNeonatalEd2012;doi:10.
1136/fetalneonatal-2012-301708.
23DeJongCL,FrancisA,VanGeijnHP,GardosiJ.
Customizedfetalweightlimitsforantenataldetectionoffetalgrowthrestriction.
UltrasoundObstetGynecol2000;15:36-40.
24GenestDR,WilliamsMA,GreeneMF.
Estimatingthetimeofdeathinstillbornfetuses:I.
Histologicevaluationoffetalorgans;anautopsystudyof150stillborns.
ObstetGynecol1992;80:575-84.
25KooperbergC,PetittiDB.
Usinglogisticregressiontoestimatetheadjustedattributableriskoflowbirthweightinanunmatchedcase-controlstudy.
Epidemiology1991;2:363-6.
26ConfidentialEnquiryintoMaternalandChildHealth.
Perinatalmortality2007.
CEMACH,2009:21.
27BaiJ,WongFW,BaumanA,MohsinM.
Parityandpregnancyoutcomes.
AmJObstetGynecol2002;186:274-8.
28FlenadyV,KoopmansL,MiddletonP,FrenF,SmithGC,GibbonsK,etal.
Majorriskfactorsforstillbirthinhigh-incomecountries:asystematicreviewandmeta-analysis.
Lancet2011;377:1331-40.
29HollierLM,LevenoKJ,KellyMA,McIntireDD,CunninghamFG.
Maternalageandmalformationsinsingletonbirths.
ObstetGynecol2000;96:701-6.
30ReeskeA,KutschmannM,RazumO,SpallekJ.
Stillbirthdifferencesaccordingtoregionsoforigin:ananalysisoftheGermanperinataldatabase,2004-2007.
BMCPregnancyChildbirth2011;11:63.
31PerssonM,NormanM,HansonU.
Obstetricandperinataloutcomesintype1diabeticpregnancies:alarge,population-basedstudy.
DiabetesCare2009;32:2005-9.
32King-HeleS,WebbRT,MortensenPB,ApplebyL,PicklesA,AbelKM.
Riskofstillbirthandneonataldeathlinkedwithmaternalmentalillness:anationalKing-Helecohortstudy.
ArchDisChildFetalNeonatalEd.
2009;94:F105-10.
33GoyaJ,DoddL,RosenbergMWKingaWDHealth-riskbehaviours:examiningsocialdisparitiesintheoccurrenceofstillbirthPaediatrPerinatalEpidemiol2008;22:314-20.
34McCowanLM,DekkerGA,ChanE,StewartA,ChappellLC,HunterM,etal.
Spontaneouspretermbirthandsmallforgestationalageinfantsinwomenwhostopsmokingearlyinpregnancy:prospectivecohortstudy.
BMJ2009;26;338:b1081.
Erratumin:BMJ2009;338.
doi:10.
1136/bmj.
b1558.
35Leonardi-BeeJ,BrittonJ,VennA.
Secondhandsmokeandadversefetaloutcomesinnonsmokingpregnantwomen:ameta-analysis.
Pediatrics2011;127:734-41.
36SchickS,GlantzS.
PhilipMorristoxicologicalexperimentswithfreshsidestreamsmoke:moretoxicthanmainstreamsmoke.
TobControl2005;14:396-404.
37GardosiJ,FrancisA.
Controlledtrialoffundalheightmeasurementplottedoncustomisedantenatalgrowthcharts.
BJOG1999;106:309-17.
38RoexA,NikpoorP,vanEerdE,HodylN,DekkerG.
Serialplottingoncustomisedfundalheightchartsresultsindoublingoftheantenataldetectionofsmallforgestationalagefetusesinnulliparouswomen.
AustNZJObstetGynaecol2012;52:78-82.
doi:10.
1111/j.
1479-828X.
2011.
01408.
x.
39WestMidlandsPerinatalKPIReport,Q22010/11.
PerinatalInstitute,2011.
2012.
www.
pi.
nhs.
uk/pnm/maternitydata/Q2_2010-11_Perinatal_KPI_report.
pdf.
40LindqvistPG,MolinJ.
Doesantenatalidentificationofsmall-for-gestationalagefetusessignificantlyimprovetheiroutcomeUltrasoundObstetGynecol2005;25:258-64.
41StaceyT,ThompsonJM,MitchellEA,ZuccolloJM,EkeromaAJ,McCowanLM.
Antenatalcare,identificationofsuboptimalfetalgrowthandriskoflatestillbirth:findingsfromtheAucklandStillbirthStudy.
AustNZJObstetGynaecol2012.
doi:10.
1111/j.
1479-828X.
2011.
01406.
Accepted:18December2012Citethisas:BMJ2013;346:f108Thisisanopen-accessarticledistributedunderthetermsoftheCreativeCommonsAttributionNon-commercialLicense,whichpermitsuse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited,theuseisnoncommercialandisotherwiseincompliancewiththelicense.
See:http://creativecommons.
org/licenses/by-nc/2.
0/andhttp://creativecommons.
org/licenses/by-nc/2.
0/legalcode.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page6of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTablesTable1|UnivariateanalysisofriskfactorsassociatedwithstillbirthscomparedwithlivebirthsRelativerisk(95%CI)Rate/1000birthsNo(%)ofstillbirthsNo(%)ofallbirthsRiskfactors—4.
2389(100)92218(100)TotalGeneralmaternalcharacteristicsn=389n=92208Age(years):1.
3(0.
9to1.
9)5.
133(8.
5)6456(7.
0)90n=380n=88053Fetalgrowthrestriction:Reference2.
4185(48.
7)76356(86.
7)NoYes4.
0(2.
8to5.
7)9.
735(9.
2)3601(4.
1)Detectedantenatally8.
0(6.
5to9.
9)19.
8160(42.
1)8096(9.
2)Notdetectedantenatally*Placeofbirthcombinedifeithersubgroup<1000women.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page9of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable2|Smokingandfetalgrowthrestriction(birthweight<10thgestationrelatedoptimalweightcentile)Stillbirthrate/1000birthsProportionoftotal(%)Variables4.
2100.
0All5.
818.
7Smokers:13.
04.
3Fetalgrowthrestriction3.
713.
7Nofetalgrowthrestriction3.
881.
3Non-smokers:18.
38.
3Fetalgrowthrestriction2.
168.
7NofetalgrowthrestrictionNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page10of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable3|Multivariableanalysisofsignificant(P<0.
1)riskfactorsintable1Populationattributablerisk(%)Prevalence(%)PvalueAdjustedrelativerisk(95%CI)VariablesParity:21.
343.
4<0.
011.
8(1.
3to2.
5)04.
69.
40.
051.
6(1.
0to2.
5)≥3Ethnicorigin,placeofbirth:2.
93.
00.
012.
4(1.
2to4.
6)African*2.
22.
00.
012.
3(1.
3to4.
1)African-Caribbean*3.
95.
2<0.
012.
1(1.
3to3.
5)Indian*6.
44.
6<0.
013.
0(1.
9to4.
8)Pakistani,non-UKBodymassindex:4.
512.
50.
071.
4(1.
0to2.
0)30-34.
94.
27.
30.
031.
6(1.
1to2.
4)≥354.
711.
70.
061.
4(1.
0to1.
9)Mentalhealthhistory2.
00.
7<0.
013.
9(1.
7to8.
9)Pre-existingdiabetes15.
58.
1<0.
013.
4(2.
6to4.
5)AntepartumhaemorrhageMaternalsmoking,nofetalgrowthrestriction9.
414.
9<0.
012.
5(1.
7to3.
6)Activesmoker—15.
70.
281.
3(0.
8to2.
0)PassivesmokerMaternalsmoking,fetalgrowthrestriction:6.
14.
6<0.
015.
7(3.
6to8.
9)Activesmoker9.
12.
1<0.
0110.
0(6.
6to15.
8)Passivesmoker22.
26.
5<0.
017.
8(5.
6to10.
9)Fetalgrowthrestriction,non-smokerReferencegroup:para1,UKborn,non-smokingEuropeanmother;bodymassindex18.
5-24.
9.
*UKandnon-UKgroupscombinedbecauseofsmallnumbers.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page11of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable4|Gestationalageatdeliveryandriskofstillbirthsinpregnancieswithfetalgrowthrestriction*,withandwithoutantenataldetectionPopulationattributablerisk(%)PvalueAdjustedrelativerisk(95%CI)Median(interquartilerange)gestationalageatdelivery(days)Prevalence(%)VariablesReference280(273-286)86.
8NofetalgrowthrestrictionFetalgrowthrestriction:6.
2<0.
013.
4(2.
2to5.
2)270(261-279)4.
0Detectedantenatally32.
0<0.
016.
5(4.
9to8.
4)280(273-287)9.
2Notdetectedantenatally*Adjustedforethnicity,parity,bodymassindex,pre-eclampsia,antepartumhaemorrhage,historyofmentalhealthproblems,andsmoking.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page12of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromTable5|Fetalgrowthrestrictionandotherpathologicalfactorsbeforeandafter34weeksofgestationPopulationattributablerisk(%)Prevalence(%)PvalueAdjustedrelativerisk*(95%CI)Variables24-33weeks13.
210.
5<0.
010.
3(0.
1to0.
6)Pre-eclampsia49.
514.
3<0.
014.
0(2.
9to5.
6)Fetalgrowthrestriction≥34weeksBodymassindex:9.
912.
0<0.
011.
9(1.
3to3.
0)30-345.
17.
30.
021.
8(1.
1to3.
0)≥357.
611.
30.
041.
7(1.
0to2.
7)Mentalhealthhistory9.
116.
60.
011.
6(1.
1to2.
3)Latebooking13.
07.
5<0.
013.
1(2.
0to4.
7)Antepartumhaemorrhage7.
314.
10.
021.
7(1.
1to2.
7)Smoker,nofetalgrowthrestriction2.
54.
30.
012.
5(1.
3to5.
1)Smoker,fetalgrowthrestriction22.
78.
0<0.
015.
1(3.
4to7.
6)Fetalgrowthrestriction,non-smoker*Adjustedforethnicity,maternalage,parity,andbodymassindex.
Birthweight<10thgestationrelatedoptimalweightcentile.
Nocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page13of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
DownloadedfromFiguresFig1StillbirthratesinrelationtofetalgrowthrestrictionandwhetheritwasdetectedantenatallyFig2Stillbirthsandlivebirthswithandwithoutfetalgrowthrestriction:cumulativepercentagegraphofgestationalageatdeliveryNocommercialreuse:Seerightsandreprintshttp://www.
bmj.
com/permissionsSubscribe:http://www.
bmj.
com/subscribeBMJ2013;346:f108doi:10.
1136/bmj.
f108(Published24January2013)Page14of14RESEARCHon3April2021byguest.
Protectedbycopyright.
http://www.
bmj.
com/BMJ:firstpublishedas10.
1136/bmj.
f108on24January2013.
Downloadedfrom
- enteredjp.ady9.info相关文档
- Millionsjp.ady9.info
- Reasonsjp.ady9.info
- treasuryjp.ady9.info
- zastpowaniajp.ady9.info
- basedjp.ady9.info
- Itajp.ady9.info
Megalayer新加坡服务器国际带宽线路测评
前几天有关注到Megalayer云服务器提供商有打算在月底的时候新增新加坡机房,这个是继美国、中国香港、菲律宾之外的第四个机房。也有工单询问到官方,新加坡机房有包括CN2国内优化线路和国际带宽,CN2优化线路应该是和菲律宾差不多的。如果我们追求速度和稳定性的中文业务,建议还是选择CN2优化带宽的香港服务器。这里有要到Megalayer新加坡服务器国际带宽的测试服务器,E3-1230配置20M国际带...
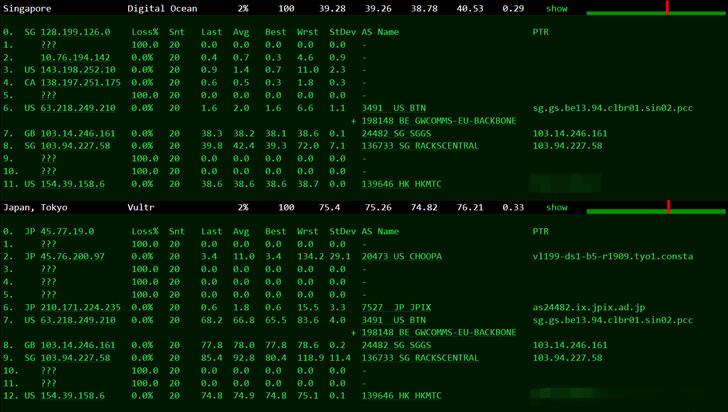
VirMach:$27.3/月-E3-1240v1/16GB/1TB/10TB/洛杉矶等多机房
上次部落分享过VirMach提供的End of Life Plans系列的VPS主机,最近他们又发布了DEDICATED MIGRATION SPECIALS产品,并提供6.5-7.5折优惠码,优惠后最低每月27.3美元起。同样的这些机器现在订购,将在2021年9月30日至2022年4月30日之间迁移,目前这些等待迁移机器可以在洛杉矶、达拉斯、亚特兰大、纽约、芝加哥等5个地区机房开设,未来迁移的时...

2021年7月最新洛杉矶CN2/香港CN2 vps套餐及搬瓦工优惠码 循环终身优惠6.58%
搬瓦工怎么样?2021年7月最新vps套餐推荐及搬瓦工优惠码整理,搬瓦工优惠码可以在购买的时候获取一些优惠,一般来说力度都在 6% 左右。本文整理一下 2021 年 7 月最新的搬瓦工优惠码,目前折扣力度最大是 6.58%,并且是循环折扣,续费有效,可以一直享受优惠价格续费的。搬瓦工优惠码基本上可能每年才会更新一次,大家可以收藏本文,会保持搬瓦工最新优惠码更新的。点击进入:搬瓦工最新官方网站搬瓦工...

jp.ady9.info为你推荐
-
酒店回应名媛拼单酒店分房时出现单男单女时,怎样处理?中老铁路中长铁路的铁路的新中国历史梦之队官网梦之队是什么呢?是那个国家的呢?他们又是参加那个项目的呢?得了几块金牌呢?嘀动网动网和爱动网各自的优势是什么?钟神发跪求钟神发名言出处,A站大神看过来同ip网站12306怎么那么多同IP网站啊?这么重要的一个网站我感觉应该是超强配置的独立服务器才对啊,求高人指点同一ip网站同一个IP不同的30个网站,是不是在一个服务器上呢?336.com求那个网站 你懂得 1552517773@qqwww.765.com哪里有免费的电影网站百度指数词什么是百度指数